ORIGINAL RESEARCH
Urban violence and effect on care practices in family health strategy territories
Cynthia Braz MachadoI, Donizete Vago DaherII, Enéas Rangel TeixeiraIII, Sonia AcioliIV
I
Nurse. Master in Nursing, Fluminense Federal University. Niterói, Rio de
Janeiro, Brazil. E-mail: cynthiabraz@yahoo.com.br
II
Nurse. Ph.D. in Collective Health. Associate Professor, Fluminense Federal
University. Niterói, Rio de Janeiro, Brazil. E-mail: donizete@predialnet.com.br
III
Nurse. Ph.D. in Nursing. Professor, Fluminense Federal University. Niterói
, Rio de Janeiro, Brazil. E-mail: eneaspsi@hotmail.com
IV
Nurse. Ph.D. in Collective Health. Assistant Professor, University of Rio
de Janeiro State. Brazil. E-mail: soacioli@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.25458
ABSTRACT
Objective: to identify the effect of urban violence on nursing care practices, nursing technicians and community health workers in areas covered by the family health strategy in Niterói, a municipality of Janeiro State of Rio. Methodology: in this descriptive case study, data were collected in the third quarter of 2014 by semi-structured interviews of eleven professionals at two family health facilities. Transcripts were analyzed by content analysis. Results: personnel perceived urban violence as adverse and compromising their care actions, especially when activities are carried out outside the facilities. Conclusion: there is a need for inter-sector discussion of the problem, so that the strategies developed address the problem effectively.
Keywords: Violence; family health; primary health care; nursing.
INTRODUCTION
Nowadays, modern societies coexist daily with the phenomenon of urban violence. This has been presented as one of the great social challenges and portrayed in different ways in television and print media. They seem to compose the living of the great urban centers: homicides, armed conflicts, robberies, kidnappings, rapes, restriction of the coming and going of individuals, among others. All these events have gradually become part of the social network and have been culturally naturalized as another event of the daily life of social groups.
The growth of violence rates and concern with this phenomenon affect several segments of different societies, and therefore, it is not restricted to Brazil. Its diversity, magnitude, incidence, and prevalence have reflected on public health, both as a major cause of health and life-threatening impairment, as well as in the provision of services in more vulnerable territories1.
Health professionals and basic health care services (ABS) located in the belts of large cities face daily urban and social violence events, as they work in communities, where high trafficking levels of unemployment, low education, poverty and social isolation are part of daily life and increase the likelihood of violence situations2. Thus, health spaces, professionals, and the community live in constant situations of vulnerability feeding violence.
The confrontation of the phenomenon of violence by professionals and health services is recent, and the new ways of dealing with this event are not yet incorporated into the daily practices of services. At times, when confronted with violence, these professionals have difficulties in facing it. The ability to work with these complex scenarios and their unexpected events is not offered in the professional training nor foreseen by the managers. They live in situations that generate outrage, frustrations and frequent turnover in team composition.
Given the above, the study aimed to identify the repercussion of urban violence on the nursing care practices, nursing technicians and community health agents (ACS) that work in areas of family health coverage, in a municipality of the Metropolitan Region II do Rio de Janeiro state.
LITERATURE REVIEW
Due to its eminently social origin, violence has always been part of society and, depending on the historical, social and cultural context of a place, its forms of expression and understanding are distinct3. Therefore, actions that in one society are characterized as violent, in others they are natural.
Violence consists of individual human acts, groups, classes and even nations that lead to the death of other human beings or compromise their physical, mental, spiritual and moral integrity4. Violence, besides compromising the physical structure of the individual, also affects the mind, the spiritual and emotional state, and this commitment is often not identified or perceived by others.
According to an analysis of the phenomenon of violence carried out by the German philosopher Hanna Arendt, violence has always played an important role in human affairs, a fact that has led it to be trivialized and even disregarded by society.
No one who has been thinking about history and politics can remain oblivious to the enormous role that violence has always played in human affairs, and at first sight, it is surprising that violence has rarely been chosen as an object of special consideration. [...] This indicates how violence and its arbitrariness were considered commonplace and, therefore, disregarded5:16.
Currently, the following characteristics of violence prevail in the country: the profit objective, the relationship between legal and illegal and associated organizations, related to the increasing number of murders and high crime rates3.
