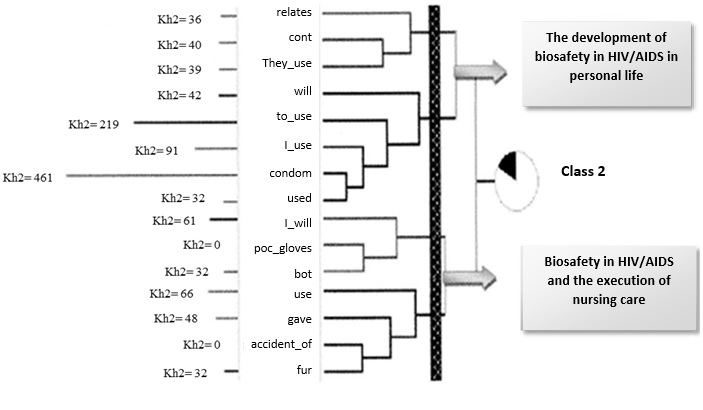
FIGURE 1: Hierarchical Ascending Classification of Class 2. Rio de Janeiro, 2011.
ORIGINAL RESEARCH
Social representations of biosecurity in the context of HIV/AIDS: contributions to workers' health
Ana Paula Munhen de PontesI, Denize Cristina de OliveiraII, Virginia Paiva Figueiredo NogueiraIII, Yndira Yta MachadoIV, Renata Lacerda Marques StefaiskV, Marcio Martins da CostaVI
I
Nurse. PhD. Adjunct Professor, Faculty of Nursing, Center of Higher
Education of Valencia (Centro de Ensino Superior de Valença). Rio de
Janeiro, Brazil. E-mail: ana.munhen@faa.edu.br
II
Nurse. PhD. Full Professor, Nursing College, State University of Rio de
Janeiro. Brazil. E-mail: dcouerj@gmail.com
III
Nurse. PhD, Post-Graduation Program in Nursing, State University of Rio de
Janeiro. Brazil. E-mail:
virginiafigueiredo@yahoo.com.br
IV
Nurse. PhD student, Graduate Program in Nursing, University of the State of
Rio de Janeiro. Brazil. E-mail:
yndiramachado@gmail.com
V
Nurse. MS. Graduate Program in Nursing at the State University of Rio de
Janeiro. Brazil. E-mail: renata_350@hotmail.com
VI
Nurse. PhD. Adjunct Professor, Faculty of Nursing, Center of Higher
Education of Valencia (Centro de Ensino Superior de Valença). Rio de
Janeiro, Brazil. E-mail: marcio.martins@faa.edu.br
DOI: http://dx.doi.org/10.12957/reuerj.2018.21211
ABSTRACT
Objective: to analyze the social representations of biosecurity for nurses who work with HIV-positive patients. Method: qualitative and exploratory research, based on social representations theory, held in eight health institutions, with 19 nurses, in the city of Rio de Janeiro. Data were obtained through interviews and analyzed with the ALCESTE 4.10 software. The project was submitted and approved by Research Ethics Committee. Results: two themes emerged from the analysis: the development of biosafety in HIV/AIDS in personal life and, biosecurity in HIV/AIDS and performing nursing care. It was identified that self-protection is one of the key elements that constitute the nurses' social representation of biosafety, assuming the facets of self-protection in professional and personal life. The use of gloves is featured as the main caution measure at work. Conclusion: stands out the influence of the social representation of HIV/AIDS in the self-protection actions carried out by these nurses.
Descriptors: Occupational health nursing; containment of biohazards; acquired immunodeficiency syndrome; nursing.
INTRODUCTION
The nursing team is characterized as the professional category that most suffers accidents in health institutions. This worker is exposed to several risks arising from assistential and managerial activities in the work environment. It should be noted that, especially, the nursing auxiliaries category presents a high number of accidents due to their often exhausting and stressful work routine.1-3
The biological risk is highlighted in the hospital environment due to the permanent exposure of nursing workers to biological agents existing in the environment. This risk became more evident after the emergence of Acquired Immunodeficiency Syndrome (AIDS) and the increase in the number of people infected with Hepatitis B and C Virus.4
In health services, most of the accidents involving workers are due to non-observance of safety standards, since the use of safe practices and the use of appropriate personal protective equipment (PPE) significantly reduce the risk of occupational accidents.5 Biosafety comprises a set of actions to prevent, control or eliminate risks inherent in activities that may interfere with or the compromise quality of life, human health and the environment. The health biosecurity actions are essential for the promotion and maintenance of well-being and protection of life and health, ensured by the basic principles of the Unified Health System (SUS) and government policies.6
In Brazil, the first biosafety legislation, Law No. 8794, was created in 1995. In 2005, the Ministry of Labor established the Regulatory Norm 32, which purpose is to establish the basic guidelines for the implementation of measures to protect the health and safety of workers of health services. 7,8 In 2011, some articles of this Norm were modified by means of Administrative Rule no. 1,748 / 11, instituting the mandatory implementation of a Plan for the Prevention of Accident Risks with Perforating materials.9
Thus, this study aims to analyze the social representations of biosafety constructed by the nurses who work with patients seropositive to the Human Immunodeficiency Virus (HIV).
