ORIGINAL RESEARCH
Non-invasive technologies in obstetric nursing care: effects on newborn vitality
Octavio Muniz da Costa VargensI; Carlos Sérgio Corrêa dos ReisII; Maria de Fátima Hasek NogueiraIII; Juliana Amaral PrataIV; Carla Marins SilvaV; Jane Márcia ProgiantiVI
IRN. RNM. PhD. Professor of Nursing at the Nursing Faculty of Rio de Janeiro
State University, Brazil. E-mail: omcvargens@uol.com.br
IIRN. RNM. PhD. Assistant Professor at the Nursing Faculty of Rio de Janeiro
State University, Brazil. E-mail: carlosreis.prof@gmail.com
IIIRN. RNM. PhD. Adjunct Professor of Nursing at the Nursing Faculty of Rio de
Janeiro State University, Brazil. E-mail: fatimahasek@gmail.com
IVRN. RNM. PhD. Assistant Professor at the Nursing Faculty of Rio de Janeiro
State University, Brazil. E-mail: juaprata@gmail.com
VRN. RNM. PhD. Adjunct Professor of Nursing at the Nursing Faculty of Rio de
Janeiro State University, Brazil. E-mail: carlamarinss@hotmail.com
VIRN. RNM. PhD. Associate Professor of Nursing at the Nursing Faculty of Rio
de Janeiro State University, Brazil. E-mail: jmprogi@uol.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.21717
ABSTRACT
Objective: to compare the association between Apgar scores of neonates whose mothers used only non-invasive obstetric nursing care technologies during labor and those whose mothers received traditional care. Method: in this retrospective, cross-sectional study of 6,790 records of childbirth attended by obstetric nurses between September 2004 and December 2011, logistic regression was used to assess the likelihood that exposure to these non-invasive technologies contributed to better Apgar scores as compared with other types of care. Results: neonates whose mothers used any of these non-invasive technologies returned higher percentage Apgar scores, in both the 1st (93.41%) and 5th minute of life (99.01%), as compared with those whose mothers underwent traditional care procedures (82.78% and 94.74%, respectively). Conclusion: the Apgar score odds ratio of > 8 is increased in favor of those who used only non-invasive obstetric nursing care technologies.
Keywords: Obstetrical nursing; humanized childbirth; new-born; Apgar score.
INTRODUCTION
In the hospital environment, despite all the discussion regarding the care provided to the parturient and the newborn, it is also verified the predominance of the adoption and incorporation of medicalized obstetrical practices1. These practices are based on the technocratic care model, for which the parturition process must occur in the hospital environment, being controlled by the health professional with the use of procedures considered invasive or often painful interventional behaviors that cannot be refused by the parturient2.
Several factors such as strict routines, intense medicalization, unnecessary and potentially iatrogenic interventions, abusive cesarean delivery, isolation of the pregnant women from their families, lack of privacy and disrespect for their autonomy and rights, among other factors, contribute to increase maternal and perinatal risks. These risks, most of the times, can be reduced through a better follow-up of the parturient3,4. On the other hand, practices and care that are proven adequate, recommended by the World Health Organization since 19965 and adopted by the Ministry of Health (MS - Ministério da Saúde)6 for the childbirth follow-up are not usually employed, encouraged and respected.
With the intention of transforming this reality and looking forward to the decrease in the rates of maternal and perinatal morbidity and mortality, many government and non-governmental organizations have submitted proposals for the return of the childbirth as a physiological process whose care centered on the well-being of the woman and her child. Thus, the humanistic care model is being perceived as the healthiest and safest way of giving birth and being born.
It is important to highlight, in this context, that such conception of care for pregnant women at usual risk extended in a similar and significant way to the care of newborns (NB) also at usual risk. Since then, several behaviors have been instituted, also performed routinely, as observed in the conduct of labor and delivery. In today's traditional hospitals, the care provided for the newborn is marked by the tumultuous, noisy, cold, high-luminosity environment and the early large-scale use of invasive procedures that may influence the vitality of the newborn7.
In this humanistic model8the human body is seen in a natural way and the delivery is considered a physiological event, the woman who is experiencing it must be respected in its biological, social, spiritual, cultural and psychological aspects and its child must be seen as a social being.
