y=yes; n=no; DC= Defining characteristic
ORIGINAL RESEARCH
Non-expert nurses' performance in classifying clinical indicators of decreased cardiac output
Graciele Oroski PaesI; Juliana Faria CamposII; Juliana Silva MarinhoIII; Erika Christiane Marocco DuranIV; Rafael Oliveira Pitta LopesV; Marcos Antônio Gomes BrandãoVI
I
RN. Post-doctoral degree in Nursing, Adjunct Professor at Universidade
Federal do Rio de Janeiro. Brazil. E-mail: gracieleoroski@gmail.com
II
RN, Ph.D. in Nursing, Adjunct Professor at Universidade Federal do Rio de
Janeiro. Brazil. E-mail:
jujufariacampos@yahoo.com.br
III
Intensive care nurse. Rio de Janeiro. Brazil. E-mail: julymarinho23@gmail.com
IV
RN. Ph.D. in Nursing, Adjunct Professor, Universidade Estadual de Campinas.
Brazil. E-mail: ecduran@unicamp.br
V
M.Sc. Nurse at State Institute for Diabetes and Endocrinology Luiz
Capriglione. Rio de Janeiro, Brazil. Email: pitta.rafael@hotmail.com
VI
RN, Ph.D. in Nursing, Adjunct Professor at Universidade Federal do Rio de
Janeiro. Brazil. E-mail:
marcosantoniogbrandao@gmail.com
DOI: https://doi.org/10.12957/reuerj.2018.19972
ABSTRACT
Objective: to assess the performance of cardiology nurses, non-experts in nursing diagnosis, in classifying clinical indicators of decreased cardiac output, based on the findings of a study of experts. Method: this quantitative, cross-sectional study of diagnostic accuracy examined 23 nurses working in intensive care units of a Rio de Janeiro State public specialist cardiology hospital. The performance measures used were: efficiency, overestimation rate, and underestimation rate. Results: the average rating for efficiency in classifying clinical indicators of decreased cardiac output was 65.9%. In intergroup comparison, the underestimation rate was higher (26.5%) among those who used diagnosis in clinical practice, while overestimation was higher (49.9%) among those who did not use it. Conclusion: non-expert nurses working in clinical cardiology nursing were adequately efficient in classifying a set of indicators similarly to experts.
Descriptors: Nursing diagnosis; cardiac output; nurses; low cardiac output.
INTRODUCTION
Different alternatives have been applied to work with the nursing diagnosis since the original proposal by Fry in 19531 until the current incorporation of the idea of clinical judgment on human responses into its concept2,3.
As judgment, it transmits a summary opinion on knowledge joined and expresses the opinion on the existence of a phenomenon. Thus, a nursing diagnosis is an estimation or professional decision judged based on the clinical manipulation of a set of clues or evidences of professional and disciplinary interest of nursing.
The phenomena, concepts and clues (clinical indicators) have been proposed, described and classified in the diagnostic taxonomies of nursing by so-called experts. They are professionals of recognized knowledge and experience in a given phenomenon or area of knowledge.
One criticism against the nursing diagnosis is that it would represent an academic project4. For the author, the ND represents a disciplinary attempt to construct and take physical and conceptual control of the clinical encounter, distinguishing it from that of other disciplines, and assuming the right to describe what is or could be happening. This initiative is mostly maintained by academic nurses, many of them being faculty and researchers.
The importance of the weight of academic or clinical characteristics that would be appropriate for the validation studies of a nursing diagnosis is still under discussion.
One of the most used models to analyze and validate the contents of nursing diagnoses was proposed by Fehring5,6. In the model, a scoring system identifies an expert, adopting attributes with higher scores for academic traits, such as academic training and publication. It is a fact that, at the time the criteria were proposed, the nursing diagnosis researchers also used to have outstanding clinical experience. With the change in the contours of postgraduate training and the accelerated transition between undergraduate and postgraduate studies, there was an increase in academic researchers in nursing diagnosis who may have little clinical experience in actual health service contexts.
This raises a debate on considering clinical experience and theoretical knowledge important in the definition of an expert in nursing diagnosis7.
From this, what is questioned is the difference between the performance of nurses experts in nursing diagnosis and that of non-expert nurses in this diagnosis in the classification of clinical indicators. In this study, we investigate this issue for decreased cardiac output (DCO).
In this study, the objectives were: to verify the performance of nursing assistants in cardiology who were not experts in nursing diagnosis, in classifying clinical indicators of DCO, based on the findings of a study conducted with experts.
