ORIGINAL RESEARCH
Nurses' role in early detection of breast cáncer
Carla Andréia Vilanova Marques I; Vivian Rodrigues da SilvaII; Maria Gaby Rivero de Gutiérrez III
I
Doctorate of Nursing from Federal University of São Paulo. Brazil.
E-mail: cvilanova@inca.gov.br
II
Nursing Degree from Federal University of São Paulo. Brazil. E-mail: vivian.rs85@gmail.com.br
III
Professor at Paulista School of Nursing from Federal University of São
Paulo. Brazil. E-mail: gaby.gutierrez@unifesp.com
IV
Thanks to the National Council of Science and Technology for financial
assistance.
DOI: http://dx.doi.org/10.12957/reuerj.2017.22639
ABSTRACT
Objective: to examine the actions of nurses towards early detection of breast cancer in primary health care (PHC) services, as well as the structure of such services. Method: in this cross-sectional study (with ethics committee approval No. 0185.0162.162-09), validated questionnaires were applied to 13 nurses, 4 managers and 85 users from 4 PHC facilities in São Paulo State in 2011. The resources and training offered and the frequency of clinical breast examinations (CBE) and breast cancer education meetings were analyzed descriptively. Results: 61.5% nurses had screening guidelines; 23% had been trained; 46.2% held educational meetings; 92.3% performed CBE, 66.7% with annual indication and 58.5% with no target age. There were 22 offices for 25 physicians and another 7 offices for 15 nurses. There were 22 consulting rooms for 25 physicians and only 7 for 15 nurses. Trained nurses attained better compliance with ministry of health recommendations that other nurses. Conclusion: nurses perform breast cancer detection actions, but there is some noncompliance with governmental guidelines, while training and PHC facility structure were predictors of better compliance with recommendations.
Keywords: Nursing; breast neoplasm; primary health care; mass screening.
INTRODUCTION
Breast cancer represents the most prevalent form of cancer in the world,
second only to skin cancer1. In Brazil, the rates of late
diagnosis and resulting mortality, continues to increase2.
To control this problem, various prevention measures are being encouraged,
such as: adopting a healthier lifestyle, awareness of one's body, weight
control, reduction of alcohol consumption and eliminating tobacco 2-4. Meanwhile, more specific measures to control this type of
tumor, focus on the early detection and treatment1,4-6.
From a balanced perspective, evidence suggests (after weighing up both the risks and the benefits) that a mammogram scan is the gold standard diagnostic method to be used5,6. However, there still remain some doubts and so therefore, studies emphasize the importance of having a clinical breast exam (CBE) for women with heavier breasts, implants or who are post-radiotherapy. While for those who refuse the exam or for countries with limited resources or dubious imaging quality, the use of lighter treatments is recommended2,6.
In Brazil, for early cancer detection, the Ministry of Health (MoH) recommends that physicians and nurses from primary health care (PHC) services conduct both CBE on women with a regular risk, from the age of forty years. While for those considered to be with a high risk, the recommendation is to be examined from age thirty-five. It is also recommended that health professionals administer every two years, an mammography on women between 50 and 69 years old. And for those with a higher risk factor, it is recommended both exams annually, from the age of 357. Additionally, there must be an emphasis on social empowerment via the dissemination of information to the target demographic, including being more self-aware regarding one's body, in the form of breast self examination (BSE) with the intention of being able to identify suspect alterations or other warning signals2,6,7.
Furthermore, although holistic training is given to nurses in Brazil and can be useful for the early detection of breast cancer, little is known about this area4,8,9. Given this fact, the study here presents the objective of analyzing various procedures used by PHC nurses in the early detection of breast cancer and the structure of such services.
LITERATURE REVIEW
Studies in Brazil and in countries such as Nigeria, India, Turkey and nations in the Caribbean reveal that PHC nurses often present a lack of knowledge regarding risk factors and diagnosis methods of breast cancer tumors8,10-15. However, despite this, in PHC services, in which primary and secondary prevention measures are offered, the majority of the population seeks for healthcare1,6-9,16.