Based on these premises, non-invasive obstetrical nursing care technologies (NIONCT) and their use as a strategy for the de-medicalization and humanization of the delivery care were presented. These are defined as all the techniques, procedures and knowledge used by the nurse during the process of caring for the woman, whose main characteristic is to be non-invasive, allowing the woman to use her instinct and become the protagonist at the time of delivery9. They presuppose the shared decision in care planning, and the establishment of a bond of trust between the professional and the subject. Thus, invasion does not exist, even when the procedures touch intimate or internal parts of the biological body or the sociocultural body of the woman10.
These technologies have been used in some municipal maternity hospitals in Rio de Janeiro and there was the need to assess the repercussion of their use on the vitality of newborns, since there are no publications in the literature with research results that perform this assessment. Thus, the present study was developed with the objective of analyzing, through the assessment of the Apgar Index in the first and fifth minutes, the effects of non-invasive technologies of obstetric nursing care used in the care of the parturient on the vitality of the newborn.
It was hypothesized that the use of NIONCT during labor and delivery accompanied by obstetric nurses was not a risk factor for the impairment of the vitality of the newborn (Apgar indexes> 8 in the first and fifth minutes of life).
Since its creation in 1953, the Apgar Index (AI), established by scoring the child's vitality at birth, has been widely and universally adopted and used by health professionals caring for the neonate in the most diverse birthplaces of the world. In addition, over the years it has been extended to assess the behavior related to obstetrical practices, and its repercussion for the fetus and/or newborn11.
METHOD
Cross-sectional, retrospective, documentary study carried out in a maternity hospital in Rio de Janeiro, a reference for pregnant women at usual risk, whose mission is to encourage normal and humanized delivery.
The documentary universe consisted of 10,675 records of deliveries monitored by obstetric nurses between September 2004 and October 2016. The sample, in this study, was composed of 6,790 birth records from September 2004 to December 2011, corresponding to the first stage of the proposal to encourage normal and humanized delivery through the implantation of delivery care by nurses in the maternity ward studied. The source of information was the Book of Birth Records (BBR) in the obstetric center of the institution. The data were typed in an electronic instrument and stored in a database using the Epi-Info software, version 6.04D, 2001.
The interventions to which the parturients were exposed during labor were studied. These interventions were recorded in the electronic instrument separately and with the resources of the statistical package used four exposure variables have been created: a) NIONCT – including parturients exposed exclusively to non-invasive obstetric nursing care technologies regardless of type and number - stimulus to ambulation, use of the obstetric bank, sprinkler bath with warm water, relaxing massage, stimulation of pelvic movements, aromatherapy, breathing exercises, use of the fisioball, encouragement for the participation of the companion, lateral decubitus, supported squatting position, option for the four-way position; b) Traditional Care (TC) - including parturients exclusively exposed to procedures that are routinely employed in the medicalized care model regardless of the type and number - intravenous infusion of exogenous oxytocin, amniotomy, episiotomy and reduction of the uterine cervix; c) NIONCT + TC – including the parturients exposed to non-invasive technologies of nursing care and procedures routinely employed in the medicalized model regardless of the type and number; d) No record of NIONCT and/or TC - included the parturients who are not exposed to any intervention.
The outcomes assessed were the Apgar Indexes in the first and fifth minutes of life attributed by the pediatricians who provided care for the neonates after birth. The Apgar Index is obtained by observing five objective clinical signs: heart rate, muscle tone, reflex irritability, skin color and breathing, which can receive 0.1 or 2 points each. The total score ranges from 0 to 10 points. The assigned indexes were recorded in the electronic bank and later two variables have been created by grouping them into two categories - less than 8 and greater than or equal to 8 - for each of the two assessment moments. A value greater than or equal to 8 was considered a cutoff point because it characterized the lowest risk for the newborn.
The confounding variables included in the analysis were those recorded in the Birth Records Book: risk classification, number of pregnancies, parity, characteristic of amniotic fluid and birth weight. The criterion adopted for the classification of parturients as usual risk or high risk was the absence of preexisting or gestational pathological conditions and their presence, respectively.
The statistical treatment involved the use of descriptive statistics, bivariate analysis and logistic regression. The regression models were used to assess the chance of NIONCT exposure during labor and delivery contributing to an AI>8 in the first and fifth minutes of life, when compared to the other types of care provided.
Through the bivariate analysis we verified the existence of a relationship between the confounding variables and the intervention variables as well as the outcomes studied. The Chi-square test was used considering significant values of p below 0.05.
