ORIGINAL RESEARCH
Kidney disease screening in patients with Diabetes Mellitus in primary health care
Edli Araújo Pinheiro CarvalhoI; Clarissa Cordeiro Alves ArreliasII; Maria Lucia ZanettiIII; Carla Regina de Sousa TeixeiraIV; Francineide Pereira da Silva PenaV; Liudmila Miyar OteroVI
I
Nurse. Master. Federal University of Amapá. Brazil. E-mail: edipinheiro@yahoo.com.br
II
Nurse. PhD. Clinical Hospital of the Medical School of Ribeirão Preto. São
Paulo Brazil. E-mail: claarrelias@usp.br
III
Nurse. PhD. Associate Professor III, School of Nursing of Ribeirão Preto,
University of São Paulo. Brazil. E-mail: zanetti@eerp.usp.br
IV
Nurse. PhD. Associate Professor I, School of Nursing of Ribeirão Preto,
University of São Paulo. Brazil. E-mail: carlarst@eerp.usp.br
V
Nurse. Adjunct Professor, Federal University of Amapá. Brazil. E-mail: francip@bol.com.br
VI
Nurse. PhD. Associate Professor, Federal University of Sergipe. Brazil.
E-mail: liudmilamiyar@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2018.21495
ABSTRACT
Objective: to determine the occurrence of elevated albumin in patients with type 2 Diabetes Mellitus. Method: this quantitative, cross-sectional study considered a convenience sample of 46 patients treated at a primary care health service in Macapá, Amapá, in 2012. Data were collected from March to July 2012, using a form to record demographic (sex and age) and clinical variables (treatment for DM, HbA1c, 24-hour albuminuria and albumin-creatinine ratio). Data were analyzed using descriptive statistics. The project was approved by the research ethics committee. Results: of the 46 patients with diabetes investigated, 4.3% had elevated albumin in 24-hour urinalysis and a 19.6% albumin-creatinine ratio. Conclusion: these results confirm the importance of annual screening for kidney disease with a view to early diagnosis and treatment in order to slow the progression of the disease.
Descriptors: Diabetes mellitus; albuminúria; renal insufficiency chronic; nursing.
INTRODUCTION
Diabetic Nephropathy (DN) is one of the major complications of Diabetes Mellitus (DM) and affects approximately 35% of the population with the disease. This complication represents an additional risk for cardiovascular diseases and increased mortality rate1-4. The worsening of the disease can increase the cost of treatment, leading to more hospital admissions and outpatient consultations, among others5.
Annual screening for renal disease is recommended for patients with type 1 DM (DM1) from the fifth year of diagnosis onwards and, in the case of patients with type 2 DM (DM2), since the moments of diagnosis. Increased urinary excretion of albumin is an indication of renal impairment 6,7.
Despite these recommendations in the municipality of Macapá, Amapá, the screening of renal disease in DM patients still has to be included in the protocol of care for diabetes patients. When urine tests for DN are requested, they are performed in another state. Thus, early diagnosis of DN may be compromised in DM patients. This study aimed to determine the occurrence of increased albuminuria in type 2 DM patients.
LITERATURE REVIEW
In Brazil, in 2003, there were 54,523 patients undergoing dialysis treatment; in 2011, there were 91,314; in 2012, 97,586; and in 2013, 100,397. This indicates an increase of 3% in the three years of study. Of these patients, 30% had DM8 as the underlying disease. Other studies conducted in Brazil with the aim of characterizing patients with renal disease showed that DM is one of the main comorbidities present in patients with renal disease9-12.
A retrospective cohort study conducted in the USA showed that the cost of patients who progressed from the stage of normoalbuminuria to that of microalbuminuria (MA) was 37% higher when compared to those who remained in the normoalbuminuria stage. Likewise, for those who progressed from MA to macroalbuminuria, the cost was 41% higher when compared to patients who continued at the MA stage5.
Early diagnosis of renal disease allows renal damage to be identified in the MA stage, i.e., when albuminuria values range from 30 to 299 mg in a 24-hour urine sample or when the albumin-creatinine index is between 30 and 299 mg/g in an isolated sample of urine. The presence of MA is an important risk factor for cardiovascular problems and progression of chronic kidney disease in diabetes patients6,11,12.
Increased urinary excretion of albumin is detected in approximately 25% of patients1,2. The treatment aims at renal protection and is effective when kidney disease is detected early. Estimation of glomerular filtration rate (GFR) and measurement of urinary albumin excretion are the recommended screening tests. Albuminuria can be performed by measuring the albumin-creatinine index or by the concentration of albumin in an isolated sample of urine, or in a 24-hour urine sample6.
Another important parameter for the prevention of DN is the evaluation of glycemic control, whose gold standard is the measurement of glycated hemoglobin A1c (HbA1c). The reduction in HbA1c values is directly related to the reduction in the number of cases of DN, especially when glycemic control is performed early13.
METHODOLOGY
A quantitative, cross-sectional study was carried out in a Basic Health Unit (BHU) in the city of Macapá, Amapá, in 2012. The population was composed of DM patients enrolled in abovementioned BHU. Patients with DM1, with at least 5 years of diagnosis, and with DM2 with information in medical records were included in the study. Patients with a history of renal disease recorded in the medical records were excluded. The convenience sample consisted of 46 DM2 patients who attended the BHU from March to July 2012.