THEORETICAL-METHODOLOGICAL REFERENCE
Exploratory, descriptive, qualitative approach. As theoretical methodological reference was used the Theory of Social Representations in its procedural approach.10,11 Eight public health institutions were selected, four hospitals and four municipal health centers, located in the city of Rio de Janeiro, which provide care for people living with HIV and AIDS (PLHA).
The participants were 19 nurses working in the direct care of PLHA. Each participant received a fictitious nomenclature, characterized as E1, E2 to E19. The data collection took place in the year of 2011, instrumented by a thematic itinerary of interview and a questionnaire of socio-professional characterization. The socio-professional data will not be presented in this study.
The ethical aspects of research were respected, in accordance with Resolution No. 196/1996, in force during the period of data collection. The umbrella project to which this study is associated was submitted to the Research Ethics Committee of the University of Rio de Janeiro (UERJ) and the City of Rio de Janeiro, approved under protocol numbers 048.3.2010 and 38A/2011, respectively.
The interviews were submitted to lexical analysis, developed by the hierarchical technique of the software ALCESTE 4.10. It was built a corpus which includes the interviews transcribed in a single file, separated by the star line containing the variables referring to each one of them. After, the software proceeded to segment and treat the corpus. The purpose of examining the corpus by means of this quantitative technique of treatment of textual data is to provide important information about the nature of the contents of the representation analyzed.12
RESULTS
Hierarchical Descendant Classification (HDC) allows the visualization of the corpus in sets of Elementary Context Units (ECU), characterized by excerpts from the participants. The set of ECUs result in lexical classes, which show the contents of a given representation or of more than one representation of the studied object. Also, as a result of each class, the Hierarchical Ascendant Classification (HAC) is presented, which is constituted by determining the value of association between the reduced forms of a given class.
The analysis of the set of interviews resulted in 6 classes identified in the standard analysis from the HDC, and from these, class 2 was the one that synthesized the contents related to biosafety, being discussed in this work from the HAC.
The class 2 – Precautionary measures adopted by nurses who work in the care of people living with HIV/AIDS: the threshold between professional and personal life – dealing with biosafety content; Thus, it was sought to identify the protection actions developed by nursing workers, in personal and professional life, constituents of the group's representation about biosafety, and that influence professional practice.
This class covers a total of 349 ECU, out of a total of 1414, representing 17% of analyzed corpus. It presents a statistical association with: nurses aged between 35 and 44 years; physical and verbal contact with people with HIV; frequency of daily contact with PLHA; time of action with PLHA from 11 to 15 years.
The reduced forms associated to this class, and that presented higher qui-square values (x2), were: condom+; use+; proc_gloves+; conf+; relates+; mask; accident_of+; fur+. It is noted that the reduced forms point to contents related to precautionary measures in personal and professional life, as well as occupational exposure.
The delimitation of the contents of class 2 can be identified in detail from the HAC, coming from the successive binary divisions made by the software in the discursive material. The grouping of words that assign meaning to the class is specified in Figure 1.
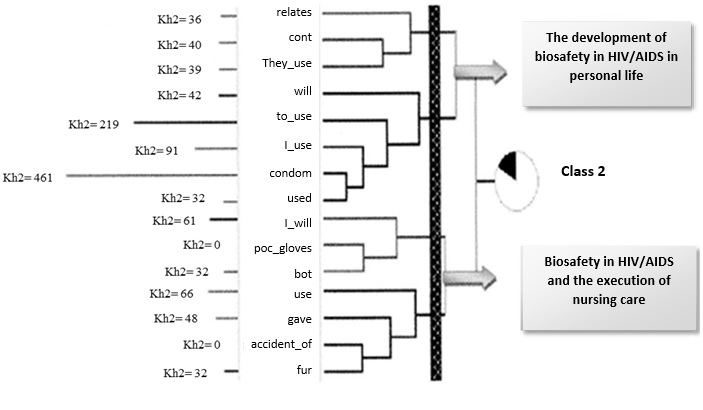
FIGURE 1: Hierarchical Ascending Classification of Class 2. Rio de Janeiro, 2011.
