ORIGINAL RESEARCH
Costs of Chronic Patient Management Program in a healthcare provider organization
Sarah Lopes SilvaI; Ana Clara TolentinoII; Luis Carlos SantiagoIII; Cristiano Bertolossi MartaIV; Antônio Augusto de Freitas PeregrinoV; Vivian SchutzVI
I
Master student in nursing, Federal University of Rio de Janeiro. Brazil.
E-mail: enfasarah@gmail.com
II
PhD student in nursing, Federal University of the State of Rio de Janeiro.
Brazil. E-mail:
anaclaratolentino@gmail.com
III
Post Doctor. Adjunct Professor of the basic nursing department of the
Federal University of the State of Rio de Janeiro. Brazil. E-mail: luisolitrio@yahoo.com.br
IV
Post Doctor in nursing. Adjunct Professor, Department of Nursing
Fundamentals, University of the State of Rio de Janeiro. Brazil. E-mail: cristianobertol@gmail.com
V
PdH in public health. Associate Professor of the Radiological Sciences
Laboratory of the University of the State of Rio de Janeiro Brazil. E-mail: antoniop@uerj.br
VI
PhD in Nursing. Adjunct Professor, Department of Nursing Fundamentals of
the University of State of Rio de Janeiro. Brazil. E-mail: vshutz@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.21937
ABSTRACT
Objective: to analyze the cost-containment strategy for multiple avoidable hospitalizations in a program of Chronic Patient Management (GDC), since its implementation in a health care provider organization. Method: this is a retrospective study with quantitative approach in which a survey was conducted with data obtained through monitoring of 243 patients assisted by the program from 2009 to 2012. Approved by Research Ethics Comitee (CAAE: 34525614.8.0000.5285). Results: in the case of basic conditions, most patients possessed more than one installed disease. Regarding the costs of emergency hospitalization in the year before GDC was BRL 1,323,295.43 and the subsequent year BRL 629,565.89. It was possible to observe how expensive were the patients who presented pathologies that could be avoided. Conclusion: it was concluded that an efficient management in health allows profesionals to offer services in order to a greater number of users with no prejudice to the operators, especially when allocated to preventive actions.
Keywords: Cost and cost analysis; supplemental health; chronic disease; aging.
INTRODUCTION
Brazil has undergone an epidemiological transition in recent decades, characterized by an increase in chronic-degenerative diseases and a decline in infectious and parasitic diseases as a result of advances in health sciences and technologies. This change in the health profile significantly contributes to the reduction of mortality, which leads to longer life expectancy of the brazilian population1-3.
Estimates indicate that by 2050, the world's population over the age of 60 will be about two billion people. This will occur as a result of the change in health indicators related to the fall in fertility and mortality rates as opposed to increased life expectancy4.
Population aging brings as a consequence the rise of chronic diseases, which have slow and persistent evolution. As significant health costs around the world are required for their complex and long-term treatment, interfering in public and private budgets, they have been the cause of concern to many health managers. According to World Economic Forum , between 2011 and 2030, economic losses generated by chronic non-communicable diseases will be up to 47 trillion dollars, representing 5% of the gross global product of that period. The situation will not be different in Brazil; 4.18 billion US dollars are expected to be spent on diabetes, cardiovascular disease and cerebrovascular accident by 20155,6.
Among the chronic diseases that most affect the elderly population are cardiovascular diseases, chronic obstructive pulmonary diseases (COPD) and Diabetes Mellitus (DM). These may be related not only to the aging process, but also to life habits such as smoking and alcohol consumption, diet, physical inactivity, and genetic predisposition. However, these diseases do not affect only the elderly population and rich countries nowadays, but also the young and middle-aged people living in developing countries6,7.
Currently, efforts have been put on the adoption of health promotion and healthy aging programs. The Ministry of Health included the health of the elderly as a priority in the country's health system. Through Normative Resolution nº 265, the National Supplementary Health Agency (ANS) encourages the participation of health plan users in active aging programs. However, the focus on assistance is still predominant and a challenge to be constantly overcome2,8.
On the other hand, there are patients with already installed pathologies. Chronic diseases do not regress. Thus, their progression should be slowed down so as to prolong the expectancy of active life. In this context, a program to care for the elderly and their multiple associated pathologies is necessary, through management groups of patients with chronic diseases 8.
This study aimed to analyze the cost containment strategy for multiple avoidable hospitalizations. This strategy was adopted by a self-managed health care provider after the implementation of the chronic patient management (CPM) program. This program was implemented in 2009 and, since then, has undergone constant changes. The objective is to answer the following question: Was there any reduction in the costs generated by patients followed by this program one year after its implementation?