On another more positive note, research reveals that health literacy for the community, constitutes being the most effective empowerment tool for social control in order to strengthening improvements in health services 6,9,16,17. In this regard, as a healthcare educator, the nurse can direct information (either in verbal or written form) about available interventions, preventative measures to cancer prevention, in different forms and locations, such as in clinical consultations, waiting rooms, during Pap Smear and in organized meetings or activities together with the community7,13.
In reference to clinical practice, despite the first national program for cancer control dating back to 1998, investigations demonstrate that some nurses have not CBE confidence, are unaware of Brazilian target public and about active search, the other ones who were performing CBE didn't follow basic technique, such as static and dynamic breast inspection, breasts and armpits palpation and examination of nipple discharge7,8,17. An inadequate infrastructure and excessive demand were perceived as the main problems for this.
METHODOLOGY
A cross-sectional study was conducted in February of 2011, in four PHC services in the southeastern region of the city of São Paulo. Data were colleted from three types of employees (managers, nurses and follow-up patients in PHC) for analyze the practices of breast cancer detection performed by PHC nurses. The sampling process was conducted in two stages, with the inclusion of PHC services institutes after January 2006, managers and nurses without restriction of age or gender, and female patients ≥35 and 69 years of age in PHC follow-up of ≥ three years.
To target population sampling, it has been considered 50% of outcome, 95% of confidence interval, maximum sampling error of 3% and 2.0 of design effect (deff).
In the first stage, 38 out of 90 PHC services in the area were selected and then from this number, 10% rate were considered as a final sample, corresponding with two traditional PHC services, one Mixed and one Family Health Strategy (FHS)18.
In the second stage, all nurses (f=15) and managers (f=4) were invited, and out of a total of 760 users within the sample, 85 were interviewed (subsample). However, during the collection of data, the absence of two nurses in the PHC services, resulted in their exclusion from said sample. After approval from the Committee of Research Ethics (nº 0185.0162.162-09) and those involved, trained interviewers conducted validated questionnaires to PHC informants19.
In this study, the variables analyzed were backgrounds of the nurses (educational level, professional experience and type of PHC in which they function) as well as PHC services infrastructure and resources (availability of guidelines, offices, operating wards, employees and educational materials), and factors relevant to CBE care processes (age, frequency, reason, professional responsible, moment of investigation, challenges, risk factors and educational activities offered). The absolute, relative and average terms frequencies were measured using the Statistical Package for the Social Sciences (version 20).
RESULTS
Of the 13 nurses interviewed, 5 (38.5) worked in FHS, 5 (38.5%) in Mixed and 3 (23.1%) in Traditional PHC services. As for the average time employed by these PHC nurses, it was revealed that those who worked in FHS had an average of 3 years and 10 months experience (maximum 9 years, minimum 4 months), those from Mixed PHC had an average of 3 years and 6 months experience (maximum 11 years, minimum 1 year and 6 months) and those from the Traditional group had an average of 15 years and 1 month of experience (maximum of 25 years, minimum of 11 months).
With regards to education and training, the majority (69.2%) were specialized, of which four were in Public Health Nurse, two Midwife, two Family Nurse Practitioner and one Occupational Health Nurse. Training in the tracking of the breast cancer was offered to 7 (53.8%) of them, of which 4 (57.1%) had completed more than two years and 3 (42.9%) had completed less than two years.
The risk factors for the breast disease were investigated in 11 (84.6%) of those interviewed, in clinical consultations (30.8%), during Pap Smear (15.4%) or in both situations (38.4%). Orientation was offered to female patients (from the age of 35 and up every month) regarding BSE by 12 (92.3) of these health professionals, in appropriate moments, such as the Pap Test (25%) or clinical consultation (16.7%).
The PHC guideline availability was reported among 8 (61.5%) of the nurses surveyed, while 4 (30.8%) did not have it and 1 (7.7%) was unaware of such a thing. The promotion of educational meetings about this theme occurred among 6 (46.2%) of those surveyed, in contrast with the actual clinical performance of 12 nurses interviewed (92.3), supported by evidence revealing an average of one to ten medical consultations per day.
