(*) minimum wage during the research period = R$ 788.00
ORIGINAL RESEARCH
Characteristics of obese women receiving care from a Family Health Support Unit
Sabrina Bezerra da SilvaI; Rafaella Queiroga SoutoII; Fábia Alexandra Pottes AlvesIII; Tibério Gambarra MoraisIV; Gleicy Karine Nascimento de AraújoV; Mikellayne Barbosa HonoratoVI
I
Nutritionist. Master degree. General Manager of the Hospital e Maternidade
Sinhá Carneiro. Paraíba, Brazil. E-mail: sabrinabs@gmail.com
II
Nurse. Post-PhD. Adjunct Professor, Federal University of Paraíba. Brazil.
E-mail:
rafaellaqueiroga7@gmail.com
III
Nurse. PhD. Adjunct Professor, Federal University of Pernambuco. Brazil.
E-mail:
fabia.alexandra@terra.com.br
IV
Physiotherapist. General Manager of the Hospital e Maternidade Sinhá
Carneiro. Paraíba, Brazil.E-mail: tiberiogm@gmail.com
V
Nurse. Federal University of Pernambuco. Brazil. E-mail: gleicy.kna@hotmail.com
VI
Nurse. Federal University of Pernambuco. Brazil. Brasil. E-mail:
mikellaynebhonorato@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2018.22565
ABSTRACT
Objective: to describe the efficacy of the eating re-education and weight control group of the Family Health Support Center (FHSC) in the city of Santa Luzia, Paraíba. Method: in this community trial, conducted from April to September 2015, participants were evaluated by nutritional consultation and nutritional assessment before and after the educational activities. The population comprised 15 female patients, with body mass index (BMI) above 30 kg/m². Issues such as healthy habits and physical activities were discussed in lectures and conversation circles. Results: significant reduction was observed in participants' BMI (p = 0.000), from 36.22 kg/m² (before the intervention) to 32.94 kg/m² (afterwards), evidencing the importance of the group in improving the quality of users' lives. Conclusion: BMI reduction was satisfactory, underlining the importance of the FHSC team and of maintaining the group.
Descriptors: Obesity; family health; body mass index; primary health care.
INTRODUCTION
The demographic and epidemiological transition currently experienced shows a reduction in infectious diseases and an increase in chronic non-communicable diseases (CNCD), as well as the nutritional transition that reflects in the reduction of malnutrition and the increase of excess weight1. In 2012, about 38 million people in the world died due to consequences of CNCD, of which obesity is one of the greatest risk factors for illness2.
From this perspective, a line of care was developed in primary health care for overweight and other risk factors associated with overweight and obesity, ranging from the reception to the care in specialized services 1.
The person who is overweight may be directed by the Basic Health Unit (BHU) team to a Public Gym Center to perform physical activity and to the Family Health Support Center (NASF in Portuguese) to receive guidance on healthy and balanced eating. The BHU is one of the first contacts to the health system, coordinating the assistance within the system itself2.
The creation of the NASF aimed to broaden the primary care actions, supporting the insertion of the FHS into the service network. It is believed that under the guidance of these professionals and through changes in lifestyle, cases of overweight and obesity can be reversed and prevented, thus preventing or delaying the manifestation of chronic non-communicable diseases associated with overweight3.
Interventions to reverse overweight need to articulate the diverse visions of society about food, physical activity, body and health. The BHU, besides hosting and treating the patient with overweight, should be the care coordinator and communication center among the other units of the Health Care Network (HCN), thus guaranteeing comprehensive care, seeking interdisciplinarity and intersectoriality1.
Another path in the fight against overweight has been the implementation of the strategic action plan for coping with CNCDs, whose purpose is to halt the growth of the proportion of overweight or obese Brazilian adults by 20224.
In this context, the objective of the present study was to describe the comparison of the Body Mass Index (BMI) of patients assisted by NASF in the city of Santa Luzia-PB, before and after their participation in the group of nutritional re-education and weight control.
LITERATURE REVIEW
In Brazil, the prevalence of these data in adults has increased since the surveys conducted in the 1970s. Obesity has increased 60% in 10 years, increasing from 11.8% in 2006 to 18.9% in 20165.