The target audience of this program corresponds to patients with chronic degenerative diseases such as COPD, DM, systemic arterial hypertension (SAH), coronary artery disease (CAD), dyslipidemia (DLP), and congestive heart failure (CHF). The criteria for inclusion of patients were to have at least one of the aforementioned pathologies and to have been hospitalized because of these diseases.
These patients are monitored by a multidisciplinary team through pre-scheduled telephone calls, according to the degree of complexity of the disease, which may be mild, moderate or severe. These calls may happen quarterly, monthly or biweekly, respectively. This monitoring is done by an outsourced company that passes the reports according to the agreed periodicity. The health insurance provider, on its part, pays a fee per capita, per associate, according to the degree of complexity described above.
LITERATURE REVIEW
The complementary health market in Brazil is subdivided into insurers, cooperatives, group medicines and self-management companies. These correspond to a non-commercial and, therefore, non-profit segment of health care and in some cases are sponsored by employers. The logic of the market is not applied in the case of these companies because they do not aim at profits, and the revenues are reverted to the costing of the activity itself9.
Health care costs have increased exponentially, culminating in a scarcity of available resources, which places the paying sources, public or private, in a delicate situation. Managerial knowledge is, therefore, necessary to contribute to restriction of costs and efficient allocation of resources in order to maintain the financial balance of health care providers in face of this situation10,11.
Given this scenario, it is critical that health sector managers focus on creation of values and not just on cost cutting. The adoption of preventive measures and a comprehensive management program is, thus, fundamental to reduce the risk and the worsening of diseases. Studies show that it is possible to obtain a return of 2.9 US dollars for every dollar invested into chronic disease management and prevention1.
Some companies, currently, have started programs of attention to chronic patients in the attempt to control costs, with the intention of identifying and following patients regularly. However, there are few published studies showing the benefits of these programs in terms of costs.
These programs aim to identify individuals with chronic pathologies of high care risk, acting in the prevention of their worsening by involving patients and their families in the care, and generating a database on these patients. The proper definition of action and the ability of the multidisciplinary team responsible for this program is of extreme importance for its success1.
METHODOLOGY
This is a descriptive study with quantitative approach. To solve the question, data obtained through the monitoring of patients assisted by the CPM program since 2009 was surveyed. This was done through the analysis of the database of a private self-management company, located in the state of Rio de Janeiro. The management of this program underwent changes in 2013. Data collection occurred between November and December 2014.
The program was launched in 2009 with the participation of 78 members whose selection was based in the history of hospitalizations and baseline pathologies. New members were progressively included in the program, based on the researches of hospital visits and hospitalizations of patients with the aforementioned baseline pathologies. In the first half of 2010, 10 new members were included; in the second half of 2011, 30 new patients were included; and in 2012, 71 in the first semester and 61 in the second were included, totaling 250 members.
A new search for members is currently occurring through identification of patients with multiple hospitalizations and patients with underlying diseases. However, the new associates are not eligible for the present study because they do not have a year enrolled in the program.
The inclusion criteria were: patients who were followed up by the program at the time of data collection and who had completed 12 months of adherence to the program.
During the follow-up period, seven associates were disconnected from the CPM program and were excluded from the study. The population was composed of 243 participants, which represents all members of the program. It is worth mentioning that this program is of national scope and, therefore, counts on associates from all regions.
In order to meet the objectives of this study, the following steps were taken:
Data were organized in the Microsoft Access 2007® and entered into tables.
It is worth mentioning that access to the database was authorized by the director of the social security and assistance, who signed an agreement term. There was no need to involve the Ethics Committee because the study did not present risk to the subjects involved neither exposed their identities.
RESULTS AND DISCUSSION
The patients started being monitored at the moment they were inserted in the chronic patient group, when they received a classification related to their most serious baseline disease. This evaluation led to their allocation in each group.
Regarding the classification by groups, 178 (73.2%) belonged to group 1, 57 (23.4%) to group 2 and 8 (3.2%) to group 3, totaling 243 associates. During the annual follow-up, 4 (1.6%) evolved to death, 3 (1.2%%) improved, and seven patients were excluded from the study.
Data in the literature point to theoretical models applied to the elderly according to their degree of dependence and complexity, for stratification into four levels. This stratification guides the actions to be employed in each group, in the health promotion and disease control programs. These models follow the logic that these individuals must be permanently monitored under the respective periodicity of the group to which they belong2.