In regards to CBE performance by 12 nurses, 5 (41.6%) alleged that there were no real impediments for their work, while 2 (16.6%) claimed that a lack of routine impeded things. Despite this, the majority (92.3%) of nurses performed CBE, predominantly during the collection of oncotic cytology (33.3%), without importance for the age of patient (58.5%) and on a yearly basis (66.7%).
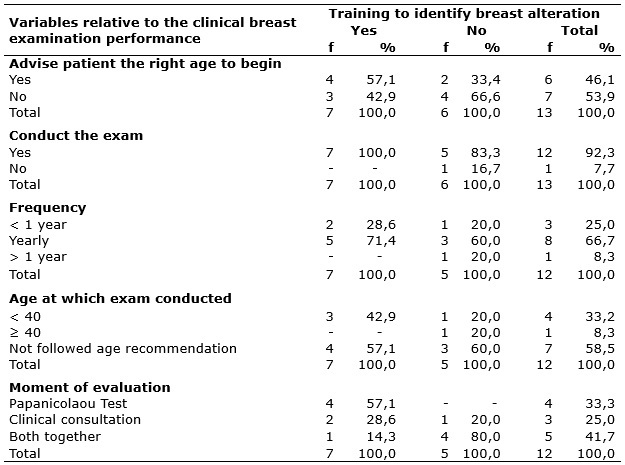
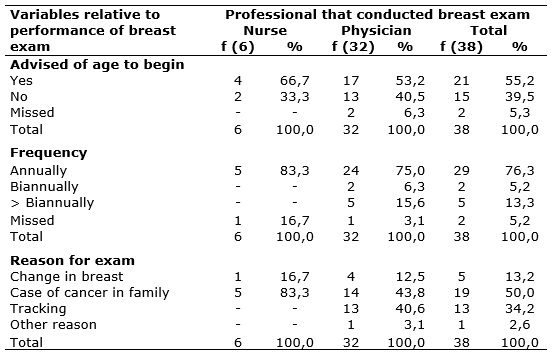
For cases of changes to CBE in different PHC services, the most common action performed among 9 (75%) out of the 13 nurses interviewed, was the solicitation of a medical evaluation. While for the target demographic that had not done CBE, an active search was conducted by 2 nurses from FHS and by 1 belonging to Mixed PHC service. The frequency of CBE was higher among nurses from Mixed PHC and FHS (38.5% respectively) versus the Traditional (15.3%) services. The practice of CBE was analyzed with via the training of its nurses, as seen in Table 1.
TABLE 1
. Distribution of variables regarding clinical breast exams, based on
training after 2004. Southeastern districts of the city of São Paulo, SP,
Brazil, 2011.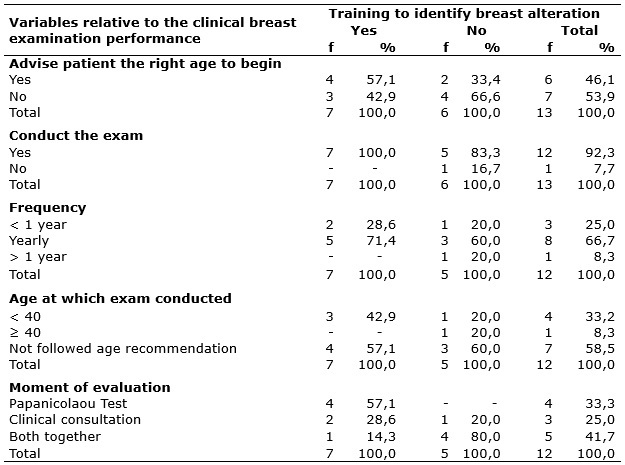
Notice how, except in the item age at which exam conducted, that trained nurses were more successful in reaching the recommendation of MoH when compared to those without training, as shown here in Table 1.
The results regarding care structure for the early detection of breast cancer, according to the four managers at PHC selected, are specified in Table 2.
TABLE 2:
Distribution of care structure for the detection of breast cancer,
according to the care model at UBS. Southeast region of the city of São
Paulo, SP, Brazil, 2011.
(*) UBS - Basic health unit. (‡) ESF - Family Health Strategy.
