ORIGINAL RESEARCH
Blood loss and signs or symptoms during puerperal assessment: implications for nursing care
Mariana Torreglosa RuizI; Natália Alves ParaisoII ; Ana Rita Marinho MachadoIII; Maria Beatriz Guimarães FerreiraIV; Anneliese Domingues WysockiV; Marli Villela MamedeVI
I
Ph.D. Federal University of the Triângulo Mineiro, Undergraduate Nursing
Course. Uberaba, Minas Gerais, Brazil. Email :
marianatorreglosa@hotmail.com
II
Nurse. Federal University of Triângulo Mineiro, Uberaba, Minas Gerais,
Brazil. E-mail: nat_paraiso@hotmail.com
III
Ph.D. Federal University of the Triângulo Mineiro, Undergraduate Nursing
Course. Uberaba, Minas Gerais, Brazil. E-mail: anarita@mednet.com.br
IV
Ph.D. University of Uberaba, Undergraduate Nursing and Medicine courses.
Uberaba, Minas Gerais, Brazil. E-mail: mariabgfo@gmail.com
V
Ph.D. Federal University of Mato Grosso do Sul, Undergraduate Nursing
Course. Três Lagoas, Mato Grosso do Sul, Brazil. E-mail: lilisew@yahoo.com.br
VI
Ph.D. University of São Paulo, Nursing School of Ribeirão Preto. São Paulo,
Brazil. E-mail: mavima@eerp.usp.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.22756
ABSTRACT
Objective: to relate blood loss with complaints, signs or symptoms of blood disorders in the postpartum period, by measuring hemoglobin (Hb) and hematocrit (Ht) levels. Method: epidemiological cross-sectional study of 100 primiparas at a São Paulo teaching hospital, from August to December, 2012. Information from antenatal and hospital records were analyzed and Hb and Ht dosed, at mother's admission and 48 hours postpartum. The study was approved by São Paulo University research ethics committee (HCRP No. 4172/2011) Results: women with greater blood loss showed statistical differences in mucous membrane pallor and symptomatic complaints (weakness, fatigue, depression and/or apathy). Hypotension and tachycardia showed no association with decreased hematocrit. Conclusion: quality nursing care can contribute to reducing maternal morbidity and mortality in cases of postpartum hemorrhage, by early identification of, and consideration for, postpartum women's complaints and signs/symptoms, and appropriate interventions.
Keywords: Postpartum hemorrhage; postpartum period; nursing care; signals and symptons.
INTRODUCTION
The puerperium can be defined as the chronologically variable period of the pregnancy-puerperal cycle in which involutive manifestations occur, causing local and systemic changes caused by gestation in the maternal organism to return to the pre-gravid state1.
In this period, care for puerperal women should be provided in an interdisciplinary way and should comprehensively respond to their needs. The prevention of preventable puerperal deaths demands attention and availability of the health team2. This attention has become even more relevant before the 12,843 puerperal deaths occurred in Brazil during the period from 1996 to 2015, of which 10,840 occurred immediately and up to 42 days after delivery and 2,003 between 43 days and one year after delivery. These numbers represent 38% of maternal deaths in the country 3.
The major cause of puerperal death is postpartum haemorrhage (PPH), characterized by blood loss of more than 500 ml in vaginal deliveries and 1000 ml in cesarean deliveries4. Although the predominantly clinical diagnosis of PPH is simple to perform and involves only the measurement of blood loss through visual assessment and laboratory criteria 5, this problem still affects about 536 thousand women/year worldwide6,7, with death as outcome in approximately 25% of the cases4-8. In Brazil, HPP is responsible for more than 41% of maternal deaths9.