From the grouping of the reduced forms and the analysis of the ECU of the class, it was possible to identify two facets related to the biosafety measures adopted by nurses in their daily activities, which are described below.
The development of biosafety in HIV/AIDS in personal life
The nurses interviewed show that they have theoretical knowledge related to biosafety measures and in their discourses associate self-protection in personal life with the importance of condom use, even in the face of a relationship considered stable.
When I started to get a sense of what AIDS really was, I started to think a lot more about protection in condoms. In my youth, we used to say that it was 'to chew a gun wrapped'. And no doubt it changed, even changed in relation to marriage. Because it's not because you're married that you're immune. That was also something I used to believe and I do not believe anymore, I really do not believe it. (E2)
Noting the complex relations between knowledge and practice, some factors were described by nurses as a justification for not adopting condoms, even acknowledging their need. Among them, trust in partner loyalty can be highlighted, determining a sense of invulnerability to AIDS, and the difficulty of negotiating the use of condom.
We end up taking this risk. For me it has not changed because I do not go out, I do not have relationships outside of marriage and I try to trust a lot in my husband. (E6)
I said: people this is very difficult. There are people who if you ask: do you use a condom? I do. Are you going to say they don't, that you do not believe? Because if people say they do, it's because they do. There are people that believe. I trust in my husband. (E9)
In the suspicion of extramarital relationships, the need for protection is emphasized and the difficulty in negotiating the use of condoms is present.
From time to time I think like this: is he [the partner] correct? I know of myself, but we never know what goes on in the other's mind, what he's doing out of my sight. I already tried to propose to be just with condoms, but for me these things are more complicated. (E3)
Biosafety in HIV/AIDS and the execution of nursing care
In general, it is observed that nurses have theoretical knowledge related to prevention, standard precaution, biosafety and the occupational risks to which they are exposed. In the professional sphere, self-protection covers issues related to standard precautions and occupational exposure, since they recognize the importance of adopting precautionary measures to avoid the occurrence of work-related accidents during the execution of care.
Because there it is to be used, I use. I use the procedure glove, I wear the mask, I wear a smock. It's hot, I'm sweating, the sweat is dripping, but I'm there. (E4)
He went there, he protected himself in terms of personal protective equipment. When you do not know what it is, you use everything, you wear smock, mask, a lot of things. You do not know which organic fluid contaminates. (E3)
Nursing care is modulated by the known presence of HIV, as greater caution is reported by professionals related to the occurrence of accidents with biological material in these situations. Feelings such as fear, anguish and prejudice in dealing with patients living with HIV/AIDS are present in the speeches.
If I know that the patient is an HIV positive patient or know that the patient has hepatitis it is clear that my care is increased, even because the patient is a source of contamination, you behave more carefully. (E3)
Nurses recognize the need and importance of using PPE during nursing care, especially the procedure glove, as evidenced in another study.13
We know it is scientifically proven that the procedure glove is a [protective] way, I always use it and I talk to new staff. We have it, there is no lack, have everything. Now, not always people use, I do not use the mask myself, I am being sincere [...]. (E9)
In a specific way, it was possible to identify justifications for not using PPE and for the occurrence of accidents. These include spiritual protection and some activities that require immediate action, such as emergency situations.
An accident at work can happen to anyone, you can use the procedure glove, why not use it? Then she said that: 'it is not a matter of being an accident at work, even if I puncture myself there is no problem, because Virgin Mary is always with me' (E1).
I worked a lot, a lot of time even dealing with direct contact with patient blood. Why do they say: Why don't you wear a procedure glove? Sometimes the thing is so fast, so immediate, or you do or the guy is going to drain in blood there and when realize, you already got it and sometimes you do not see it and you touch it and such ... (E15)
The nurses report great concern about the different types of accidents to which they are exposed, highlighting the biological risk objectified as a work accident with biological or sharp material.