The amount of health offices and physicians were superior to those of nurses, according to the data in Table 2. Furthermore, 3 (75%) mentioned that the lack of professional staff at PHC, as well as the difficulty of scheduling exams, were the biggest impediments to implementing proposed actions.
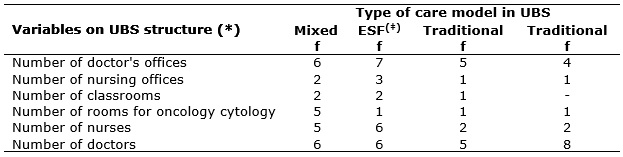
In regards to report that 85 of female interviewed PHC of São Paulo, 38 (43.5%) had their breasts examined between 2008 and 2011. The details about this exam are presented in Table 3.
TABLE 3:
Distribution of variables regarding clinical breast exams, based on
professional category. Southeastern districts of the city of São Paulo, SP,
Brazil, 2011.
The CBE performed by physicians in relation to the conduct by nurses was higher. Just as with the frequency of CBE, the annual exam was more common in both professional categories (Table 3).
DISCUSSION
In this investigation, the results highlighted that the majority of nurses had specialized knowledge in relation to PHC and worked almost four years in these services. Note that also, there is a large variation in terms of time and of professional expertise in PHC (between 4 months and 25 years). Additionally, those in Traditional PHC services, worked more time when compared to the others.
A national study revealed that nurses connected in the PHC service in the state of São Paulo, had more or less the same profile in terms of educational training and amount of work experience20 . Similarities were also found in the state of Pernambuco, in regards to amount of work experience activity in PHC, among this class of workers (averaging 5 years), while in the state of Rio Grande do Norte, the majority allege to have worked for more than 5 years in these types of environments10,21.
A similar study of nurses in Turkey highlighted a relation in the CBE performance with having the longest amount of time with professional experience15. That aspect has not yet been explored in this current study in Brazil, due to the number of nurses and amount of experience of those interviewed.
Despite the viability of amount of work experience observed among PHC professionals of Brazil things can be better understood when considering the transition from a Traditional care assistance model, to the current one in FHS, established with the creation of municipality-based in São Paulo healthcare services, starting in the year 2000 and still being implemented 22,23. The evaluation of the effects of FHS in PHC regarding health were positive, encouraging its expansion24,25. Consequently, more nurses were admitted into PHC. However, data emphasizes that this adaptation requires new attributes and work conditions in relation to a more centralized form of training in a biomedical model. Issues include a limited possibility of career advancement due to the precarious nature of employment, in addition to the high level of employee rotation within this field 20,26. Such factors appear to explain, in part, this observed trend.
The frequent replacement of nurses, had a negative impact on the quality of care, such as impeding the establishment of personal connections with patients, something which is a vital factor for healthcare to be more effective26. Beyond this, the rotation of nursing employees were its effects on having an organized work environment, overburdened staff that continue in service, precarious and discontinued care and the increased costs for the training, were all noted as negative consequences 20,26.
As a study on staff turnover shows, regarding PHC in Brazil, this factor is a result of conjuncture logistics both internal and external, within such services26. Therefore, change can be promoted by way of integrated education and training to meet the demands of the population, such as increasing the number of permanent job offers within healthcare and the adoption of management and participative practices in these locations 9,20,26.
In the context of this study focusing on the city of São Paulo, it can be seen that more than half of the nurses interviewed were available in their services, were aware of workplace procedures and had received training within the last two years for early detection of breast cancer (this information confirmed by local managers).
By contrast, 87.9% of nursing professionals currently in PHC service in the state of Rio Grande do Norte, allege to have not received any training relevant to this theme17. In a national survey conducted among 477 professionals in the health and nursing fields (as well as physiotherapy and medicine) more than half (55%) had received oncology training for their services, principally via specialized courses or residency (84.3%)27. The same group indicated that breast cancer tumors (24.4%) and PHC (65.8%) were the fields with the biggest necessity of qualification27.