In view of the above, the importance of nursing assessment in helping the detection of HPP is evident. The nursing team is responsible for quantifying blood loss in the puerperium, performing early diagnosis of signs and symptoms of PPH, improving interdisciplinary communication and mobilizing a prompt and adequate response from the team, which demands adequate training and preparation4,5,7. Thus, the objective of this study was to correlate red cell loss with complaints, signs or symptoms of blood changes in the puerperium by measuring hemoglobin (Hb) and hematocrit (Ht) levels.
LITERATURE REVIEW
According to the World Health Organization, preventing and treating cases of increased blood loss can avoid most PPH deaths and this should be one of the primary goals of puerperal care10, with a view to a rigorous and careful evaluation.
Blood loss that progresses to PPH generally occurs with signs and symptoms of hypovolemia within 24 hours after delivery. Thus, recognizing signs, symptoms, and causes of PPH can significantly reduce morbidity and mortality associated with this problem11.
When investigating the obstacles to the prevention and treatment of PPH, the main one from the perspective of the patients is the lack of information about what is happening. Professionals, in turn, point to the lack of accessible guidelines in the workplace, lack of knowledge to recognize signs and symptoms, and communication failures between staff members12. In this sense, training is extremely important. After training the team on PPH and using a bundle for prevention and treatment of PPH cases, there was a 20.8% reduction in the cases of severe maternal morbidity13.
Since maternal death caused by PPH is associated with the quality of obstetric care during delivery and postpartum, postponing evaluation and monitoring may result in maternal death within the first 24 hours postpartum9. At this point, it is important to emphasize that despite the high rate of satisfaction of the puerperae towards the assistance provided by the health team during the inpatient care, failures related to attentions or absence of records, lack of constant vigilance during the immediate puerperium, lack of protocols and systematization of care during the postpartum period persist9. They reveal poorly visualized care deficits that may lead to risks in the evaluation of PPH in these puerperal women.
The analysis of cases of maternal death and the respective hospital care provided shows that the process involves social and assistance factors. Besides structural deficiencies in services, there are technical professional deficiencies that range from not negligence towards signs and symptoms up to delay in recognizing the severity of the cases, contributing to progress to death14. This indicates the importance of being attentive to the patients' complaints in order to avoid severe intercurrences and consequent death.
METHODOLOGY
This is a cross-sectional epidemiological study carried out in an obstetric unit of a large teaching hospital in the countryside of São Paulo.
The sample consisted of primiparous women who gave birth to live newborns as a result of single gestation, regardless of the delivery method adopted and interventions performed during prenatal, delivery and puerperium, in the period between August and December 2012. It should be pointed out that the choice of primiparous women occurred in an attempt to guarantee sample homogeneity and to reduce the possible effects of parity in the results since the literature indicates that parity and number of pregnancies higher than three are predictors for increased risk of HPP15,16. Moreover, some studies have confirmed the association between multiparity and uterine atony, which is the main cause of PPH17,18.
The sample was determined so as to ensure a maximum error of 10% between the estimated prevalence and the prevalence of PPH in the population, with a 95% confidence interval. Thus the sample consisted of a minimum of 68 primiparous women. However, data from 100 primiparous women were collected for convenience, thus respecting the proposed sample calculation.
The following criteria were used to exclude postpartum women: twin births; previous pregnancies that resulted in abortions and/or repeat abortions; abortions; fetal deaths and stillbirths; and patients with coagulopathies and/or hematological diseases (except for anemia during pregnancy).
An instrument structured and elaborated based on a review study published in the Cochrane Library19, that has been already used in a master's thesis 20 and previously tested in a pilot study, was used for the present data collection. The pilot study was performed with a sample of 10 (10%) subjects and the data were included in the study since no reformulation of the instrument was necessary.
The instrument presented the sections, namely: maternal data (sociodemographic, clinical and obstetric history data); labor, including hematimetric results (Hb and Ht) during admission of the parturient and interventions performed in this period; birth room (type of delivery, birth data, perineal integrity and deconditioning); third period (use of active management in this phase, need for ocytocic stimulation or ergotamine).