The Brazilian Institute of Geography and Statistics (IBGE) follows the parameters of the World Health Organization (WHO) in the classification of overweight (BMI greater than 25%) and obesity (BMI greater than 30%) 6.
In relation to overweight, it was observed that in 2013, 33.2% of the adult population was overweight and 17.5% was obese. The prevalence of overweight and obesity increased significantly in both sexes, at all educational levels and in all regions, being considered an epidemic in Brazil 7-9.
However, women are a vulnerable group to overweight and obesity due to the transition of the phases experienced throughout the life cycle from the menarche, pregnancy-puerperal and climacteric periods10,11. In spite of this, studies point out that the female sex has a greater predisposition to decrease body weight and, mainly due to the influence of the current society, in the perception of the body image, seeking to adapt to the lean and ideal bodies to which they are imposed12. In line with this, most women with obesity or overweight report not being satisfied with their body image13.
BMI values between 25 and 30 account for most of the impact of overweight on certain comorbidities associated with obesity. A survey found that about 36.6% of men and 62.9% of obese women had between two or three comorbidities. The female population stood out, since 80% of them presented Diabetes Mellitus (DM) and could, theoretically, prevent the disease if they had a BMI less than or equal to 2514.
Despite the change in the search for healthy habits of the Brazilian population, the levels of obesity and overweight are still worrisome in the country. Results show that one in five Brazilians are obese and 54% of the population of the Brazilian capitals are overweight. In fact, the prevalence of the disease increased from 11.8% in 2006 to 18.9% in 2016 15. This increase in obesity may have influenced the increase in the prevalence of comorbidities, especially hypertension and diabetes16.
METHODOLOGY
This is a community trial with a quantitative approach. A trial is defined as a study where the participants can be evaluated after accomplishing interventions17. The study was developed in the NASF of the city of Santa Luzia, from April to September 2015.
For the selection of the sample, all users with the following characteristics were referred by the FHS to the NASF: BMI above 30 kg/m² and the condition of being invited to participate in the group of nutritional re-education and weight control. Twenty-two participants were included, however, seven dropped out due to schedule mismatch, resulting in a final sample of 15 participants.
Data collection was done through a consultation and nutritional evaluation before and after the accomplishment of educational activities. Socioeconomic information (age, sex, profession, marital status, housing and income) was collected in order to characterize the population.
For the nutritional evaluation, the weight and height of the volunteers were verified. The weight gain was measured in kilograms using a 0.1 kg Filizola platform scale, with the patient unadorned and without shoes. To verify the height, measured in centimeters, an anthropometric ruler with an accuracy of 0.1cm was fixed on the scale, and for this purpose, the patient was asked to stand erect and with legs and heels together, arms positioned along the body and look at the horizon without hyperextension of the spine.
For the calculation of BMI, the formula (weight in kg divided by the square of height in meters) was used to assess the nutritional status according to the WHO.
The data collected were entered in the Microsoft Excel program version 97-2003 and imported into SPSS version 20, where they were analyzed through descriptive and inferential statistics.
To evaluate the impact of the nutritional re-education group on the nutritional status of the participants, that is, whether there was a significant reduction of BMI, the Student's test was performed for paired samples, since the same individuals were evaluated at two different times. For the application of the test, it is assumed that the samples follow a normal distribution and, for this purpose, the tests of Kolmogorov-Smirnov and Shapiro-Wilk were performed.
In addition, confidence intervals were constructed for the sample mean, considering the continuous quantitative variables. For all tests, a confidence level of 95% was set.
Weekly meetings were held between April and September 2015, totaling 17 meetings, lasting one hour each, aiming to work on eating habits and healthy habits. From this, the focus of the interventions was on an awareness about healthy eating and physical activity, through discussion of themes related to motivation and self-perception, with dynamics and group therapy.
This study was approved by the Research Ethics Committee of the Health Science Center (CCS) of the Lauro Wanderley University Hospital of the Federal University of Paraíba (UFPB), through the protocol number 41786615.9.0000.5183. Resolution 466 of December 12, 2012 was followed, in which the National Health Council (CNS) approved the guidelines and regulation of research involving human beings, seeking to guarantee the rights and duties that concern the scientific community, the research participants and the State.
Before the data collection, the purpose of the research was explained to the users, and the Informed Consent Form (ICF) was presented, highlighting the freedom of participation and the guarantee of anonymity.