Data from other countries indicates that 8% of nurses in Saudi Arabia were trained in the control of breast neoplasm. While lower rates of training for CBE (4.3%) and BSE (5.2%) were offered to nursing professionals in Nigeria12,28. According to these findings, note that little investment had been destined to guarantee the quality of the early detection of breast cancer, reflected in the lack of training of nurses at PHC setting. Therefore, it becomes imperative to establish and maintain care procedures within these services, in addition to the distribution of these recommendations, either at the physical location or online. This can be done via local initiative or in partnership with educational and research institutions1,9,16,29-31.
One aspect not yet analyzed with the nurses interviewed, as well as with any other national investigation, refers to the relation between one´s training and their practices in the detection of breast tumors. In international studies, four different surveys explored this existence of the relation between said variables, in which half confirmed that there does in fact exist this association, while other half did not find any type of relation whatsoever13-15,28.
Another aspect that was identified, in regard to nurses in the city of São Paulo, references the small proportion that had educational meetings about the theme. While on the other hand, the majority encouraged female patients about awareness, via a BSE and educating the public about health in more intimate opportunities, such as during health consultations or in the collection of Papanicolau Test.
Another factor drawn from results is how certain elements appear to emerge from the data in reference to managers within the four PHC services, in which it was observed that the internal structure in which they acted, how nurses favored the clinical approach as opposed to a more educational one, characterized by the number of spaces destined for each purpose (37 for clinical activity and only 5 for educational). This picture presented, is consistent with certain authors, which highlight that a lack of community involvement in this process of care and assistance and a lack of initiatives to instigate collaborative work between healthcare professionals and users of their services22-24.
In regard to actions in the detection of the disease, the majority of nurses interviewed in the study did not advise their patients about the age in which CBE is recommended. However, in clinical consultations investigating risk factors for cancer, while examining the breasts of their patients during yearly checkups, especially during the collection of Papanicolaou Test, without referencing age, simply recommended a medical evaluation for those who presented abnormal breast alterations. A lack of routine was cited as a factor, which complicated their work.
In Rio Grande do Norte, CBE was the diagnosis method most valued, more so than mammography (72.3%) once the exam had been indicated to women with a complaint about a lump on the breast (68%), without taking into account the frequency (78.7%). Just as in the rural region within the state of Pernambuco, as in the rural areas within the state of Minas Gerais, the frequency of CBE by nurses was definitely higher (100% and 92%, respectively). Yet, information about the orientations and approaches in the identification of changes to the breasts of the patients, was not explored in these areas21,32.
Among the 120 nurses in Nigeria who were interviewed in another study, the biannual frequency of CBE (40%) surpassed the yearly rate (7.8%), 8 (7%) reported that this exam is medical practice and 13 (11.3%) claim to be attributed to this specifically, while the other 12 recognized that both professionals should conduct it6. CBE was performed by 52 (45.2%) of medical employees, despite some not feeling totally capable (13.5), causing the rerouting of changes to the breasts, to secondary and tertiary line of care6.
In a different study, featuring 62 nurses in the Caribbean, the majority (61,3%) recommended that women from the age of 20 years old, have their breasts examined by a health professional, while the minority (12.9%) suggested that this exam to be conducted from the age of 40 years (36%) 12.
When analyzing these findings it can be perceived that publications, regarding the work of nurses in the early detection of breast cancer, are rarely released, despite being part of a professional field that acts in the majority of PHC and who are the closest to female patients 8,10-15.
Furthermore, it is a fact that the implementation of CBE and health education in the early detection of breast cancer does not require much financial cost nor expensive equipment. But simply requires an increased number of trained professionals, strategic planning, care coordination, and basic physical infrastructure in the implementation of assistance and care 1,9,16,29-31.
According to a report by managers of PHC services in the city of São Paulo, the reduced number of professional medical staff was one of the main barriers in the implementation of this proposal. Local administrators indicated that the quantity of nurses (f=15) and nurse's offices (f=7) was extremely low and insufficient, within the context of the total number of professional medical staff (f=25) and medical offices (f=22).
Validating this point, more than half of the 85 users interviewed in São Paulo PHC services claimed that although nurses and physicians were oriented about what age to initiate the CBE, that only physicians on a yearly basis predominantly conducted the breast evaluation.