The final part of the instrument included two sections: puerperal complications (visual estimation of great or mild blood loss; need for blood transfusions; Hb level < 9 mg/dl 24 hours after childbirth; need for supplementation with iron in the puerperium in therapeutic dose; need for curettage; bleaching of mucous membranes; duration of third period exceeding 30 minutes; need for additional intravenous ocytocic stimulation to control bleeding; hemodynamic changes – hypotension, tachycardia, hypothermia, lipothymia and other complications; and red blood cell count results 48 hours after delivery (Hb and Ht levels) and registration of HPP in the medical chart.
In order to evaluate the blood loss in the puerperae, Hb and Ht dosages were collected at the admission of the parturient and at 48 hours postpartum. Blood loss was calculated as the difference between admission and postpartum Ht values. Ht values greater than or equal to 10% of that at admission were interepreted as PPH8.
Lipothymia, altered vital signs, mucosal bleaching, and apathy data collected through the review of prenatal cards and printed and electronic medical records were considered signs and symptoms of red cell loss.
In the analyses, the occurrence of PPH was considered the dependent variable and the reporting of complaints and/or signs and/or symptoms of hemorrhage were treated as independent variables.
The data were double-entered, with later validation, using the application Microsoft Excel®, and the consequent statistical analyses were carried out in the application Data Analysis and Statistical Software (Stata 9).
The main variables of interest were listed in categories and the effect of each variable was evaluated through an analysis of variance (F test) in order to compare the means of outcomes found among puerperae with and without signs suggestive of PPH.
Variables that presented p-values of less than 0.250 in the F test and that presented normal distribution were included in a Multiple Linear Regression in which the effect of each one of the variables was adjusted to the levels of the others, in order to seek relations that explained the event (variable of interest). Variables that presented p < 0.05 were considered significant.
The project of this study was approved by the Research Ethics Committee with Human Subjects of the Clinical Hospital of the Medical School of Ribeirão Preto of the University of São Paulo (CEP HCRP and FMRP - USP), HCRP process n° 4172/2011. The ethical principles of the research were observed, according to Resolution 466/2012 of the National Health Council.
RESULTS AND DISCUSSION
Sample characterization
The age of the 100 puerperae participating in the study ranged from 13 to 38 years, with a mean of 23.0 ± 5.7 years; 18% were adolescents and 5% were older women (age over 35 years); 65% did not have a permanent partner; 51% had completed high school; and 76% self-reported to be white. As for the situation in the labor market, 60% of the women did not have paid work.
It was verified that the majority of the patients (71%) had at least one pathology and 29% had no alterations, but they were referred to the institution because they resided in the area covered by the hospital complex. Hypertensive syndromes (26%), anemia (10%), diabetes (8%) and Human Papilloma Virus infection (8%) were the most frequent pathologies.
All participants had at least one prenatal consultation and the number of consultations ranged from one to 24, with a mean of 8.7 (SD: ± 4.0). When admitted to the institution, 64% of the women had term, 6% had post-term and 30% pre-term pregnancies. Labor resulted in normal labor in 62% of the cases, and 38% progressed to cesarean delivery.
Signs/symptoms and control of PPH
The use of additional oxytocin at therapeutic doses for the control of bleeding and uterine tone was the most performed intervention in the immediate postpartum period (20%), indicating that there were complications related to tonus and/or bleeding. Hemoglobin level < 9 mg/dl (48 hours postpartum) was also a frequent result (20%), and in addition, 14% of the women had records of lipothymic episodes and need for supplementation with ferrous sulfate. However, low frequencies of curettage (1%) and hemotransfusion (3%) were identified in the sample studied. The Ht at 48 hours postpartum varied from 19 to 48%, with a mean of 31.7% (SD: ± 5.2%).