[speaking about the fear of working in the infectious sector] From here I do not know how long, it may be a hypothesis, it's a hypothesis, and people are afraid of it and are afraid of the work accident with biological material too, but we say that in Nursing care anywhere is the same. (E12)
I had colleagues who suffered an accident at work, they stuck a finger when puncturing the vein, but thanks to God, until today this haven't happened to me. And I also have the utmost care, and I have to be careful with myself and careful with others. (E8)
DISCUSSION
On the theme of the first axis, the development of biosafety in HIV/AIDS in the personal life, emerged talks about the theoretical knowledge of the nurses about the measures of self-protection. It was observed that professional practice with HIV-positive patients has implications for private life, since participants' discourses are characterized by the assumption of safer sexual practices in intimate relationships, the use of condom and the need for dialogue within the family.
Reports of non-use of the condom associated with the belief in partner loyalty refer to a representational process where marriage takes the place of measures to protect against HIV/AIDS. In this perspective, some women believe in invulnerability to infection as an extension of the belief in partner loyalty.
The reliability and the relationship time are considered important factors in the decision not to use condoms.14 Thus, trust in the partner is associated with unsafe sex practices, which increases the risk of HIV infection, in the existence of unknown extramarital relationships. 14,15
In 1987 it was published in Guide for Prevention of HIV and Hepatitis B Virus Transmission in Healthcare Professionals , by the Center for Diseases Control and Prevention (CDC). The Standard Precaution (SP) measures are recommended by the CDC that guides its use for all patients, regardless of their pathology, in all procedures involving bodily fluids that have blood.16
Regarding the second axis, biosafety in HIV/AIDS and the execution of nursing care, it is observed that the nursing work process is associated with several risks and vulnerabilities, among them are biological and accident risks. There is recognition of the importance of standard precaution during nursing care. It is worth emphasizing that this precaution should be adopted for all patients, regardless of their disease.
However, several professionals referred to the accomplishment of nursing care adjustments provided to the patient known to be HIV positive, in relation to the others. These particularities are characterized by excessive use of care when occupational exposure to HIV17, contrary to the one recommended by CDC.16
Important changes occurred in the professional practices of nurses due to the processes of explanation that were established in the face of AIDS. Among the changes can be highlighted the objectivation of distancing practices, verefied both in the use of unnecessary professional self-protection techniques and in the distance observed in interpersonal relationships with patients.18
For these nurses, PPE are necessary and have their importance recognized during nursing care. It emphasizes the glove of procedure, to the detriment of others, like the use of mask and of protective glasses, depending on the situation of exhibition. In the study it was observed that the glove was cited as the main PPE, and sometimes the only one, and consequently the most used by professionals in reducing occupational exposure in contact with blood and body fluids.
It is worth emphasizing that the application of biosafety measures is related to the control of the risks to which health professionals are exposed. Among these measures stand out the use of PPE, continued education, correct hand hygiene, and, above all, the choice of appropriate measures according to the exposure situation faced by the professional.
Hand hygiene, according to the World Health Organization (WHO), is a simple and very important practice as a biosafety measure and in the prevention and control of hospital infection. However, there is still enormous difficulty in putting it into practice.19 In this study, no nurse referred to handwashing as a biosecurity measure; this reinforces that professionals' knowledge and practices in relation to biosafety do not always correspond to the care recommended by technical standards.
Biosafety is a recent area of knowledge, which representsa challenge for health professionals. There is a gap between the theoretical field and the daily practice, since in several contexts the biosafety norms are not adhered properly.20
The situations that justify the non-use of PPE in the hospital routine make professionals more vulnerable to working environment conditions, accidents with biological materials and also to contamination by a communicable disease. The referred vulnerability is underestimated by nursing workers, leading to a feeling of invulnerability enhanced by belief in spiritual protection.
Studies indicate that work-related accidents occur for a variety of reasons, such as needle picking, non-use of PPE, lack of professional attention, intense work pace and working conditions. The inadequacy of PPE was also pointed out as one of the main problems predisposing the accident. It is verified that the majority of workers resist the correct use of PPE, increasing the exposure to accidents by biological material. 3,13, 21
Over time, the adoption of biosafety measures in professional activities has been presented as a challenge for nursing. Some knowledge and acceptance of biosafety norms in professional discourse is observed, however, they are not incorporated into daily practice with the same intensity, revealing the complex network and non-horizontality of the relations between knowledge and practices.22
Feelings such as fear and concern permeate the daily lives of health professionals who fear they may have an accident at work, even among those who have never been injured. These aspects reveal the intensity of the psychological and social repercussions of the accident in the work environment. This fact reinforces the need to recognize and include the psychosocial and educational dimensions in the programs for the prevention of accidents and assistance to workers in health institutions.13
Through the applied characterization questionnaire, a fragility of professional qualification was noticed, since most of the nurses included in this study never participated in specific courses focused on the topic HIV/AIDS. The importance of the discussion on biosafety in the professional training of health students and the constant updating of nursing professionals in this and other areas is considered incontestable, since the qualification of the workforce represents one of the main needs for the incorporation of biosafety measures in care practice.23
CONCLUSION
The discussion on biosafety is nowadays more present in the health institutions of the country, but this discussion has not yet been fully incorporated by the workers who work in the direct assistance of the patient. The participants of the study are aware of the biosafety measures, they refer to them, however, they have not yet transformed them into continuous and conscious professional practices.