For each outcome, two logistic regression models were constructed. In the first model all the confounding variables that were statistically significant were included in the result of the bivariate analyzes. In the final model, only the statistically significant variables observed in the results of the first model were included. In both models, the cross-product ratios expressed in Odds Ratio (OR) with 95% confidence intervals (CI95%) and p value<0.05.
The study was approved by the Research Ethics Committee of the Municipal Health Department - RJ under the protocol No. 189/09 - CAAE: 0221.0.314.000-09, with no need of the free and informed consent term.
RESULTS
In the period studied, the obstetric nurses of this maternity ward monitored 6,790 deliveries. It is important to highlight that, in relation to the age group, 26.96% were adolescents aged from 10 to 19 years old 12. When the number of pregnancies was assessed, it was found that 37.92% were pregnant for the first time; and 41.64% were primiparous - gave birth for the first time. Of the total number of records related to the prenatal care (67.48%), there were 6 or more appointments.
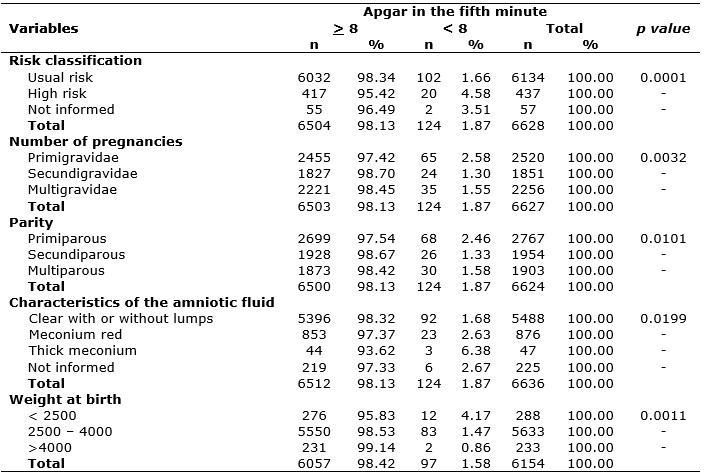
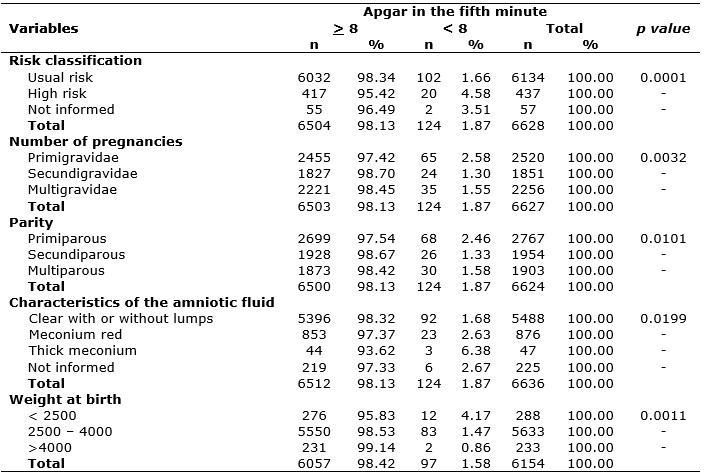
The data in Table 1 show that when assessing the AI at the fifth minute associated with the same variables analyzed in the first minute of extrauterine life, almost all of the newborns, even those who were born bathed in thick meconium (93.62%), adapted to the environment satisfactorily until the fifth minute of life. The same occurred with the newborns whose mothers presented obstetric risk, and the macrosomic NB who presented percentages of 95.42% and 99.14%, respectively.
TABLE 1:
Distribution of frequencies related to the confounding variables according
to the Apgar index in the fifth minute of life. Rio de Janeiro, RJ, Brazil,
2017.
The results obtained in the first logistic regression model related to AI of the first minute of life allowed the adjustment of the modeling. The result of the second adjusted final model allows us to state that the chance of the IA to be >8 in the first minute of life is increased when only the NIONCT is used during labor and/or delivery than when using only TC (OR 2.333; IC95% 1.492 – 3.650; p value 0.0002) or neither NIONCT nor TC is applied, as shown in Table 2.
TABLE 2:
Logistic regression results having as response variable the Apgar index in
the first minute (final model). Rio de Janeiro, RJ, Brazil, 2017.