RESULTS AND DISCUSSION
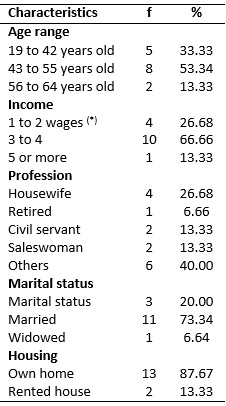
The population is composed of 15 women, with BMI over 30 kg/m². More than half - 8 (53.34%) - of the respondents presented age between 43 and 55 years, while only 2 (13%) reported age over 55 years. Most of the women were married - 11 (73.3%)-, and had their own home - 13 (86.6%). Considering the frequency distribution for the income variable, it was found that 7 (46.7%) patients receive 3 minimum wages, while only 4 (26.7%) receive less than 3 wages, as described in Table 1.
TABLE 1: Socioeconomic characteristics of study participants. Santa Luzia,
PB,2015. 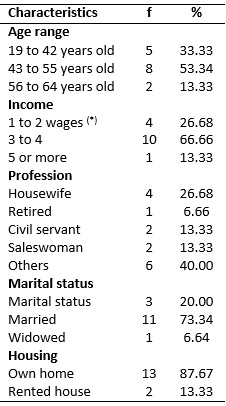
(*) minimum wage during the research period = R$ 788.00
It is in the younger strata of the population that measures aimed at behavioral changes can have greater effect, so the age group between 10 and 19 years is considered the most effective for the concentration of efforts directed to combat overweight and obesity18.
Regarding the income factor, in developing nations, such as Brazil, there is a relationship between obesity and the highest socioeconomic level. This fact is due to the existence of a greater availability of foods with greater energy density and the little practice of physical activity in this socioeconomic profile2.
Being single, separated or widowed, that is, not being engaged in a more stable relationship, seems to protect the woman from nutritional disorders, compared to married women or in marital union, who presented a greater risk of being obese19.
Regarding the interventions, after the presentation of the group for nutritional re-education and the NASF team, three meetings were held in which themes such as self-perception, nutritional taboos and daily physical activity were addressed through lectures, orientations and group dynamics.
In the subsequent meetings, the difficulties encountered were discussed, through a round of conversation, in addition to expository and dynamic lectures. The themes discussed were imposition of personal limits, importance of posture and its influence on health, preparation of healthy food and recipes, favoring of self-esteem, and building of healthy behaviors.
During the workshops, posters were produced, in which the participants expressed their feelings and their expectations about the development of the group. Most were anxious about being overweight and expected weight reduction and biochemical rates. Guiding activities were adapted to the group's reactions, making it possible for them to participate in a dynamic and conscious way.
Regarding the descriptive and inferential results of the comparison of the initial and final BMI of the participants, it is worth noting that there was a reduction of the final BMI, according to Table 2.
TABLE 2: Comparison of the BMI of the participants before and after the
educational activities. Santa Luzia/PB, 2015
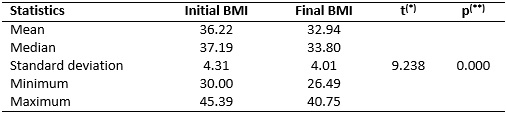
(*)
Student's t test
(**)
significance level of the test
The mean BMI before participation in the group was 36.22 kg/m2, with a standard deviation of 4.31 kg/m2. In addition, the median BMI reached 37.19 kg/m2, indicating that 50% of the population of interest has a BMI greater than or equal to this value. Thus, it is possible to verify that more than half of the population was initially classified in obesity grade II or obesity grade III according to WHO classification.
According to the BMI classification of the patients, considering the two periods in which the measurements were taken, it was verified that, before their participation in the nutritional re-education group, 7 (46.6%) of the patients were classified by the WHO criteria as severely obese and 6 (40.0%) with moderate obesity. After re-education of eating habits through the group, a substantial reduction in obesity cases was observed, with 5 (33.3%) patients with severe obesity and 4 (26.6%) with moderate obesity. Also, 5 (33.33%) patients were no longer classified with some type of obesity, proving the effectiveness of the group work in improving patients' quality of life.