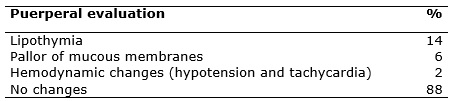
Approximately 20% of postpartum women presented signs and/or symptoms of excessive blood loss, evidenced by the occurrence of lipothymia and/or bleeding of mucous membranes and/or changes in vital signs (hypotension and tachycardia). Women who presented such complaints more often reported the presence of weakness, tiredness, discouragement, and apathy, as shown in Table 1.
TABLE 1:
Percentage distribution of signs or symptoms reported or
identified during the puerperal evaluation. Ribeirão Preto, 2012. 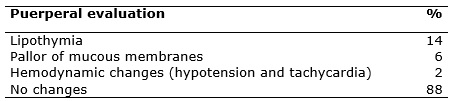
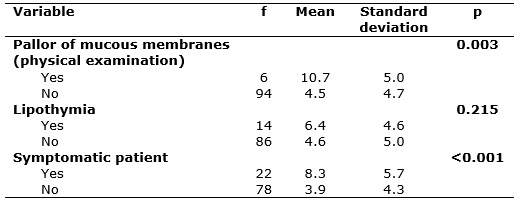
The data show that women with higher blood loss had mucosal pallor at physical examination and had complained about weakness, fatigue, discouragement and/or apathy in the medical records. Reporting of complaints and pallor mucous membranes caused statistical significance in red cell loss, according to Table 2.
TABLE 2:
Distribution of variables related to complaints and signs and/or symptoms
indicative of PPH. Ribeirão Preto, 2012.
In the case of PPH, women may be symptomatic or tolerate blood loss because of the increase of one to two liters of blood caused increasing of blood volume during pregnancy21.
However, the body tends to respond to hypovolemia with changes in vital signs, which include increased respiratory and heart rate. The reduction of circulating blood volume may also be expressed by the pallor of the skin and mucous membranes, decreased body temperature, and excessive sweating. As the loss becomes continuous, the cerebral blood flow is reduced and the woman may appear restless, confused, anxious, and ultimately lethargic. In such situations, a joint effort is needed for the detection of changes and early interventions21-23. It should be noted that even in more severe cases, where blood loss may lead to hypovolemic shock, the diagnosis is essentially clinical and based on a good anamnesis and physical examination22,24.
From this perspective, nurses should be alert to signs and symptoms of shock and treat the problem as early as possible in order to restore intravascular volume and revert the inadequate perfusion by redistributing fluid volume. In this sense, nurses are responsible for the execution of the prescribed treatment, monitoring the patient, preventing complications and promoting comfort, with the essential action of providing the appropriate treatment for a better prognosis24.
It should be noted that lipothymia also reflects excessive blood loss and can be defined as loss of muscle strength not linked to loss of consciousness, preserving respiratory and cardiac functions. It may be accompanied by skin-mucous pallor, profuse sweating, ringing in the ear, and a premonitory feeling of fainting21. Thus, its occurrence must be valued and investigated.
The results presented in this study point out the necessary attention to signs and/or symptoms and/or complaints of puerperal women, such as the valuation of anamnesis and physical examination, since the presence of symptoms and mucosal pallor were significant in this sample.
In the description of the nursing care provided in the immediate puerperium, nurses listed as main actions: management/administration of nursing actions - which include the role of nurses in foreseeing and providing assistance with human and material resources; nursing assistance/intervention - described as biologicist actions based only on technical procedures, such as bath assistance, medication administration, vital signs verification, without valuing actions established in the systematization of nursing care (SNC)25.
The nurses also stressed that women undergoing cesarean delivery are considered as highly complex patients while women who had normal delivery are classified as minimal care patients, focusing on the biomedical care model. When addressing the topic nursing investigation/research, they showed gaps in nursing work in this area, not valuing the use of evidence-based practices. In turn, on the topic of nursing teaching/learning, they indicated the educating role of the nursing team, as well as the lack of permanent education of the whole team25.