MoH recommends that in all female consultations, the CBE should be done as part of a holistic healthcare treatment7. Therefore, some elements such as adequate physical infrastructure, sufficient human resources, guidelines availability and sufficient assistants are required at least at a basic level1,6,9,16.
From this perspective, the findings assert that the infrastructure, work procedures and training offered at PHC services are not favorable in terms of work conditions for nurses. Therefore, some recommendations include an even distribution of clinical offices among the staff, increasing the number of nursing staff, training regarding the service subject in question, allocation of nurses for the coordination of programs, encouraging more educational activities and implementing these actions proposed by MoH, and some type of presentation for everyone involved, regarding targets to reach and points to improve.
Additionally, in regards to this situation, a fact that was verified in a national investigation of nurses of PHC, was evidence of the removal of nursing staff from clinical practice20. It was observed that these models of PHC in São Paulo in which it was assumed that treatment included better relationships between the nursing staff and the community (FHS and Mixed PHC services) focusing on having more staff, the opposite situation was actually occurring.
Furthermore, it was verified that the staff, which received more training, had practices that were more consistent with what was established by MoH. Due to this, to make improvements in the detection of neoplasm in Brazil, it is recommended that nurses participate in this training, performing CBE on women of the target demographic (≥ 40 years old), maintaining the frequency as recommended by government (yearly), initiating the participation of those who do not partake or are unwilling, via educational forms and active search.
CONCLUSION
The majority of nurses are specialized in areas related to PHC. However, the service training for the early detection of breast cancer did not reach all nurses and that the inferior infrastructure of PHC did not favor the situation. Note also, that active nurses in their largest number in PHC services and those that received the most training also had the best practices, indicating that such conditions are indicators of the quality of care. These factors combined can be reflected in the lack of conformity of recommendations, given that there is no unanimity among nurses regarding conducting educational meetings and of CBE in the target demographic during the collection of oncotic cytology.
The present investigation offers a reflection of practices regarding the early detection of breast cancer on the part of nurses, facing an inferior infrastructure and inadequate working processes within four services of São Paulo APS. Regardless, it must be considered that this picture was constructed according to information self-reported by informants, and based on a unique geographical area with specific characteristics and which does not necessarily reflect other regions of Brazil.
REFERENCES
1.Denny L, de Sanjose S, Mutebi M, Anderson BO, Kim J, Jeronimo J, et al. Interventions to close the divide for women with breast and cervical cancer between low-income and middle-income countries and high-income countries. Lancet. 2016; (16):31795-0. doi: http://dx.doi.org/10.1016/S0140-6736(16)31795-0
2.Rocha-Brischiliari SC, Oliveira RR, Andrade L, Brischiliari A, Gravena AAF, Carvalho MDB, et al. The rise in mortality from breast cancer in young women: trend analysis in Brazil. PLoS One. 2017; 12(1):e0168950. doi: https://doi.org/10.1371/journal.pone.0168950