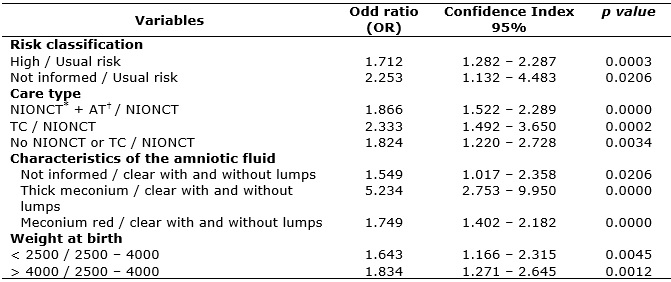
*
Non-invasive obstetric nursing care technologies
†
Traditional care
Regarding the results of the second regression model or adjusted final model, according to Table 3, it was verified that the chance of the AI in the fifth minute being >8 is increased for newborns whose mothers used only NIONCT as a care resource (OR = 4.927; IC95% 2,349 – 10.334; p value 0.00020) when compared to the NB whose mothers belonged to the group of parturients who received TC, with those whose mothers were included in the group in which the type of care employed was unknown (OR = 2.671; CI95%: 1.214 – 5.876; p value 0.0000) and with those whose mothers received both types of care (OR = 2.097; CI95%: 1.314 – 3.348; p value 0.0019).
TABLE 3:
Controlled logistic regression of the variables that obtained significance
in the simple analysis (p<0.01) in relation to the Apgar in the fifth
minute (final model). Rio de Janeiro, RJ, Brazil, 2017.
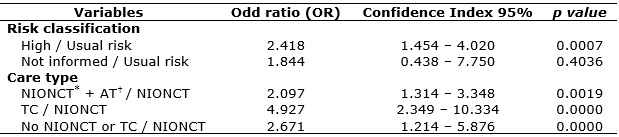
*
Non-invasive obstetric nursing care technologies
†
Traditional care
DISCUSSION
As observed in the results, when characterizing the parturients that had their deliveries accompanied by obstetrical nurses some data deserve to be highlighted. The first is the percentage of adolescents (26.96%), higher than the 24.2% found in another study13. These data alone show the obstetrical nurses' concern about the follow-up of adolescents and show that teenage pregnancy continues to be a global public health problem, especially in developing countries14.
Regarding the obstetric nurses attending the primigravida and primiparous deliveries, the percentages were 37.92% and 41.64%, respectively. These results are close to those found in other studies that indicated 43.6% (11) and 40%15. These conditions, as a rule, are largely associated with behaviors characteristic of the TC model, including the early hospitalization and increased practices/interventions such as endovenous infusion of synthetic oxytocin, amniotomy and episiotomy. It is important to emphasize that even for this group, generally related to the use of interventions, it was observed by the obstetrical nurses the offer and availability of NIONCT.
The percentage of parturients over 35 years old was 5.14%. Regarding this data, studies show that there is no consensus on the isolated age group or maternal condition of risk in the development of pregnancy with unfavorable results for both the woman and the fetus16,17.
Regarding the follow-up of prenatal consultations, it was found that approximately 2/3 of the 6,458 records indicated that the pregnant woman had attended six or more appointments. In the current context, despite the increase in the coverage of the prenatal care, there is a need for better organization by the services, a condition that has been evaluated systematically by the Ministry of Health, which has fomented proposals and actions, in order to meet one of its main principles that is the humanization of the delivery and birth18. Despite not being object of this study, the institution has sought to follow the MS recommendations related to the prenatal care, and the professionals who work there have the responsibility to make pregnant women aware of the importance of the prenatal care for their health and that of their child and their effective participation during the parturition process.
When the dilated uterine cervix was observed at admission, it was verified that in 30.74% of the pregnant women had been admitted in the latent phase of labor (uterine cervix dilatation <4 cm). This condition has been pointed out by some authors as one of those that increases the possibilities of adopting TC-related behaviors. Although this percentage is still high in the present study, it is lower than that presented in a study of 2014, in which, comparing maternity hospitals working under the collaborative model and the traditional model of delivery care, it registered 47.4% and 52.6% %, respectively, of hospitalization of latent women19.