The need of implementing the SNC in the puerperium is evident, going beyond the biological and the technical aspects, having the integral and holistic care as guiding principle and valuing signs, symptoms, and complaints and meeting the affected human needs25.
It is obvious that nurses understand the importance of the SNC, but this requires knowledge, critical vision and sensitivity to meet the needs of the patient, enabling better working conditions for nurses. Thus, they point out the work overload, the small number of professionals, the lack of qualification and investments for the operationalization of the SNC, and the lack of commitment of the professionals with the updating and quality of the assistance as difficulties26.
In this sense, a study pointed out that the nursing process based on the Basic Human Needs Theory (psychobiological and psychosocial) makes it possible to identify the real needs of the puerperal women. Based on the identification of the needs affected, quality and individualized assistance can be promoted27.
Given the complexity PPH, and bearing in mind the implementation of SNC in puerperal care, the following nursing diagnoses are suggested: postpartum haemorrhage, postpartum haemorrhage risk, and vaginal bleeding. It is emphasized that the nursing diagnosis demonstrates a clinical diagnosis in which the nursing team is responsible for achieving an outcome after an intervention. In the case of PPH, the diagnosis is a collaborative task, that is, one that requires interdisciplinary action. Thus, the inclusion of these diagnoses in the SNC suggests a need for training the professionals who work in the obstetric area to meet this goal28.
The ability to quantify severe postpartum vaginal bleeding with reliable assessment instruments, including the identification of hemorrhagic signs and symptoms, the accurate quantification of loss, and laboratory confirmation of hematometric data, is fundamental to detect a case of PPH. Notably, the underestimation of postpartum blood loss can lead to erroneous quantification and delay the recognition of symptoms, increasing the risk of morbidity and mortality associated with PPH. Thus, it is necessary to train the entire team, especially nursing members, to recognize as early as possible the signs and symptoms of bleeding7.
A study that evaluated the quality of the care provided to puerperal women in a public maternity hospital in Manaus asked the patients about the positive characteristics that the nursing professionals should have and which they considered to be missing in the professionals who assisted them. Among the characteristics, the following stood out: education (25.7%); attention (22%); and patience (10.4%). As for the characteristics that the women found to be absent in the nursing team were lack of humanization (24.7%); lack of attention (21%) and irresponsibility (14.3%). The results showed weaknesses in care, mainly regarding the principle of humanized care and the need for greater attention of the professionals towards the puerperal women29.
It is known that Nursing is an important component of the health team that provides care to patients admitted to hospital institutions since these professionals stay 24 hours a day in the hospital and keep greater contact with the patients. However, it is noted that staff often displays lack of emotional engagement during patient care, even as a method adopted to place a barrier to protect themselves from psychic suffering30.
The quality and safety of the care provided to the patient are directly affected by the number of professionals in the nursing team, by the number of professionals per professional category (nursing assistants and technicians), by the nursing/patient ratio, and by the complexity of patients under nursing care31.
In this sense, the literature shows that the nursing team and the persons who receive care (puerperal women) and the care team have divergent views on the care provided. A qualitative study pointed out that, during the puerperium, both staff and the puerperal women focus primarily on the nutritional needs of the newborns, focusing evaluations and guidance on issues related to breastfeeding and care with the babies32.
The analysis of the speeches also made it possible to identify in the aforementioned study the thematic category Postpartum : is maternal care forgotten? pointing to gaps in the comprehensive health care of the puerperal woman. From the point of view of women, puerperal care was restricted to technical measures aimed primarily at surgical incisions and discharge guidelines (avoiding physical exertion, sexual abstinence, and suture removal). However, for the nursing team, puerperal care consists in routine health assessment based on techniques such as blood pressure and blood glucose measurement, with no major particularities32.
The results of the present study reveal the importance of the nursing team to promote safe and quality care for puerperal women.
CONCLUSION
The existence of the relationship between significant blood loss and signs and symptoms such as mucosal pallor, complaints of weakness, fatigue, discouragement, and apathy were identified.