LITERATURE REVIEW
DCO is the insufficient amount of blood pumped by the heart to meet bodily metabolic demands. It currently consists of 36 defining characteristics (DC) and six related factors (RF)5. The main DCs are dyspnea, orthopnea, nocturnal paroxysmal dyspnea, fatigue, edema, jugular vein distension and decreased ejection fraction8, being of crucial importance for the nurse's role in coping with cardiac situations, especially those of greater severity.
Historically, since the time of Florence Nightingale, the nursing area has been concerned with providing quality care9 and, in this context, the application of the nursing diagnosis determines the clarity in the care behavior and better communication among the staff10.
A good clinical evaluation allows the identification of patients with low cardiac output, and nurses have this ability to reliably evaluate patients with heart failure, improving their prognosis11. Despite the contribution of standardized diagnostic languages to clinical reasoning7, the diagnostic decision is not a consensual aspect, especially in the case of a construct going through refinement and clinical validation.
Method
Quantitative, cross-sectional performance study (diagnostic accuracy) study, involving 23 nurses working in intensive care units of the State Institute of Cardiology Aloysio de Castro (IECAC), a public state-owned hospital specialized in cardiology, located in Rio de Janeiro-RJ.
The inclusion criterion considered only nurses active in the system who are intensive care unit attendants, totaling 44 hospital employees. Exclusion criteria were: refusal to participate and nurses who did not present an active situation in the Institution, like in the case of vacations or leaves, among others. Thus, 23 nurses could be interviewed who met the criteria.
The institution and sample were compatible with the reality of many health services in Rio de Janeiro: (1) no standardized institutional use of standardized ND languages (56.5%), (2) nurses with less than five years since graduation (69.6%) and with at least more than one job (86.9%).
For data collection, an instrument was constructed with 53 clinical indicators (signs, symptoms and findings) that could be related to DCD. Forty-six of these derived from the study by Lopes, Altino, Silva 12, and seven were inappropriate indicators that authors had inserted as confounders; being 30 defining characteristics of the diagnostic taxonomy NANDA-I - 2009-2011 (version available when the research project was submitted to the Ethics Committee).
Each clinical indicator was scored on a four-point scale that best represented the strength of indication or intensity of fitness of the clinical indicator to the diagnosis of DCO, with the responses: 3 = main; 2 = secondary; 1 = irrelevant and 0 = inappropriate. We sought to work with the semantics of the strength of evidence concept contained in the concepts of principal, secondary, irrelevant and inappropriate.
The following procedures sometimes used in expert validation studies were waived: presentation of conceptual or operational definitions and realization of training for the knowledge or use of nursing diagnoses or on clinical reasoning strategies. This was done for the purpose of capturing participants not considered as experts in diagnosis in everyday situations of action.
As a parameter of comparison for the participants' answers, the content validation of the DC of the nursing diagnosis DCO was adopted, developed in a study by Lopes, Altino, Silva12, where DC that had a weight equal to or greater than 0.80 were considered as main, those with weight between 0.51 to 0.79 as secondary, those with mean equal to or lower than 0.50 as irrelevant and 0 as inappropriate. After defining the main, secondary and irrelevant categories, the DCs were considered validated (main and secondary) and not validated (irrelevant and inappropriate).
The confounding clinical indicators considered inappropriate, that is, which are not parameters to judge DCO, are: dehydration, headache, decreased skin turgor, diarrhea, chills, chest X-ray alterations and bronchospasm.
The indication strength of the 46 clinical indicators that coincided with the DC in the study by Lopes, Altino, Silva12 was compared iwith the categories derived from the weights, in accordance with the experts' opinion.
Each clinical indicator the study participants scored from 0 to 3 was dichotomized into the categories valid (2 and 3) and not valid (0 and 1) for comparison with the valid (primary and secondary) and non-validated (irrelevant) DC of reference12. The comparison generated coincident and divergent situations.
Divergent: situations in which a participant classified an indicator in the category non-valid (0 or 1), being valid in the study by Lopes, were denominated underestimation of the clinical indicator; when the participants classified an indicator as valid (2 or 3), which had not been validated in the study involving experts, this was called an overestimation of the clinical indicator.
The performance measures used to evaluate the nurses' judgment on the clinical indicators were: efficiency, overestimation rate and underestimation rate.
Efficiency is the performance of an evaluator in coincidentally classifying the strength of the clinical indicator according to its validity in the experts' opinion (E = number of coincident identifications / total number of cases analyzed x 100).
The underestimation rate (Tsub) is the percentage of clinical indicators whose strength was classified as inferior to the validity attributed by the experts (Tsub = number of classification situations in which the strength attributed to the clinical indicator was inferior to what it would actually have / total number of cases subject to underestimation x 100).