Thus, urban violence articulates a complex of practices having most of the social conflicts in large cities. For this, it uses aggressive means to threaten the physical and patrimonial integrity of the people. In this way, it is a form of expression that produces practical-moral understanding daily in the cities of the country6.
METHODOLOGY
The research adopted the descriptive method of the case study type. Two families´ health units were included in the scenario, from a municipality in the Metropolitan Region II of the State of Rio de Janeiro. These units develop their care practices with two health teams. The participants were three nurses, four nursing technicians, and four ACS, totaling 11 professionals, whose election was based on the following inclusion criteria: being part of the team of family health professionals, and agreeing to participate freely in the research, signing the Free and Clarified Consent Term. The exclusion criteria were: professionals with less than six months of service in the unit and who for some reason were away from the service, during the period of field work, from August to October 2014.
The semi-structured interview was chosen for the data collection, through open questions, favoring the interviewee to freely discuss the proposed topic, without being confined only to the question asked. The interviews were conducted in an appropriate room of the unit and were recorded using a digital recorder. The participants were identified with the letter E for the nurse, TE for the nursing technician and ACS for community health agent to preserve the identity of the interviewees, with the number corresponding to the sequence of the interview and according to the professional category.
The content analysis proposed by Bardin was used for the data treatment, considering the three recommended steps: pre-analysis, material exploration and treatment of results obtained and interpretation7.
The ethical precepts contained in Resolution 466 of December 12, 2012, were met, and the project was approved by the Ethics and Research Committee of the Antonio Pedro University Hospital of the Fluminense Federal University under number 893.308/2014.
RESULTS AND DISCUSSION
Characterization of the participants
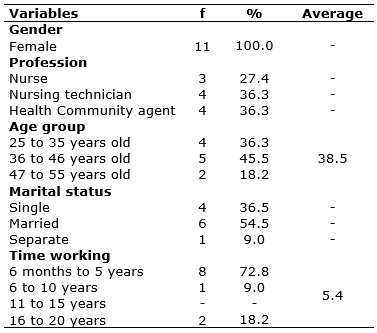
All participants in the survey are female, according to Table 1. This fact can be understood by the expansion and increase in levels of education as well as the reduction of fertility rates, which have driven women to the paid labor market8.
TABLE 1: Characterization of the research participants. Rio de Ja neiro, 2014.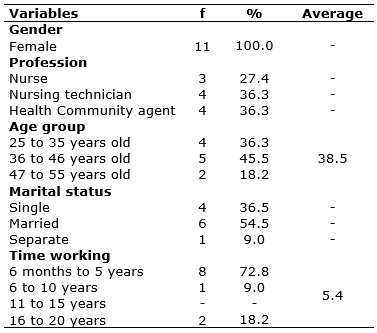
Only women were found in the scenario investigated, an approximate result of the literature, which reveals to be the feminization process of the health professions a Brazilian tendency, and therefore, of the workers of the family health teams, subjects of this study9.
The average age is 38.5 years old, ranging from 27 to 51 years old, corresponding to the productive age range of these subjects. A similar result was found in a study carried out in the State of Rio Grande do Sul, in which the profile of professionals working in family health was studied, whose average age reached 37.3 years old10.
Regarding the marital status, more than half of the participants were married. This data may be associated with the age of the respondent professionals, who are in the adult phase, considering the cycle of human development, which, in general, predisposes to the constitution of family nuclei. This was a convergence data found in a survey carried out in municipalities in the interior of São Paulo, where it was found that more than half (66%) of the participants in the ESF were married11.
The time working on the unit ranged from 6 months to 19.9 years, with an average of 5.4 years. In this finding, it is expected that the greater the time of the unit, the greater the knowledge regarding the territory, the population, the health needs of the population and the potentialities of the residents of the community, the formation of bond and longitudinally of care12.
Categories of the studies
The content analysis of the testimonies generated two categories interpreted below.
Perceptions of professionals in the urban violence in the territory
It was remarkable the relation observed by the participants between urban violence and crime in the territories surveyed.
Among the violent events reported, there were gun shots and police interventions such as the predominant, which have long interfered with citizens´ lives and the provision of care for professionals working in the ABS. Participants report that access to health services such as vaccinations, drug searches and consultations are often delayed due to violence in the territory.