The rapid diagnosis - identification of signs and symptoms - of PPH is essential to minimize the risk of death of puerperal women.
The importance of a systematized and qualified nursing care in the puerperium based on the best evidence is emphasized. Among the nursing actions, it is necessary to value the complaints of the puerperal women, using pertinent tools such as listening without judgments, anamnesis and a thorough physical examination, aiming at better interventions.
Quality care can substantially reduce maternal morbidity and mortality rates related to PPH and, concomitantly, contribute to the achievement of the Millennium Development Goal 5 (reducing mortality and promoting maternal health).
The authors understand as limitations of the study the restricted population from the studied municipality and the small sample, that make it impossible to generalize the results.
REFERENCES
1.Ministry of Health (Br). Prenatal and puerperium - qualified and humanized care. Brasília (DF): Ministry of Health; 2006.
2.Andrade RD, Santos JS, Maia MAC, de Mello DF. Factors related to women's health in puerperium and repercussions on child health. Esc Anna Nery. 2015;19(1):180-6. http://dx.doi.org/10.5935/1414-8145.20150025
3.Unified Health System. Maternal deaths, according to the place of residence in the period from 1996 to 2015. [Internet]. 2017 [cited on 08 Sep, 2017]. Available from: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/mat10uf.def
4.Prata N, Bell S, Holston M, Quaiyum MA. Is attendant at delivery associated with the use of interventions to prevent postpartum hemorrhage at home births? The case of Bangladesh. BMC Pregnancy Childbirth. 2014, 14: 24. http://doi.org/10.1186/1471-2393-14-24
5.Gabel KT, Weeber TA. Measuring and communicating blood loss during obstetric hemorrhage. JOGNN. 2012; (41): 551-558. http://dx.doi.org/10.1111/j.1552-6909.2012.01375.x
6.Viana RC, Novaes MRCG, Calderon IMP. Maternal Mortality - an update approach. With Health Sciences. 2011; [cited on Jun 10, 2017] 22 (Sup 1): S141-S152. Available from: http://bvsms.saude.gov.br/bvs/artigos/mortalidade_materna.pdf
7.Edmonds JK, Hruschka DA, Sibley LM. A comparison of excessive postpartum blood loss estimates among three subgroups of women attending births in Matlab, Bangladesh. J Midwifery Womens Health. 2010; 55 (4):378-82. doi: http://10.1016/j.jmwh.2009.08.003
8.American College of Obstetricians and Gynecologists. ACOG Simulations Consortium Learning Objectives Postpartum Hemorrhage Caused by Uterine Atony. Washington (DC): ACOG; 2013.
9.Souza ML, Laurenti R, Knobel R, Monticelli M, Bruggemann OM, Drake E. Maternal mortality due to hemorrhage in Brazil. Rev Latino-Am Nursing. 2013; 21(3):711-8.
10.World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. Genebra(Swi): WHO; 2014.
11.Evensen A, Anderson J, Fontaine P. Postpartum hemorrhage: prevention and treatment. Am Fam Physician. 2017; 95(7): 442-9.
12.Woiski MD, Belfroid E, Liefer J, Grol RP, Scheepers HC, Hermens RP. Influencing factors for high quality care on postpartum haemorrhage in the Netherlands: patient and professional perspectives. BMC Pregnancy Childbirth. 2015; 15: 272. doi: http://10.1186/s12884-015-0707-9
13.Main EK, Cape V, Abreo A, Vasher J, Woods A, Carpenter A, Gould JB. Reduction of severe maternal morbidity from hemorrhage using a state perinatal quality collaborative. Am J Obstet Gynecol. 2017; 216 (3): 298e.298e11. doi: http://10.1016/j.ajog.2017.01.017
14.Saito PY, Teixeira NZF, Nakagawa JTT. Analysis of the hospital care of the cases of maternal deaths: a critical reflection. Rev enferm UERJ. 2016; 24(1): e12530.