In this study it was evidenced that of the 6,635 IA registered in the first minute of life, 89.63% presented AI>8. This percentage is above the data provided by the Information System on Live Births (SINASC - Sistema de Informações sobre Nascidos Vivos)20 referring to the AI of the newborns from women who had their term gestation deliveries (37-42 weeks gestation), in the hospital environment, vaginally and with the exclusion of the ignored AIs. Therefore, these characteristics are very similar to those of women who had their deliveries accompanied by obstetric nurses in this study. The results of this study were closer to those emanated by SINASC for the year of 2012, which were 87.3% and 87.7% respectively for Brazil and Rio de Janeiro.
When this same process was applied to the AI of the fifth minute of life, it was found 98.13% of AI>8. This result is quite close when compared to 97.9% for the national scope and 97.8% for Rio de Janeiro provided by SINASC20. This first analysis shows that the deliveries attended by obstetrical nurses presented more favorable neonatal outcomes, determining that the use of NIONCT was not a risk factor for the impairment of the vitality of the NB.
When comparing the AI results with the type of care received by the woman during labor and/or delivery, that is, women who only used NIONCT, made use of NIONCT and TC, were only submitted to TC and the group without NIONCT or TC, it was observed that they were discretely inferior to the 99.3% of AI in the 5th day of extrauterine life in CPN as indicated by a study of 201413.
This analysis was important because of the results obtained, which demonstrated, once again, the importance of the obstetric nurse's role in the conception of humanized childbirth care and use NIONCT, aiming at the de-medicalization of the parturition process, especially of women with usual obstetric risk.
When comparing the collaborative and traditional methods of care for labor and delivery of primiparous women in public institutions in Belo Horizonte, regarding the assessment of neonatal vitality through the assessment of the AI with cut of >7, it was observed that newborns from the collaborative method presented better AI in the first minute of life (91.6%) than the group of NB whose mothers had their parturition process conducted by the traditional method (88.5%)19.
A study on low AI in the fifth minute of life in usual-risk parturients and neonatal evolution found that the episiotomy was performed in 71.5% of the cases and was not associated with AI <7 in the fifth minute of life of the newborn. They also report that similar results have been observed by many researchers, others have suggested that failure to perform the episiotomy may cause a prolonged phase of the second period of labor, leading to reduced AI and umbilical artery acidosis at birth21. Although this study did not directly assess the low AI in relation to the variables of episiotomy and time of the second period of labor, but in relation to a set of care guided by the use of NIONCT, of which these variables are also part, it can be inferred, based on the AI in the first and fifth minutes, that the non-performance of episiotomy determines a reduced IA and umbilical artery acidosis in the children of parturients who used only NIONCT.
It was also observed that although the percentage of neonates with AI <8 of parturients who only used NIONCT were significantly lower than that observed when the parturient only used TC (6.59% versus 17.22%),the children of mothers who only used NIONCT responded faster to the care provided by pediatricians than the group of infants of the TC. This can be verified by observing the AI <8 presented in the 5th minute of extra uterine life of the discriminated groups (0.99 versus 5.26%). It is demonstrated once again that when the NIONCT were used, the perinatal findings were better. This evidence was also pointed out by other studies assessing the care models, comparing deliveries attended by obstetrical and nurses and doctors, respectively18,22.
In a systematic review study22, when reporting on the type of care, it was emphasized that there is moderate to high evidence that obstetric nurses use fewer interventions in the parturition process than do medical professionals, achieving similar or better outcomes. In the same study, it was also found that the NB presented percentages of AI considered to be good, and in one of the studies the results related to the assessment of the neonate's vitality were more favorable in the deliveries attended by the obstetric nurses.
In the present study, the best results for newborns in terms of AI >8 (good vitality) were when the obstetric nurse took care of the parturients, who could use only the NIONCT, demonstrating once again the importance of this care model being adopted for pregnant women at usual risk.
CONCLUSION
When assessing the AI (outcome) regarding the variables of interest in order to compare the association between first and fifth minutes of life among mothers who used NIONCT or who underwent TC, it is concluded that the best perinatal results were observed in the group of patients who used only NIONCT during the parturition process. This finding confirms the hypothesis that the use of NIONCT in the obstetric nurse parturition care was not a risk factor for the vitality of the newborn (higher AI> 8 in the first and fifth minutes of life).
The study presented limitations, the most important of which are related to the fact that it is a retrospective study, whose instrument of data collection was elaborated from existing records of information. However, the fact that the registry of the AI of the NB was done by the pediatricians who attended them constituted an important indicator of the reliability of these results. The main limitation of the study regarding the assessment of the vitality of the neonate of deliveries monitored by obstetrical nurses was that there was no record of the procedures performed and, thus, discriminating the fate of the newborns who received AI <8.