As for sex, there was not much difference between the prevalence of men and women, being 53% women and 47% men. With respect to age group, the majority of members were aged between 61 and 80 years (67%) followed by those over 80 years (20%). This was expected because these are patients with chronic diseases that have higher prevalence among the elderly.
With regard to pathologies, most patients had more than one disease. They had the following diseases: hypertension (93%), dyslipidemia (51%), DM (47%), COPD (42%), CAD (5%) and CHF (4%).
Hypertension represents one of the major causes of reduced expectation and quality of life and is directly related to the development of cardiovascular diseases, accounting for 25% of the multifactorial etiology of ischemic heart disease and 40% of strokes. In Brazil, cardiovascular diseases are the leading cause of hospitalization in the public sector and account for 33% of deaths by known causes. Most of these diseases occur as an outcome of patients with mild risk factors, without the proper treatment, such as hypertensive patients12-14.
In 2010, DM affected 6.4% of adults between 20 and 79 years and, in 2008, this disease was responsible for 1.3 million deaths worldwide. In Brazil, this scenario is no different, with 54,800 deaths occurring in a contingent of 6 million people. Linked to the high prevalence of DM patients, a growing increase in hospitalizations due to this disease has been observed when compared to others15,16.
Among diseases, COPD is characterized by chronic and progressive obstruction of the expiratory flow and is associated with exposure to tobacco and environmental pollutants in addition to climatic variations. In Brazil, this disease represents the third cause of death due to chronic non-communicable diseases, with an estimated annual mortality of 40,000. In 2011, the Unified Health System recorded a cost of 103 million Reais linked to 142,635 hospitalizations for COPD17.
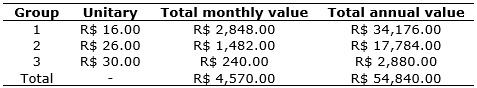
The company that provides services has a monthly follow-up cost, per member, according to the group to which they belong. As for profile of the associates, the majority were in group 1.It is worth mentioning that although the value per member is lower in group 1, the final cost with this group is higher in relation to the others, as shown in Table 1.
TABLE 1: Cost (in Brazilian Reais) of the program incurred to the company
by group of associates. Rio de Janeiro, 2014.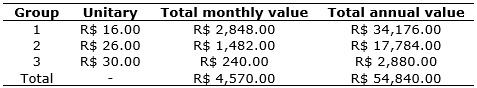
In order to assess costs, individuals were separated into groups according to the period when they were inserted in the program. The sum of the annual cost of individuals of each group and data obtained were organized in Table 2.
TABLE 2: Total cost (in Brazilian Reais) for hospitalizations and number of
hospital visits. Rio de Janeiro, 2014. 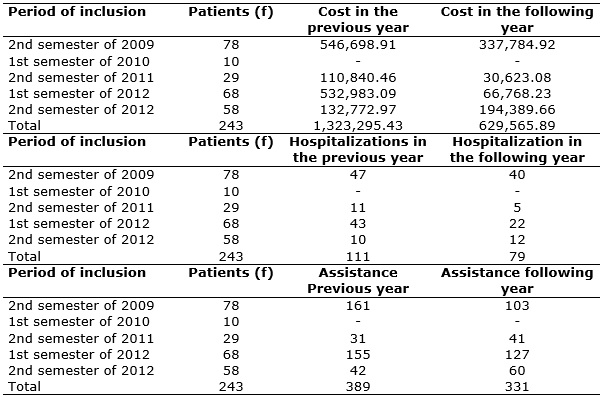
The compiled data shows that there was a reduction of approximately 52% of hospitalization costs in the following year. The sum of the cost after implementation of the program (R$ 629,565.89) and the cost of maintaining it (R$ 54,800.00) reaches the total amount of R$ 684,365.89, which represents the cost of hospitalization plus the cost of the program. Therefore, the total percentage of reduction in costs, based on this corrected value, was approximately 48%. See Table 2.
Of the total number of members, only 17 (7%) had a higher hospitalization cost in the year after treatment, that is, 226 (93%) patients had a reduction in costs.
Regarding the number of hospitalizations, there was also a reduction in the year after the CPM program. In the year prior to inclusion, the 243 associates had a total of 111 hospitalizations and in the subsequent year that number was reduced to 79, as shown in Table 2.
In addition to obtaining data related to hospitalization costs and the number of hospitalizations, the numbers of urgency and emergency care events were identified. These represent another sink of resources of health care providers with decompensated chronic patients were also identified, who are not properly followed up, as observed in Table 2.
In the respective year prior to inclusion of members in the CPM program, the total number of urgency and emergency care events was 389 and, in the subsequent year, the number was 331. It is noteworthy that in both groups there was an increase in the number of hospital visits, despite the follow-up by the CPM program. When analyzing each data separately, it was found that the increase was randomized and pulverized in the several associates.