The social representation of biosafety constitutes a set of knowledges, attitudes, behaviors and images resulting from the daily experience of professionals in the workplace, thus, it is perceived that the very transmissibility of AIDS and other diseases such as Hepatitis B and C, are retranslated into this representation. If, on the one hand, this transmissibility is recognized and named at the cognitive level, on the other hand it is not expressed in the same way at the level of professional practices.
Regarding theoretical thinking, the transmissibility is expressed at risk to the physical integrity of the nurse; about practical thinking, it becomes a vague possibility of compromising this integrity, resulting in alternative protection behaviors.
Thus, one can infer the hypothesis of the existence of a non-autonomous representation of biosafety, anchored in the social representation of AIDS. It is observed that the contradiction between fear of contagion and a feeling of invulnerability to HIV conditions the practices, the attitudes and the behaviors of protection adopted by the professionals studied.
A limitation of this study is the number of participants, which allows us to suggest an enlargement of the sample, as well as the adoption of a single technique of analysis, since in the field of social representations the triangulation of data would allow a broader understanding of the object of study under discussion.
Finally, it is believed that continuing/permanent education programs on worker health and hospital surveillance centers can be great allies in the implantation of the biosafety norms in the health services, from an effective and responsible participation of the professionals, in order to improve the conditions of work, making it safe and far from risks.
REFERENCES
1.Marziale MHP, Rocha FLR, Robazzi MLCC, Cenzi CM, Santos HEC, Trovó MEM. Organizational influence on the occurrence of work accidents involving exposure to biological material. Rev. latinoam. enferm. [Online]. 2013; [cited 2018 Apr 20]; 21(Spec): [08 telas]. Available from: http://www.scielo.br/pdf/rlae/v21nspe/pt_25.pdf
2.Carvalho DC, Rocha JC, Gimenes MCA, Santos EC, Valim MD. Acidentes de trabalho com materiais biológicos na equipe de enfermagem de um hospital do Centro-Oeste brasileiro. Esc. Anna Nery Rev. Enferm. [Online]. 2018; [cited 2018 Jan 16]; 22(1): 1-8. Available from: http://www.scielo.br/pdf/ean/v22n1/pt_1414-8145-ean-2177-9465-EAN-2017-0140.pdf
3.Oliveira AC, Paiva MHRS. Análise dos acidentes ocupacionais com material biológico entre profissionais em serviços de atendimento pré-hospitalar. Rev. latino-am. Enferm. [Online]. 2013 [cited 2018 Apr 18]; 21:309-15. Available from: http://www.scielo.br/pdf/rlae/v21n1/pt_v21n1a04.pdf
4.Magagnini MAM, Rocha SA, Ayres JA. O significado do acidente de trabalho com material biológico para os profissionais de enfermagem. Rev. gaúch. enferm. 2011 [cited 2018 Apr 20]; 32(2):302-8. Available from: http://www.scielo.br/pdf/rgenf/v32n2/a13v32n2.pdf
5.Valle ARMC, Feitosa MBF, Araújo VMD, Moura MEB, Santos AMR, Monteiro CFS. Representações sociais da biossegurança por profissionais de enfermagem de um serviço de emergência. Esc. Anna Nery Rev. Enferm. 2008; 12(2): 304-9.
6.Ministério da Saúde (Br). Biossegurança em saúde: prioridades e estratégias de ação. [online]. Brasília (DF); 2010. [cited 2018 Apr 20] Available from: http://bvsms.saude.gov.br/bvs/publicacoes/biosseguranca_saude_prioridades_estrategicas_acao_p1.pdf
7.Ministério do Trabalho e Emprego (Br). Riscos biológicos: guia técnico. Os riscos biológicos no âmbito da Norma Regulamentadora nº 32. Brasília: MTE; 2008.