3. Azevedo ESG , Moura L , Curado MP , Gomes FS , Otero U , Rezende LF, et al. The fraction of cancer attributable to ways of life, infections, occupation, and environmental agents in Brazil in 2020. PLoS One. 2016; 11(2):e0148761. doi: http://10.1371/journal.pone.0148761
4.Jerônimo AFA, Freitas AG, Weller M. Risk factors of breast cancer and knowledge about the disease: an integrative revision of Latin American studies. Cien Saude. 2017; 22(1):135-49. doi: http://dx.doi.org/10.1590/1413-81232017221.09272015
5.Pace LE, Keating NLA. A systematic assessment of benefits and risk to guide breast cancer screening decisions. JAMA. 2014;311(13):1327-35. doi: http://dx.doi.org/ 10.1001/jama.2014.1398
6.Coleman C. Early detection and screening for breast cancer. Seminar in Oncology Nursing. 2017; 33(2):141-55. doi: http://dx.doi.org/ 10.1016/j.soncn.2017.02.00 9
7.Marques CA, Figueiredo EM, Gutiérrez MG. Public health policies for breast cancer control in Brazil. Rev enferm UERJ. 2015; 23(2):272-8. doi: http://dx.doi.org/10.12957/reuerj.2015.13632
8.Cavalcante SAM, Silva BS, Marques CAV, Figueiredo EM, Gutiérrez MGR. Nurse actions towards breast cancer screening and early diagnosis in Brazil. Rev Bras Cancerol. 2013 [cited 2016 Aug 15]; 59(3):459-66. Available from: http://www.inca.gov.br/rbc/n_59/v03/pdf/17-revisao_literatura-acoes-enfermeiro-rastreamento-diagnostico-cancer-mama-brasil.pdf
9.Galassi A, Challinor J and Key Stakeholder Group on Oncology Nursing in Low- and Middle-Income Countries . Strengthening the oncology nurse workforce in low-income and middle-income countries. Lancet Oncol. 2015; 16(8):887-8. doi: http://dx.doi.org/10.1016/S1470-2045(15)00144-8
10.Jácome EM, Silva RM, Gonçalves MLC, Collares PMC, Barbosa IL. Breast cancer detection: knowledge, attitude and practices of doctors and nurses from the Family Health Strategy of Mossoró, RN, Brazil. Rev Bras Cancerol. 2011[cited 2016 Aug 15]; 57(2):189-98. Available from: http://www.inca.gov.br/rbc/n_57/v02/pdf/06_artigo_deteccao_cancer_mama_conhecimento_atitude_pratica_medicos_enfer meiros_estrategia_saude_familia_mossoro_RN_brasil.pdf
11.Barreto ASB, Mendes MFM. Evaluation of a strategy adopted to expand adherence to breast cancer screening in brazilian northeast. Rev Bras Ginecol Obstet. 2012 [cited 2016 Aug 15]; 34(2):86-91. Available from: http://www.scielo.br/pdf/rbgo/v34n2/a08v34n2
12.Oluwatosin O. Primary health care nurses knowledge practice and client teaching of early detection measures of breast cancer in Ibadan. BMC Nursing. 2012; 11:22. doi: http://dx.doi.org/ 10.1186/1472-6955-11-22
13.Fotedar V, Seam RK, Gupta MK, Guota M, Vats S, Verma S. Knowledge of risk factors & early detection methods and practices towards breast cancer among nurses in Indira Gandhi Medical College, Shimla, Himachal Pradesh, India. Asian Pac. J. Cancer Prev. 2013; 14(1):117-20. doi: http://dx.doi.org/10.7314/APJCP.2013.14.1.117
14.Onuoha PC, Richards OR. Knowledge of breast cancer: a study of the primary health care (phc) nurses of the caribbean island of st vincent and the grenadines. International Journal of Current Research. 2014[cited 2016 Aug 15]; 6(12):11023-30. Available in: http://www.journalcra.com/sites/default/files/6833.pdf
15.Andsoy II, Gul A. Breast, cervix and colorectal cancer knowlege amog nurses in Turkey. Asian Pac J Cancer Prev. 2014; 15(5):2267-72. doi: http://dx.doi.org/10.7314/APJCP.2014.15.5.2267
16.Rubin G, Berendsen A, Crawford SM, Dommett R, Earle C, Emery J, et al. The expanding role of primary care in cancer control. Lancet Oncol. 2015; 16(12):1231-72. doi: https://doi.org/10.1016/S1470-2045(15)00205-3
17.Lourenço TS, Mauad EC, Vieira RAC. Barriers in the breast cancer screening and the role of nursing: an integrative review. Rev Bras Enferm. 2013; 66(4):585-91. doi: http://dx.doi.org/10.1590/S0034-71672013000400018