CONCLUSION
The management of chronic patients represents an important tool for the efficient management of financial resources in health, so scarce nowadays. The data demonstrated the high costs of patients who presented preventable pathologies and how significant was the reduction in costs with hospitalizations for the health care provider, as well as the reduction in the number of urgency/emergency care events and hospitalizations, as a result of the implementation of this program.
In view of the aforementioned facts, it is evident that efficient health management makes it possible to offer health services to a larger number of users without burden to companies, especially when allocated to actions involving prevention.
The time of follow-up of associates and the change in the company providing the service during the follow-up period must be considered as limitations of this study.
Further studies are needed to verify the adequacy of this practice in other types of users, such as in the public health system.
REFERENCES
1.Veras RP. Management of chronic disease: misconception for the age group of the elderly. Rev Saude Publica. 2012; 46(6):929-34.
2.Daros RF, Gomes RS, Silva FH, LOPES TC. Satisfaction of complementary health members from the perspective of quality and comprehensiveness. Physis [online]. 2016; 26(2), 525-47.
3.Sousa SPO, Branca SBP. Epidemiological overview of the aging process in the world, Brazil and Piauí: evidence in the literature of 1987 to 2009. Enfermagem em Foco. 2011; 2(3):188-90.
4.Ministry of Health (Br). Department of Health Care. Department of Primary Care. Ageing and Health of the Elderly. Brasília (DF), 2006. [cited in March 05, 2016]. Available at http://189.28.128.100/dab/docs/publicacoes/cadernos_ab/abcad19.pdf
5.Silva LS, Cotta RMM, Rosa COB. Strategies for health promotion and primary prevention for coping with chronic diseases: a systematic review. Rev Panam Salud Publica. 2013; 34(5): 343-50.
6.Veras RP. Strategies for coping with chronic diseases: a model in which all are benefited. Rev Bras Geriatr Gerontol. 2011; 14(4): 779-86.
7.Pimenta MA, Castanheira CHA, Lana FCF, Malta DC. Prevention risk actions and diseases in the complementary sector. Rev Min Enferm. 2012; 16(4): 564-71.
8.Gerschman S, Ugá MAD, Portela M, Lima SML. The role required of the Complementary National Health Agency in regulating health plans and service providers. Physis Rev of public health. 2012; 22(2): 463-76.
9.Freitas RM, Cherchiglia ML, Lana FCF, Malta DC, Andrade EIG. Study of the care models practiced by private health plan companies. Physis Collective Health Magazine. 2011; 21 (4): 1561-77.
10.Lima AFC, Castilho V, Fugulin FMT, Silva B, Ramin NS, Melo TO. Costs of the most frequently nursing activities performed in highly dependent patients. Rev Latino-Am Nursing. 2012 [cited in March 05, 2016]. 20(5): 880-7. Available at: http://www.revistas.usp.br/rlae/article/view/48627/52668
11.Martins AVF, Peter MGA, Machado MVV, Catrib AMF. Strategies for reducing costs in health insurance providers. Rev of Accounting Information. 2013; 7(1): 55-72.
12.Marta CB, Leite JL, Peregrino AAF, Schutz V, Francisco MTR, Magnago C. Costs of adherence to the treatment of acquired immune deficiency syndrome: cross-sectional study. Rev nursing UERJ. 2014; 22(2):193-9.
13.Silva SSBE, Oliveira SFSB, Pierin AMG. The control of hypertension in men and women: a comparative analysis. Rev Esc nursing USP. 2016; 50(1):50-8.
14.Pinto NBF, Vieira LB, Pereira FMV, Reis AMM, Cassini SHDB. Drug interactions in prescriptions of elderly hypertensive patients: prevalence and clinical significance. Rev nursing UERJ. 2014; 22(6):735-41.
15.Malta DC, Iser BPM, Andrade SSCA, Moura L, Oliveira TP, Bernal RTI. Trend of the prevalence of self-reported diabetes mellitus in adults in the Brazilian capital, 2006-2012. Rev Epidemiol Health Serv. 2014; 23(4): 753-60.
16.Petermann XB, Machado IS, Pimentel BN, Miolo SB, Martins LR, Fedosse E. Epidemiology and care for Diabetes Mellitus practiced in Primary Health Care: a narrative review. Health, Santa Maria. 2015; 41(1): 49-56.
17. Rabahi M. Epidemiology of COPD: facing challenges. Rev Lung RJ. 2013; 22(2): 4-8.