8.Manuais de Legislação. Segurança e medicina do trabalho. São Paulo: Atlas; 2008.
9.Ministério do Trabalho e Emprego (Br). Portaria GM n.º 1.748 de 31 de agosto de 2011. Altera a Norma Regulamentadora (NR) nº 32. Diário Oficial da União. 31 ago 2011, Art. 1º. [cited 2012 Jul 04]. Available from: http://seesspa.com.br/site/wp-content/uploads/2011/12/PORTARIA-N.%C2%BA-1.748-DE-30-DE-AGOSTO-DE-2011.pdf
10.Jodelet D. Representação social: um domínio em expansão In: Jodelet D, organizadora. As representações sociais. Rio de Janeiro: Ed. UERJ; 2001. p. 17-44.
11.Sá CP. A construção do objeto de pesquisa em representações sociais. Rio de Janeiro: Ed. UERJ; 1998.
12.Oliveira DC, Gomes AMT, Marques SC. Análise estatística de dados textuais na pesquisa das representações sociais: alguns princípios e uma aplicação no campo da saúde. In: Menin MSS, Shimizu AM., organizadores. Experiência e representação social: questões teóricas e metodológicas. São Paulo: Casa do Psicólogo; 2005. p.157-200.
13.Sousa AFL, Queiroz AAFLN, Oliveira LB, Moura MEL, Batista OMA, Andrade D. Representações sociais da enfermagem sobre biossegurança: saúde ocupacional e o cuidar prevencionista. Rev. bras. enferm. [Online]. 2016 [cited 2018 Feb 18]; 69(5):864-71. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672016000500864&Ing=en .
14.Felix G, Ceolim MF. The profile of women with HIV/AIDS and their adherence to the antiretroviral therapy. Esc. Enferm. USP. 2012 [cited 2018 Apr 20]; 46(4):884-91. Available from: http://www.scielo.br/pdf/reeusp/v46n4/15.pdf
15.Carvalho CM.L, Martins LFA, Galvão MTG. Sentimentos de mulheres portadoras de HIV/AIDS diante da percepção da infecção. Revista Nursing. 2006; 100(8):1010-5.
16.Centers for Disease Control and Prevention (CDC). Guide to infection prevent for out patient settings: minimum expectations for safe care. [Internet]. 2015 [cited 2018 Apr 08]; Available from: https://www.cdc.gov/hai/settings/outpatient/outpatient-care-guidelines.html
17.Formozo GA, Oliveira DC. Autoproteção profissional e cuidado de enfermagem ao paciente sororpositivo ao HIV: duas facetas de uma representação. Acta paul. enferm. 2009; 22(4):392-8
18.Oliveira DC, Erdman AL, Giami A, Vargens OMC, Oliveira SA, Gomes AMT, et al. Representações e memória profissional da AIDS de enfermeiras no Brasil: estudo bicêntrico Rio de Janeiro/Florianópolis. Psicologia teoria e prática. 2007; 9(1): 114-8.
19.Ministério da Saúde (Br). Higienização das mãos em serviços de saúde. Brasília (DF): Anvisa; 2007.
20.Oliveira JS, Macedo MP, Morais RLGL, Tonan MS, Yarid SD. Biossegurança sob a ótica dos graduandos de enfermagem. Rev. enferm. UERJ . 2017; [cited 2018 Feb 22]; 25: [e14074]: 1-5. Available from: https://www.e-publicacoes.uerj.br/index.php/enfermagemuerj/article/view/14074
21.Villarinho MV, Padilha MICS. Risco ao acidente de trabalho no cuidado às pessoas internadas por HIV/AIDS, Florianópolis-SC-Brasil (1986-2006). Rev. enferm. UFSM. 2014;4(4):689-99.
22.Oliveira AC, Paiva MHRS. Prevalência e características dos acidentes com material biológico envolvendo profissionais do atendimento pré-hospitalar móvel. Cienc. cuid. saúde [Online]. 2013; [cited 2018 Apr 20]; 12(2):323-30. Available from: http://ojs.uem.br/ojs/infex.php/CiencCuidSaude/article/viewFile?19371/pdf
23.Marziale MHP, Santos HEC, Trovó MEM. Consequências individuais e ocupacionais da exposição a material biológico entre trabalhadores de enfermagem. Rev. enferm. UERJ. [Online]. 2015 [cited 2018 Apr 12]; 23(4):449-54. Available from: http://www.facenf.uerj.br/v23n4/v23n4a03.pdf