Considering the lack of studies that correlate the use of NIONCT and its effects on the vitality of newborns, this study represents an important contribution to the knowledge of obstetric nursing, subsidizing the training of obstetrical nurses from the perspective of de-medicalization. It is understood as necessary that there be continuity and deepening of the results found here through prospective studies, which make it possible to overcome the limitations verified in this research.
REFERENCES
1. Souza JP, Pillegi-Castro C. On labor and childbirth: the importance of quaternary prevention. Cad. Saúde Pública [Internet]. 2014 [Access 2016 Nov 08]; 30(Suppl 1):S11-S13. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2014001300003&lng=pt . doi: http://dx.doi.org/10.1590/0102-311XPE02S114
2. McCourt C. Technologies of birth and models of midwifery care. Rev. esc. enferm. USP [Internet]. 2014 Aug [cited 2017 June 26] ; 48( spe ): 168-177. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0080-62342014000700168&lng=en . http://dx.doi.org/10.1590/S0080-623420140000600024
3. Vargens OMC, Silva ACV, Progianti JM. The contribution of nurse midwives to consolidating humanized childbirth in maternity hospitals in Rio de Janeiro-Brazil. Esc. Anna Nery, Rio de Janeiro , v. 21, n. 1, e20170015, 2017 . Available from http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414-81452017000100215&lng=en&nrm=iso . Access on 26 June 2017. Epub Feb 16, 2017. http://dx.doi.org/10.5935/1414-8145.20170015
4. Leal MC, Pereira APE, Domingues RMSM, Theme Filha MM, Dias MAB, Nakamura-Pereira M, Bastos MH, et al. Obstetric interventions during labor and childbirth in Brazilian low-risk women. Cad. Saúde Pública [Internet]. 2014 [Access 2016 Nov 08];30(Suppl 1):S17-S32. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2014001300005&lng=pt doi http://dx.doi.org/10.1590/0102-311X00151513
5. World Health Organization. Maternal and Newborn health / Safe Motherbood Unit. Care in normal birth: a practical guide. WHO; 1996. [Access 2016 out 03] Available from: http://apps.who.int/iris/bitstream/10665/63167/1/WHO_FRH_MSM_96.24.pdf
6. Ministério da Saúde (BR). Secretaria de Políticas de Saúde. Área Técnica de Saúde da Mulher. Parto, aborto e puerpério: assistência humanizada à mulher. Brasília (DF): Ministério da Saúde, 2001. 199p.
7. McRae D N, Muhajarine N, Stoll K, Mayhew M, Vedam S, Mpofu D, Janssen PA. Is model of care associated with infant birth outcomes among vulnerable women? A scoping review of midwifery-led versus physician-led care. SSM -Population Healt [Internet, access on June 26 2017] 2016; 2(2016):182–93. Available from : http://www.sciencedirect.com/science/article/pii/S2352827316000215?via%3Dihub Doi: https://doi.org/10.1016/j.ssmph.2016.01.007
8. Davis-Floyd R. The technocratic, humanistic and holistic paradigms of childbirth. Int. J. Gynecol. Obstetr. [Internet] 2001 [Access 2016 Nov 08]; 75(Suppl 1):S5-23. Available from: http://www.ijgo.org/article/S0020-7292(01)00510-0/fulltext doi: http://dx.doi.org/10.1016/S0020-7292(01)00510-0
9. Vargens OMC, Silva ACV, Progianti JM. Non-invasive nursing technologies for pain relief during childbirth: the Brazilian nurse midwives' view. Midwifery, 2013;29(11):e99-106. Available from: http://www.sciencedirect.com/science/article/pii/S0266613812002185 doi http://dx.doi.org/10.1016/j.midw.2012.11.011
10. Silva CM, Vargens OMC. Strategies for de-medicalizing in gynecological nursing appointment. Rev enferm UERJ [Internet]. 2013 [Access 2016 Nov 08];21(1):127-30. Available from: http://www.epublicacoes.uerj.br/index.php/enfermagemuerj/article/view/6446/4587