For data collection, a form containing demographic (sex and age) and clinical variables (treatment for DM and laboratory tests of HbA1c, 24-hour albuminuria, and albumin-creatinine index) was used. HbAlc values lower than 7% and albuminuria less than 30 mg were considered the parameter for normality. The albumin-creatinine index was determined on an isolated sample of urine as a complementary method for the detection of kidney damage. Values lower than 30 mg/g were considered normal6.
Data regarding the address and telephone number of the patients were collected through consultation of medical records. With the information in hand, the researcher contacted the patients and invited them to a group activity in the health unit. Patients who attended the meeting were invited to participate, after clarifying the objectives and the nature of the study. Data were obtained after the signing of the Informed Consent Term.
For 24-hour urine collection, the patients received two bottles, previously identified, with space to record the time of start and end of collection, and a pamphlet with guidelines for urine collection was also provided. Patients were instructed to attend the BHU after the last morning collection to deliver the urine sample and for HbA1c dosage. A DCA 2000+ benchtop spectrophotometer was used for measurement of 24-hour albuminuria, as it was acquired by one of the researchers for this purpose. Urine analysis was performed immediately after sample collection.
The Statistical Package for the Social Sciences (SPSS) 20.0 was used for registration, analysis and processing of data. Data were analyzed using descriptive statistics. The results were presented by measures of frequency (absolute numbers and percentages), central tendency (mean) and dispersion (standard deviation).
The results of the exams were printed and delivered to the patients at a pre-scheduled day, time, and place. Patients who presented alteration in the test results were referred to an endocrinologist at the BHU. The project was approved by the Research Ethics Committee of the Federal University of Amapá under protocol nº 415907/011.
RESULTS AND DISCUSSION
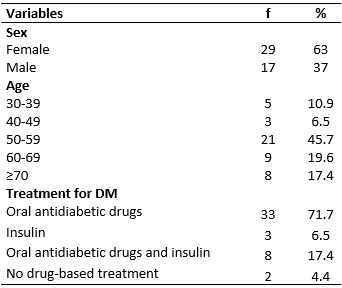
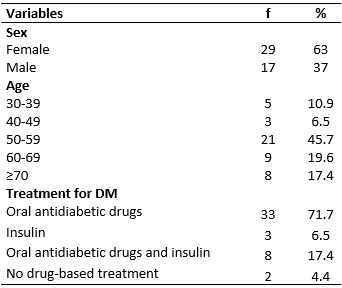
Of the 46 DM patients, 29 (63.0%) were women, with mean and standard deviation of 58 ± 12.6 years. Regarding the treatment for DM, the majority of patients used oral antidiabetic drugs as monotherapy 33 (71.7%). Insulin use alone was verified in 3 (6.5%) patients, while the use of the combined therapy of oral antidiabetic drugs and insulin was present in 8 (17.4%) patients. Furthermore, 2 (4.4%) patients had no prescription records for the treatment of the disease, as shown in Table 1.
TABLE 1:
Distribution of DM2 patients from a BHU according to sex, age and treatment
for DM. Macapá, AP, 2012. (N = 46)
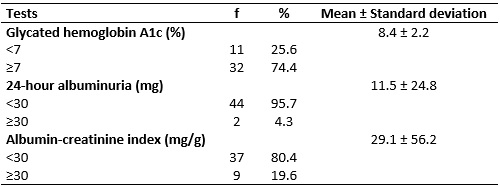
Regarding HbA1c values, of the 43 patients who had blood collected for examination, 32 (74.4%) presented values above the recommended level. As for albumin values, 2 (4.3%) presented increased values in the 24-hour albuminuria test, and 9 (19.6%) in the albumin-creatinine index, as shown in Table 2.
TABLE 2:
Distribution of DM2 patients from a BHU according to glycated hemoglobin,
24-hour albuminuria, and albumin-creatinine index. Macapá, AP, 2012. (N =
46)
The screening for increased albuminuria is of great clinical importance because of its association with increased mortality, cardiovascular risk, and progression of renal disease in both DM1 and DM23,4,7,11.
The results showed that 2 (4.3%) patients had increased albumin in the 24-hour urine test and 9 (19.6%) in the albumin-creatinine index. A cross-sectional study of 927 DM2 patients in ambulatory care showed that of the 117 patients who had advanced nephropathy, 81 were identified in the dialysis treatment units and 36 had chronic renal failure14.
The results found may indicate the presence of renal damage in a larger number of patients than that detected by the 24-hour urine test. On the other hand, this result should be viewed with caution because of the daily variability of albuminuria values and other factors that may interfere with albuminuria values such as hyperglycemia and arterial hypertension. Thus, in the case of patients with altered albuminuria values, the results must be confirmed by two of three samples, within an interval of three to six months6,15-17.
HbA1c values equal to or higher than 7% are related to an increased risk of complications such as DN18,19. The results of this study show that the majority of patients presented HbA1c values higher than the recommended, confirming the importance of annual screening of albuminuria to allow the adoption of appropriate therapeutic measures in order to delay the progression of kidney disease in these individuals.