The overestimation rate (Tsup) is the percentage of clinical indicators whose strength was classified as greater than the validity attributed by the experts (Tsup = number of classification situations in which the strength attributed to the clinical indicator was superior to what it would actually have / total number of cases that could be overestimated x 100).
The differences between efficiency, underestimation and overestimation rates were compared in statistical significance between groups of nurses using the diagnosis and those who did not use the Mann-Whitney test with the use of GraphadInstat version 3.10. For all analyses, a significance level of 5% (p <0.05) was adopted.
The project received approval from the Research Ethics Committee of the institution where the data collection took place, according to opinion 2011/44. All participants signed the Informed Consent Form after agreeing to participate in the study.
RESULTS
Eleven (47.8%) nurses reported using ND in their clinical practice while 12 (52.2%) did not apply it.
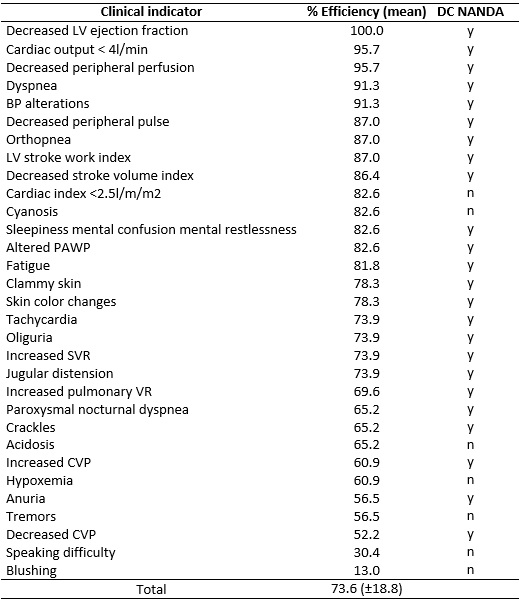
The overall classification efficiency of all 53 clinical indicators of DCO was 65.9%. The validated and non-validated indicators in the reference study13 are presented with their efficiency values in Tables 1 and 2. The mean of the efficiency values was higher (73.6%) in the category of indicators that were considered validated by the experts (main and secondary), as shown in Table 1.
Table 1:
Efficiency rate of clinical indicators validated by experts and relation
with NANDA-I Taxonomy (N=23). Rio de Janeiro, Brazil, 2015.
y=yes; n=no; DC= Defining characteristic
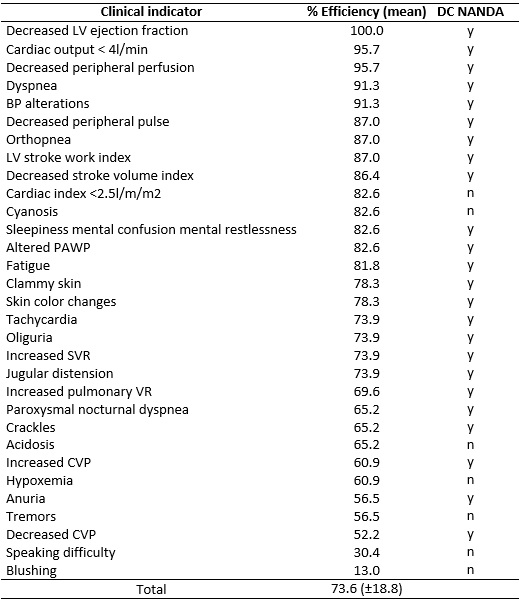
Regarding the group of non-validated (irrelevant) indicators are listed in Table 2, with a general percentage of 55.1%. The difference between the mean efficiency rates of these categories obtained a p-value of 0.018 in the Mann-Whitney test, considered significant.
Table 2:
Efficiency rate of unvalidated clinical indicators and relation with
NANDA-I Taxonomy (N=23). Rio de Janeiro, Brazil, 2015.
DC= Defining characteristic; y=yes; n=no
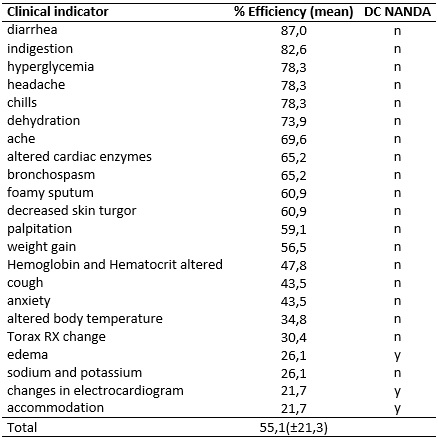
Proceeding with the intergroup analysis, the participants were separated into two groups according to the criterion of using and not using ND. For these groups, the efficiency, Tsub and Tsup of clinical indicators were calculated for each participant, according to Table 3.