15.Ruiz MT, Soler ZASG. Characteristics of obstetric care for women during the fourth period of delivery in a general teaching hospital. Enferm Brasil. 2007; 6(4): 248-55.
16.Royal College of Obstetricians and Gynaecologists. Parity and postpartum haemorrhage. London(UK): RGOG; 2013.
17.Sheldon WR, Blum J, Vogel JP, Souza JP, Gulmezoglu AM, Winikoff B, on behalf of the WHO Multicountry Survey on Maternal and Newborn Health Research Network. Postpartum haemorrhage management, risks and maternal outcomes: findings from the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG. 2014; 121 (Suppl.1): 5-13. doi: http://10.1111/1471-0528.12636
18.Kominiarek MA, Kilpatrick SJ. Postpartum hemorrhage: a recurring pregnancy complication. Semin Perinatol. 2007; 31: 159-66. doi: http://10.1053/j.semperi.2007.03.001
19.Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour (Cochrane Rewiew). In: The Cochrane Library. Chichester (UK): John Wiley & Sons Ltd; 2007.
20.Ruiz MT. Management of the third period of childbirth and its repercussions in the puerperium [master's thesis]. Ribeirão Preto (SP): University of São Paulo; 2008.
21.Leifer G. Obstetric Nursing. 11th ed. Rio de Janeiro: Elsevier; 2014.
22.American College of Surgeons. Advanced Trauma Life Support. Student Course Manual. 9th ed. Chicago (USA): ACS; 2012.
23.Felice CD, Susin CF, Costabeber AM, Rodrigues AT, Beck MO, Hertz E. Shock: emergency diagnosis and treatment. Rev AMRIGS. 2011; 55 (2): 179-96.
24.Costa ICN, Rocha AKL. Nursing care for patients at Shock. InterScientia. 2014; 2(1): 77-88.
25.Cassiano AN, Holanda CSM, Costa RKS, Morais FRR, Maranhão TMO. Nursing care to woman in immediate puerperium: a narrative description. J res: fundam care online. 2015; 7(1):2061-2071. doi: http://10.9789/2175-5361.2015.v7i1.2061-2071
26.Castro RR, Alvino ALFN, Rouberte ESC, Moreira RP, Oliveira RL. Conceptions and challenges in the systematization of nursing care. Rev enferm UERJ, 2016; 24(5):e10461. http://dx.doi.org/10.12957/reuerj.2016.10461
27.Leite MCA, Medeiros AL, Nóbrega MML, Fernandes MGM. Nursing care postpartum women using the Horta's Theory and INCP. Rev RENE. 2013; 14(1):199-208.
28.Silva AF, Nóbrega MMl, Macedo WCM. Nursing diagnoses/outcomes for parturient and puerperal women using the International Classification for Nursing Practice. Rev Eletr Enf. 2012;14(2):267-76. http://dx.doi.org/10.5216/ree.v14i2.11211
29.Llapa-Rodriguez EO, Cunha S, Inagaki ADM, Mattos MCT, Abud ACF. Quality of postpartum nursing care in a mother´s view. Rev enferm UFPE. 2013; 7(1):76-82. doi: http://10.5205/reuol.3049-24704-1-LE.0701201311
30.Filizola CLA, Ferreira NMLA. Emotional involvement of the nursing team: reality or myth? Rev Latino-Am Nursing. 1997; 5: 9-17.
31.Garcia PC, Fugulin FMT. Time of nursing care in an adult intensive care units and indicators of quality of care: correlational analysis. Rev Latino-Am Nursing. 2012; 20 (4): 651-8.
32.Pereira MC, Gradim CVC. Puerperal consultation: the view of nurses and of puerperal women. Cienc Cuid Saude. 2014; 13(1): 35-42. doi: http://10.4025/cienccuidsaude.v13i1.19572