11. Silva AL, Amaral AR, Oliveira DS, Martins L, Silva MR, Silva JC. Neonatal outcomes according to different therapies for gestational diabetes mellitus. J Pediatr (Rio J). [Internet]. 2017 [Acess 2017 Jun 29]; 93(1):87-93. Available from: http://dx.doi.org/10.1016/j.jped.2016.04.004
12. World Health Organization (WHO). Health topics - Adolescent health. [Internet Document] 2017 [Access 2017 Jun 26] Available from: http://www.who.int/topics/adolescent_health/en/
13. Santos NCP, Vogt SE, Pimenta AM, Duarte ED, Madeira LM, Madeira LM, at al. Maternal and neonatal outcomes in labor and delivery of adolescents admitted to a Brazilian Normal Birth Center. Adolesc. Saúde, [Internet]. [Access 2016 Nov 08] 2014;11(3):35-50. Available from: http://www.adolescenciaesaude.com/detalhe_artigo.asp?id=459
14. Martínez HT, Silva MA, Cabrera IP, Mendoza AJ. Obstetric profile of pregnant adolescents in a public hospital: risk at beginning of labor, at delivery, postpartum, and in puerperium. Rev. Latino-Am. Enfermagem. [Internet]. 2015 Oct [Access 2016 Nov 08];23(5):829-36. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692015000500829&lng=en doi http://dx.doi.org/10.1590/0104-1169.0316.262
15. Dahlen HG, Dowling H, Tracy S, Schmied V, Tracy S. Maternal and perinatal outcomes amongst low risk women giving birth in water compared to six birth positions on land. A descriptive cross sectional study in a birth centre over 12 years. Midwifery, 2013;29(7):759-64. Available from: http://www.sciencedirect.com/science/article/pii/S0266613812001258 doi: http://dx.doi.org/10.1016/j.midw.2012.07.002
16. Caetano LC, Netto L, Manduca JNL. Pregnancy after 35: a systematic review of the literature. REME - Rev Min Enferm. [Internet]. 2011 Dez [Access 2016 Nov 08]; 15(4):579-87. Available from: http://www.revenf.bvs.br/scielo.php?script=sci_arttext&pid=S1415-27622011000400015&lng=pt
17. Saito PY, Teixeira NZF, Nakagawa JTT. Analysis of hospital care of maternal deaths: critical reflection. Rev enferm UERJ [Internet]. 2016 [Access 2017 Nov 08]; 24(1):e12530. Available from: http://www.e-publicacoes.uerj.br/index.php/enfermagemuerj/article/view/12530/17860
18. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Atenção ao pré-natal de risco habitual [recurso eletrônico] / Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. – 1. ed. rev. – Brasília: Editora do Ministério da Saúde, 2013. 318 p.: il. – (Cadernos de Atenção Básica, n° 32). Available from: http://189.28.128.100/dab/docs/portaldab/publicacoes/caderno_32.pdf
19. Vogt SE, Silva KS, Dias MAB. Comparison of childbirth care models in public hospitals, Brazil. Rev. Saúde Pública [Internet]. 2014 Apr [Access 2016 Nov 09]; 48(2):304-13. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-89102014000200304&lng=en doi http://dx.doi.org/10.1590/S0034-8910.2014048004633
20. Ministério da Saúde (BR). Datasus. Departamento de Informática do SUS. Informações de Saúde (TABNET) Proporção de partos hospitalares[Internet]. Brasília (DF), 2012. [Access 2016 Ago 27]. Available from: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sinasc/cnv/nvuf.def
21. Salustiano, EMA, Campos JA, Ibidi SM, Ruano R, Ibidi SM. Low Apgar scores at 5 minutes in a low risk population: maternal and obstetrical factors and postnatal outcome. Rev. Assoc. Med. Bras. [Internet]. 2012 Oct [Access 2016 Nov 09]; 58(5):587-93. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-42302012000500017&lng=en doi: http://dx.doi.org/10.1590/S0104-42302012000500017
22. Johantgen M, Fountain L, Zangaro G, Newhouse R, Stanik-Hutt J, White K. Comparison of labor and delivery care provided by certified nurse-midwives and physicans: a systematic review, 1990 to 2008. Women Health Iss, [Internet]. jan/feb, 2012 [Access 2016 Nov 09]; 22(1):73-81. Available from: http://www.whijournal.com/article/S1049-3867(11)00160-5/fulltext doi: http://dx.doi.org/10.1016/j.whi.2011.06.005