It is worth emphasizing that violence is used for the conquest and maintenance of power. However, whoever thinks that violence is a form of power is extremely deceived, on the contrary, it demonstrates the incapacity of argumentation, change, and convincing individuals5 .
The violence experienced by health professionals is related to the fact that the family health services, at the time of their implementation by the Health Secretariats, have privileged areas of greater social risk, with the formulation of strategies that would enable close contact among health professionals, families and community, whether in open-door care or the patients´ homes. These factors determined the increase in the vulnerability of the worker13, as confirmed by the statements:
There were some situations when we were in the area and started the shooting, or running back to the health center or entering a patient´s home. (ACS1)
A striking fact was the shot taken in the dressing room, here on the side. I think it was something that frightened the team, which made everyone fearful... Also, we have the traffic here in the unit. Something that whether or not, we are afraid to respond, to deal with, how to speak, how to receive. Nobody from the management sees this... So, [...] they are worrying factors. (E2)
Health professionals are exposed in the work scenarios to indirect violence that can result from living together, interacting and witnessing situations of external violence, which means having face-to-face or indirect contact with victims of violence or with aggressors13.
Police teams are also repeatedly mentioned by the insecurity they generate with their presence and ways of acting in the territories. The professionals analyze in a very critical way the police incursions that generate much more insecurity, as evidenced in the speeches:
There was a period, at the beginning of the year, that we needed to close the unit completely. Because there were shots all the time, it was an entrance to a cave, etc. They do not care about anything; it was just shot [...]. Yesterday, for example, there was a rifle shot down there. It has happened that I was in the patient´s house, collecting blood, and having to hurry back because everyone was armed in the street. So, this situation is quite routine here, in this place. (E3)
Police conflicts with people in the community are what most people have here. A cave is coming in, giving shot [...], cops, here, at the door. (TE4)
It can be noticed that the presence of the police in the community, with the so-called cave, generates a lot of fear and despair in professionals, who feel alone in times of greater tension. This violence is also reported as a local power dispute. Thus, professionals experience and suffer direct and indirect violence, as they are also witnesses to the reports of the suffering of the residents of the community in which they work.
It is necessary not only the knowledge of the facts to understand the phenomenon of violence, but also the representations they have of it. In this way, it must be considered how individuals perceive it in their realities and contexts. Violence can be experienced differently in different social classes, ages, genders, and races14.
The repercussion of violence on health care practices was evidenced in the statements:
[...] it is very bad because I know that in some situations it prevents us from doing the care practices. We even lost vaccines, because they cut off electricity... many remarked consultations, etc. (E1)
Violence is discouraging. Because we have to go to the patient´s house, there is shot, there is police, and you cannot go. We could not develop the work as we would like. (ACS1)
The different social groups of large cities have lived under pressure and fear. The increase in rates of urban violence, in its most diverse forms, has contributed to a social perspective based on individualism, distrust, and distancing between people. Thus, urban violence situations in the communities can impact the work of the ESF teams, because they are inserted in the environment where they work, with a wide community participation, and get to know families and risk groups15.
Through the set of testimonies, it is observed that all participants see violence as a negative, discouraging, limiting of care practices and producing weaknesses of patients and health professionals. Therefore, it is an event that compromises the demand and the adherence of patients to the services.
The professionals' perceptions agree with the thinking defended by Hannah Arendt that there is no positivity in violence5. The philosopher contrasts with other thinkers who have a view that violence can be justified since it is in the service of a social or individual transformation3.
It is a bad part, a very negative part of violence because it disrupts everything. Sometimes our work stands still and for the patients too, because many of them live with this violence on the doorstep. We [ACS and nursing technicians] that we are also residents, we pass this on the professional and personal part. Thus, there are days that are very negative and influence the health of the patient, too. A person who is hypertensive can go wrong because of it. (ACS2)
I think this is a lack of organization of the authorities. In fact, you have the police, and you have the parallel power, which seems to live in symbiosis [...]. Because it comes in, it makes noise, it shoots, but nothing is solved, it is still there, the same way... violence is continuing. So, you need to look different from the authorities for this violence issue. (E3)
Given the complexity and multi-causality of violence, there is a diversity of representations about it, hindering to characterize it from a single point of view. To understand violence, in its most diverse expressions of contemporary society, it is necessary, first, to analyze interpersonal relations that are permeated by power, and which go beyond social classes, genders, ethnicities, and cultures, which are the structuring axes of social processes16.