After participation in the re-education group, there was a reduction in the BMI of the patients when compared to the initial BMI, from 36.22 kg/m2 to 32.94 kg/m2. The mean final BMI was 33.80 kg/m2, while the minimum and maximum were, respectively, 26.49 kg/m 2 and 40.75 kg/m2, values lower than those obtained in the first measurement. See Table 2.
Based on the t-test result, a 95% confidence level indicates that there was a statistically significant reduction (p = 0.000) in the mean BMI of patients assisted by the NASF. The importance of the educational practices of the nutritional re-education group to change the dietary habits of the investigated patients was evidenced, consequently implying the improvement of their quality of life. The effectiveness of health education is due to the fact that it is a continuous process that aims to promote health, based on the participation of users20.
In this way, collective educational practices allow the knowledge of the causes and consequences of obesity, contributing to the active participation of users of basic health care services. Therefore, the health team must work in a significant way in health education aiming at the prevention and control of excess weight and its consequences.
With the increase of obesity worldwide, changes in lifestyles and healthy habits are themes that have been addressed on in all age groups in the health area and in different environments, such as in companies, schools and day care centers. These practices have achieved great results with respect to the physical and mental health of the practitioners and, consequently, in their quality of life21.
In the short term, there was a good adaptation by participants in relation to the need to change their lifestyle, regarding the practice of physical activities and healthy eating habits.
These actions tend to present satisfactory results and can promote a significant improvement of the quality of life and reduction in obesity indices. Nutritional monitoring can serve as a tool for reducing body weight and consequently reducing the risks associated with obesity and improving quality of life22.
A study showed that more than 80% of obese women, to any degree, were dissatisfied with their body image. Despite the high level of dissatisfaction, only 30% of the women with obesity took some action to reduce the weight, such as diet, physical activity or use of medicines 23. The perception of the obese body in the woman can cause a thought of loss of the previous world, banalization of everyday life and exclusion of prospects for a better future24.
To further reduce the loss of BMI, the group should be monitored in the long term, mainly to achieve the ideal weight. Given this, group prevention activities are useful, highlighting the fact that clients have demonstrated a good understanding of the guidelines, valuing the information they received.
CONCLUSION
The results showed a significant reduction of BMI after the participation of women in the NASF group, reinforcing the need to maintain the nutritional re-education group and the importance of the participation of the NASF team in primary health care.
The results of the interventions were satisfactory because they presented positive changes in the clients' lifestyles, improving well-being in general. All of them showed an interest in the themes addressed, participating in the sharing of their anguish and individual difficulties and the overcoming of daily activities.
Prevention and health promotion actions aimed at people with obesity are beneficial, mainly because the population often does not have immediate treatment and close monitoring available. For this reason, there should be a comparison of the data recorded at the beginning and after the educational actions developed.
Health professionals have great challenges in working with this demand, so it is important to value intervention groups. They facilitate the achievement of the effectiveness of health promotion, favoring the prevention of health problems, promoting the motivation and the well-being of users with obesity.
This study should be performed in other contexts, allowing this to be an alternative intervention to be implemented by the health team to reduce BMI. In addition, longitudinal studies with larger populations should be conducted, thus overcoming the limitations of the present study.
REFERENCES
1. Ministry of Health (Br). Strategies for care of the person with a chronic disease: obesity. Brasília (DF): Publisher MS; 2014.
2.Gonçalves RMDA, Lancman S, Sznelwar LI, Cordone NG, Barros JDO. Study of the work in Family Health Support Centers (NASF), São Paulo, Brazil. Rev. bras. saúde ocup. 2015; 40(131): 59-74.
3.Pedraza DF, Menezes TN, Costa GMC. Food and nutrition actions in the family health strategy: structure and work process. Rev. enferm. UERJ. 2016; 24(4): e15848.
4.World Health Organization. Obesity preventing and overweight. Report of a WHO Consultation on Obesity. Geneva (SWI): WHO; 2015.
5. Brazil (Br). Ministry of Health. Vigitel Brasil. Habits of Brazilians impacting on the growth of obesity and increase of prevalence of diabetes and hypertension. 2016. [Access in Aug 15, 2018]. Available from: http://portalarquivos.saude.gov.br/images/pdf/2017/abril/17/Vigitel.pdf
6: World Health Organization. Obesity preventing and overweight. Report of a WHO Consultation on Obesity. Geneva (SWI): WHO; 2015.