18.Marques CAV, Cassenote AJF, Gutiérrez MGR, Figueiredo EN. Breast cancer control in primary health care: challenges in building a sampling plan. Rev. APS. 2014[cited 2016 Aug 15]; 17(2):263-7. Available from: https://aps.ufjf.emnuvens.com.br/aps/article/view/2186/811
19.Marques CA, Figueiredo EM, Gutiérrez MG. Validation of an instrument to identify actions for screening and detection of breast cancer. Acta Paul Enferm. 2015; 28(2):183-9. doi: http://dx.doi.org/10.1590/1982-0194201500031
20.Galavote HS, Zandonade E, Garcia ACP, Freitas PSS, Seidl H, Contarato PC, et al. The nurse's work in primary health care. Esc Anna Nery. 2016; 20(1):90-8. doi: http://dx.doi.org/10.5935/1414-8145.20160013
21.Rodrigues FB, Santos JJP, Pinto WM, Brandão CS. The nurse's job to prevent breast cancer in pernambuco's interior: the professional's practice approach. Saúde Coletiva em Debate. 2012[cited 2016 Aug 15]; 2(1):73-86. Available from: http://fis.edu.br/revistaenfermagem/artigos/vol02/artigo07.pdf
22.Macinko J, Harris MJ. Brazil's Family Health Strategy: delivering community-based primary care in a universal health system. N Engl J Med. 2015; 372:2177-218. doi: http://dx.doi.org/10.1056/NEJMp1501140
23.Sala A, Luppi CG, Simões O, Marsiglia RG. Integrality and primary health care: assessment in the perspective of health services users in the city of São Paulo. Saude soc. 2011[cited 2016 Aug 15]; 20(4):948-60. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-12902011000400012&lng=en
24.Costa NR. The family health strategy: primary health care and the challenge of Brazilian metropolises. Ciênc saúde coletiva. 2016; 21(5):1389-98. doi: http://dx.doi.org/10.1590/1413-81232015215.24842015
25.Malta DC, Santos MAS, Stopa SR, Vieira JEB, Melo EA, Reis AAC. Family health strategy coverage in Brazil, according to the National Health Survey, 2013. Ciênc saúde coletiva. 2016; 21(2):327-38. doi: http://dx.doi.org/10.1590/1413-81232015212.23602015
26.Giovani MSP. Longitudinalidade do cuidado diante da rotatividade de profissionais na Estratégia Saúde da Família. R Eletr de Com Inf Inov Saúde. 2013; 7(4):1-14. doi: http://dx.doi.org/10.3395/reciis.v7i4.866pt
27.Thuler LCS, Bergmann A, Ferreira SC. Teaching in oncological care in Brazil: needs and opportunities. Revista Brasileira de Cancerologia. 2011[cited 2016 Aug 15]; 57(4):467-72. Available from: http://www.inca.gov.br/rbc/n_57/v04/pdf/02_artigo_ensino_atencao_oncologica_brasil_carencia_oportunidades.pdf
28.Yousuf SA, Amoudi SMA, Nicolas W, Banjar HE, Salem SM. Do saudi nurses in primary health care centres have breast cancer knowledge to promote breast cancer awareness? Asian Pacific J Cancer Prev. 2012; 13(9):4459-64. doi: http://dx.doi.org/10.7314/APJCP.2012.13.9.4459
29.Mader EM, Fox CH, Epling JW, Noronba GJ, Swanger CM, Wisniewski AM, et al. A practice facilitation and academic detailing intervention can improve cancer screening rates in primary care safey net clinics. JABFM. 2016; 29(5):533-42. doi: http://dx.doi.org/10.3122/jabfm.2016.05.160109
30.Muhrer JC. Improving breast cancer screening in a federally qualified health center with a team of nursing leaders. The nurse pratcticioner. 2017; 42(1):12-6. doi: http://dx.doi.org/10.109/01.NPR.0000511004.83595.16
31.Andrade ME, Clares JWB, Barretto EMF, Vasconcelos EMR. Nurses' perceptions of their educational role in the family health strategy. Rev enferm UERJ. 2016; 24(4):e15931. doi: http://dx.doi.org/10.12957/reuerj.2016.15931
32.Bertocchi FM, Fernandes BM, Almeida MIG, Freitas SC, Paiva CCN, Paula EA. Professional conduct during breast and uterine/cervical cancer screening consultations. Rev RENE. 2014; 15(6):973-9. doi: http://dx.doi.org/10.15253/2175-6783.2014000600010