When reporting that the violence in the territories is motivated by the disengagement with the social reigning in these scenarios, the police institution appears as the possibility of social reorganization. However, the modus operandi of it strengthens the violence daily.
Professional care practices and limitations imposed by urban violence
The professionals who work in the family health teams, developing intramural and extramural actions, end up experiencing urban violence in their territories. When asked about the difficulties in their care practices, they reported that urban violence has been responsible for limiting their actions, since, in addition to hindering home visits, it often makes activities such as educational groups, scheduled consultations and other actions aimed at health promotion and disease prevention. In this sense, violence generates gaps in the care process, resulting in feelings of frustration.
We schedule an action, sometimes for months, to set up a tent for educational practices in the community and we cannot carry out due to violence. It impacts yes because it makes our work difficult and everything that we programmed frustrating the team and interfering even in their emotional, because they have family in here. So, it impacts on various fields of our day to day. (E2)
It impacts when there is a police operation because it makes it impossible for us to go to the countryside, to visit, to be exposed to violence and at risk of life. (TE3)
The central proposal of family health is to have the individual as a participant in the health-disease process, through individual and collective actions, in their physical and social environment. However, this focus becomes complex when the main challenge of the team is to redirect the practices in a context of urban violence, in its territory, a serious social problem that has been limiting their development17.
The statements showed the magnitude of the events, the interference in the dynamics of the units´ functioning, causing, for example, several cancellations of previously scheduled activities until the situation is controlled by the community and the fear and tension of the professionals return to the tolerable limit in day to day.
We found difficulties, several. You are organizing a group, and you know that no one is going to come down because strange people have arrived in the community, it is a consultation missing. Several times it has already messed up, but it does not stop. If that is why we will not do anything. If the police come in, we will not go up? You have to mediate this. Climbing them always go up. The question is if it has already limited.... (E3)
Violence does not let us do much. If you get a bad week, with police firing in there, it is complicated. With that, we spent a week working only internally. (ACS3)
When leaving the unit to carry out home visits, professionals are more exposed to community routines. These visits have been considered a risk factor in the work by the professionals since the security feeling of the physical structure of the unit is broken15. Also in the research scenarios, visits are suspended when there is a shootout and conflicts between police officers and possible drug traffickers because professionals are even more exposed to violence when they are in the area.
[...] violence is an obstacle for health professionals who work in primary care, especially in the ESF, given the characteristic of being provided in the community, at home, exposing professionals to violent environments. This vulnerability to violence generates feelings of fear, anxiety, impotence and frustration, compromising their physical and mental health. Violence causes the work in the ESF to be discharged because when it is limited to attending more of the health units, the community service is impaired18:938.
Based on the findings, the vulnerability to which these professionals are exposed in the work routine is clear, especially in practices outside the walls. Faced with these situations, the work process of these units, in part, is decided by the conditions of the environment in the territory. In the case of extreme situations of manifestation of violence, such as shootings, the home visits are suspended, leaving in the background assistance to patients, for protection, safety, and survival of the professional.
It has already happened to have home visits scheduled, with curative, injectable medications and cannot go. Thank God, the patient ends up understanding that we cannot go there. (TE2)
Because from the moment of the first shot, we no longer have how to walk through the community. [...] Then, it is impracticable to walk in the places in search of the patients, if someone goes awry he has to wait for the movement to improve and the police leave to be able to later, to act something. (ACS3)
The testimonies make clear that activities in the territory are often compromised due to urban violence, and since this involves different social issues, its confrontation becomes complex. In this way, it has contributed to the increasing mischaracterization of family health care practices, concentrating the work process inside the units.
CONCLUSIONS
Urban violence is a concrete reality in the territory of the communities where the family health units are located, these research scenarios. It was evidenced that it affects care practices, and this reality is like other large urban centers, as seen in the literature accessed for this research.
Urban violence takes place in these spaces mainly through intense shootings and conflicts between police and traffickers. The set of statements indicates that this violence has different repercussions on care practices so that health units offer actions according to the daily conditions of each territory. Regarding the patients, the participants reported that they experience limitations of access to the health service, with the commitment to adherence and continuity of care.