The alterations found in the results of the MA and albumin-creatinine index obtained do not allow the diagnosis of DN. However, the findings are clinically relevant because MA is the first clinical sign of renal dysfunction in DM patients, and approximately 2% to 5% of such patients present impaired renal function20.
It is noteworthy that the patients in the study reported that they had never undergone MA examination, since this test is not part of the clinical protocol of the health unit. The results obtained confirm the relevance of annual screening for MA, and of appropriate therapeutic measures to prevent or delay the evolution of DN in these individuals.
CONCLUSION
This study allows concluding that 4.3% of the patients presented increased albumin in the 24-hour urine test and 19.6% in the albumin-creatinine index. The results confirm the importance of annual screening for renal disease aiming at early diagnosis and treatment, in order to delay the progression of the disease.
The study presents limitations related to the cross-sectional design, which prevents establishing the cause and effect relationship between the variables investigated. On the other hand, the study allowed the detection of important alterations in the studied variables and the creation of new hypotheses for future research.
REFERENCES
1.Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J. Temporal trends in the prevalenceof diabetic kidney disease inthe United States. JAMA. 2011; 305(24):2532-9.
2.Dwyer JP, Parving HH, Hunsicker LG, Ravid M, Remuzzi G, Lewis JB. Renal dysfunction in the presence of normoalbuminuria in type 2 diabetes: results from the DEMAND study. Cardiorenal Med. 2012; 2(1):1-10.
3.Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guide-line. Ann. Intern. Med. 2013; 158(11):825-30.
4.Viana LV, Gross JL, Camargo JL, Zelmanovitz T, Rocha EPC, Azevedo MJ. Prediction of cardiovascular events, diabetic nephropathy, and mortality by albumin concentration in a spot urine sample in patients with type 2 diabetes. J. Diabetes Complications. 2012; 26(5):407-12.
5.Nichols GS, Vupputuri S, Lau H. Medical care costs associated with progression of diabetic nephropathy. Diabetes Care. 2011; 34(11):2374-8.
6.American Diabetes Association. Standards of medical care in diabetes-2017: summary of revisions. Diabetes Care. 2017; 40 (Suppl 1):S4–S5.
7.Huaira RMNH, Paula RB, Bastos MG, Colugnati FAB, Fernandes NMS. Validated registry of pre-dialysis chronic kidney disease: description of a large cohort. J. Bras. Nefrol. 2018; 40(2): 112-21.
8.Sesso RC, Lopes AA, Thomé FS, Lugon JR, Santos DR. Brazilian Survey of Chronic Dialysis 2013 - analysis of trends between 2011 and 2013. J. Bras. Nefrol. 2014;36(4):476-81.
9.Gomes ET, Papaléo MMM. Characterization of patients with renal insufficiency treated in the emergency of a general hospital. Rev. enferm. UERJ. 2015; 23(4):488-93.
10.Xavier BLS, Santos I, Almeida RF, Clos AC, Santos MT. Individual and clinical characteristics of clients with chronic renal disease in renal replacement therapy. Rev. enferm. UERJ. 2014; 22(3):314-20.
11.Bakris GL, Molitch M. Microalbuminuria as a risk predictor in diabetes: the continuing saga. Diabetes Care. 2014; 37(3):867-75.
12. Sesso RC, Lopes AL, Thomé FS, Lugon JR, Martins CT. Brazilian Chronic Dialysis Census 2014. J. Bras. Nefrol. 2016; 38(1):54-61.
13.Eiriz R, Sousa C. Diabetes Mellitus tipo 2: Impact of intensive glycemic control on diabetic nephropathy. Rev. Port. Med. Geral Fam. 2012; 28(5):378-80.
14.Scheffel RS, Bortolanza D, Weber CS, Costa LA, Canani LH, Santos KG, et al. Prevalence of micro and macroangiopatic chronic complications and their risk factors in the care of out patients with type 2 diabetes mellitus. Rev. Assoc. Med. Bras. 2004; 50(3):263-7.
15.Miller WG, Bruns DE, Hortin GL, Sandberg S, Aakre KM, McQueen MJ, et al. Current issues in measurement and reporting of urinary albumin excretion. Clin. Chem. 2009; 55(1):24-38.
16.Levey AS, Stevens LA, Schmid CH, Zang YL, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150(9):604–12.
17.Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am. J. Kidney Dis. 2012; 60(5):850-86.
18.UK Prospective Diabetes Study (UKPDS) Group: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352(9131):837-53.
19.Nunes MKS, Silva AS, Evangelista IWQ, Filho JM, Gomes CNAP, Nascimento RAF, et al. Hypermethylation in the promoter of the MTHFR gene is associated with diabetic complications and biochemical indicators. Diabetol. Metab. Syndr. 2017; 18 (9):84.
20. Penno G, Solini A, Bonora E, Orsi E, Fondelli C, Zerbini G, et al. Defining the contribution of chronic kidney disease to all-cause mortality in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian Multicenter Study. Acta Diabetol. 2018; 55(6): 603-12.