7.Campos DA, Vieira M, Pires ROM. Evaluation of the work process of nutritionists of the Family Health Support Centers in the Midwest of Santa Catarina. Saúde transform. soc. 2017; 8(1): 84-97.
8.Santos MC, Frauches MB, Rodrigues SM, Fernandes ET. Work process of the Family Health Support Centers (NASF): importance of professional qualification. Saúde transform. soc. 2017; 8(2): 60-69.
9.Malta DC, Santos MAS, Andrade SSCDA, Oliveira TP, Stopa SR, Oliveira MMD, Jaime P. Temporal trend of overweight indicators in adults in Brazilian capitals, 2006-2013. Ciênc. saúde coletiva (Online). 2016; 21(4): 1061-69.
10. Ferreira RAB, Benicio MHDA. Obesity in Brazilian women: association with parity and socioeconomic status. Rev. Panam. Salud Publica. 2015; 37(4/5): 337–42.
11.Pereira DCL, Lima SMRR. Prevalence of overweight and obesity in postmenopausal women. Rev. eletrônica acervo saúde. 2018; 60(1): 1-6.
12.Agra G, Araújo LLLM, Pessoa VVB, Justino Filho J, Freire MEM, Formiga NS. Perception of obese women in relation their body. Revista Ibero-Americana de Saúde e Envelhecimento (Online). 2016 [Access in Aug 15, 2018]; 2017; 2(3): 775-93. Available from: http://www.revistas.uevora.pt/index.php/saude_envelhecimento/article/view/147/329
13. Poltronieri TS, Tusset C, Gregoletto MLO, Cremonese C. Dissatisfaction with body image and associated factors in women from southern Brazil. Rev. ciência & saúde. 2016; 9(3): 128-34.
14.Silveira EA, Vieira LL, Souza JDD. High prevalence of abdominal obesity in the elderly and association with diabetes, hypertension and respiratory diseases. Ciênc. saúde coletiva (Online). 2018; 23(3): 903-12.
15. Ministry of Health (Br). National Policy for Food and Nutrition. Brasília (DF): Ministry of Health; 2013.
16.Brischiliari SCR, Agnolo CMD, Gravena AAF, Lopes TCR, Carvalho MDB, Pelloso SM. Chronic non-communicable diseases and association with risk factors. Rev. bras. cardiol. 2014; 27(1): 35-42.
17. Rouquayrol MZ, Gurgel MCS. Epidemiology & Health. 7th ed. Rio de Janeiro: Editora Med Book; 2013.
18. Castro JM, Ferreira EF, Silva DC, Oliveira RAR. Prevalence of overweight and obesity and the risk factors associated in adolescents. Rev. bras. obesidade, nutrição e emagrecimento. 2018; 12(69): 84-94.
19. Mais LA, Domene SMÁ, Barbosa MB, Taddei JADAC. Formation of food habits and promotion of health and nutrition: the role of the nutritionist in the Family Health Support Centers –NASF. Rev. APS. 2016; 18(2): 248-55.
20.Falkenberg MB, Mendes TDPL, Moraes EPD, Souza EMD. Education in health and health education: concepts and implications for collective health. Ciênc. saúde coletiva (Online) 2014; 19(3): 847-52.
21.Ferrari TK, Cesar CLG, Alves MCGP, Barros MBDA, Goldbaum M, Fisberg RM. Healthy lifestyle in São Paulo, Brazil. Cad. Saúde Pública (Online). 2017; 33(1): e00188015.
22.Souza ACB, Oliveira JED, Caritá EC, Almeida CAN. Profile of obese patients in the first attendance at the Municipal Nutrition Clinic of Ribeirão Preto (SP). Medicine (Ribeirão Preto). 2017; 50(4): 207-15.
23.Figueiredo MD, Cunha DR, Araujo AIG, Santos CM, Suplicy HL, Boguszewski CL,et al.. Food behavior and psychological profile of obese women. Rev. PsicoFAE. 2014; 3(1): 43-54.
24.Oliveira V, Santos M, Andrade N, Teixeira C, Rodrigues F, Zanetti M. The perception of the body by women with diabetes mellitus and obesity. Rev. enferm. UERJ. 2014; 22(2): 251-7.