The different external activities, such as home visits and educational practices, are those directly committed to the phenomenon of urban violence in the territory studied, mischaracterizing the proposal advocated for family health. Internal activities, such as consultations, vaccination, among others, also compromised by both the violence that limits access and by the overlapping of activities within the units. Thus, access is conditioned by external factors such as violence in the community.
There is evidence of the need for training of health professionals to deal with violence in these scenarios, as well as the creation of spaces for discussion on these events in partnership with managers, residents´ association, civil society and other sectors such as education and Justice, so collectively, in an intersectoral and interdisciplinary way, effective strategies can be built to confront urban violence in these territories.
REFERENCES
1.Teles LAL. Significados da violência: reflexões sobre as práticas escolares [dissertação de mestrado]. Salvador (BA): Universidade Federal da Bahia; 2013.
2.Rückert TR, Lima MADS, Marques GQ, Garlet ER, Pereira WAP, Acosta AM. Assistência em unidades básicas de saúde às vítimas de violência na concepção de enfermeiras. Ciênc Cuid Saúde. 2008; 7(2): 180-6.
3.Minayo MCS. Violência e saúde. Rio de Janeiro: Fiocruz; 2006.
4.Minayo MCS, Souza ER. Violência e saúde como um campo interdisciplinar e de ação coletiva. Hist cienc saúde -Manguinhos. 1997; 4(3): 513-31.
5.Arendt H. Sobre a violência. Rio de Janeiro: Relume-Dumará; 1994.
6.Silva LAM. Violência urbana, segurança pública e favelas: o caso do Rio de Janeiro atual. Cad CRH. 2010; 23(59): 283-300.
7.Bardin L. Análise de conteúdo. São Paulo: Edições 70; 2011.
8.Pinto ESG, Menezes RMP, Villa TCS. Situação de trabalho dos profissionais da Estratégia Saúde da Família em Ceará-Mirim. Rev esc enferm USP. 2010; 44(3): 657-64.
9.Costa SM, Prado MCM, Andrade TN, Araújo EPP, Silva Junior WS, Gomes Filho ZC, et al. Perfil do profissional de nível superior nas equipes da estratégia saúde da família em Montes Claros, Minas Gerais, Brasil. Revista Brasileira de Medicina de Família e Comunidade. 2013; 8 (27): 90-6.
10.Zanetti TG, Sand ICPV, Girardon-Perlini NMO, Kopf AW, Abreu PB. Perfil socioprofissional e formação de profissionais de equipes de saúde da família: um estudo de caso. Ciência, Cuidado e Saúde. 2011; 9(3): 448-55.
11.Camelo SHH, Angerami ELS. Formação de recursos humanos para a estratégia de saúde da família. Ciência, Cuidado e Saúde. 2008; 7(1): 45-52.
12.Ministério da Saúde(Br). Política Nacional de Atenção Básica a Saúde. Brasília (DF): Ministério da Saúde; 2012.
13.Lancman S, Ghirardi MIG, Castro ED, Tuacek TA. Repercussões da violência na saúde mental de trabalhadores do Programa Saúde da Família. Rev Saúde Pública. 2009; 43(4): 682-8.
14.Almeida ANN, Campos CCA, Santos LIC, Paiva IL. Juventude e violência: o que pensam os jovens de um projovem urbano em Natal/RN. Temas psicol. 2014; 22(4): 853-69.
15.Velloso ISC, Araujo MT, Rocha AM, Alves M. A visão dos profissionais de saúde sobre a violência no cotidiano de trabalho em uma unidade básica. Rev Min Enf. 2005; 9(4): 302-8.
16.Lopes RE, Adorno RCF, Malfitano APS, Takeiti BA, Silva CR, Borba PLO. Juventude pobre, violência e cidadania. Saude soc. 2008; 17(3): 63-76.
17.Polaro SHI, Gonçalves LHT, Alvarez AM. Enfermeiras desafiando a violência no âmbito de atuação da estratégia de saúde da família. Texto contexto - enferm. 2013; 22(4): 95-42.
18.Ayres RCM, França Junior I, Calazans GJ, Saletti Filho HC. O conceito de vulnerabilidade e as práticas de saúde: novas perspectivas e desafios. In: Czeresnia D, Freitas CM. Promoção da saúde: conceitos e tendências. Rio de Janeiro: Fiocruz; 2003. p.121-44.