TABLE 3: Performance of nurses who use and do not use the nursing diagnosis,
considering efficiency percentage, rates of underestimation and
overestimation of clinical indicators for decreased cardiac output (N=11).
Rio de Janeiro, Brazil, 2015. 
Tsub= rate of underestimation; Tsup= rate of overestimation.
The group of nurses who applied the ND was more efficient (66.5%) than the group that did not use it (65.3%), without statistical significance of the intergroup differences though (p = 0.60).
In the intergroup comparison (using and not using ND in practice), Tsub was higher for those who used it (26.5%) and Tsup for those who did not use (49.9%). The difference of rates was not significant, with p = 0.99 and p = 0.37 for underestimation and overestimation, respectively.
The differences between Tsub (26.5%) and Tsup (43.4%) rates in the ND group were not significant (p = 0.099). Among those who did not use ND, the difference between the median Tsup (49.9%) and Tsub (24.8%) was statistically significant (p = 0.001).
DISCUSSION
One of the challenges of the study is to establish what general efficiency could indicate difference between diagnostic experts and non-experts. The overall efficiency of 65.9% in coincidentally classifying the 53 clinical indicators appears to be convenient. Clinical validation studies of ND present the minimum efficiency expected for only one DC in 70% 7,14. The design of this study entails the complexities and subjectivities of considering dozens of clinical indicators though.
Regarding the performance of evaluators in correctly identifying the ND, there is a proposal to use a minimum efficiency rate of 80%7. There are differences in interpretation though in coincidentally classifying 80% of 53 indicators with experts' opinions in order to be considered efficient.
It should be highlighted that the participants performed best in clinical indicators considered validated, that is, very representative of the ND referring to DCO. Of the 31 items in this category, 14 obtained efficiency rates higher than 80%.
Thus, the high performance only shows that the participants' judgment coincides with that of the experts in the study that served as a basis for comparison. No definitive inference can be made about the diagnostic accuracy (clinical validity) rates of indicators.
The greater efficiency in clinical indicators considered to be evaluated by invasive hemodynamic monitoring and/or dependent on clinical assessment is contrary to new diagnostic trends. Currently, the use of less invasive techniques/technologies is encouraged to minimize the risks associated with health care, and because many cardiac patients are hospitalized in low and medium-complexity services where it is not always possible to apply invasive or minimally invasive monitoring. Thus, the DC depends on evaluation by physical examination, interview or observation gain relevance.
The minimal and statistically non-significant differences between the efficiency rates of nurses who use and do not use ND are somewhat surprising at first glance. In the specific (but not exclusive) case of the DCO, however, one can affirm that the concept derives from basic science and is commonly discussed in undergraduate nursing education, particularly in physiology and biophysics. Both the idea and the indicators of changes in cardiac output are themes that tend to be part of theoretical knowledge in cardiology nursing. In addition, the nurses participating in this study work in intensive cardiology care services, where it is assumed that altered cardiac output is not a rare event.
Thus, one can assume that, even if most of the participants did not use the specific ND language, their nursing actions most likely involved evaluating, monitoring and intervening in individuals with DCO. In a way, the lack of a formalized language would not be an impediment, given the relevance of specific knowledge and experience.
Then, the necessity of the criteria of expertise5 is questioned, given the efforts to comply in situations where there are professionals with experience and theoretical knowledge in the specific diagnosis or in the correlated area7.
Another issue is that of the (unconscious) myth of experts' inerrancy. They are particularly subject to errors linked to the omission of important information, tunnel vision and trend towards familiar hypotheses. Hence, their opinions cannot be taken as infallible.
Analyzing the Tsup and Tsub between the groups (use and do not use), one can affirm the existence of an inclination to overestimate clinical indicators, demonstrating a more liberal classification profile, even if not supported by statistical significance.
One hypothesis for overestimation is the belief that there is less damage from false-positive errors or from overestimating the indicator value. The idea of erring on the side of overestimation would lead one to accept indicators without actual relevance as less harmful than to underestimate relevant data.
Another explanation would be related to the teaching of ND and use of DC which are not accompanied by information that indicates its diagnostic test value (sensitivity, specificity, predictive values, among others). Therefore, individual assumptions based on the belief, knowledge and prior experience of the diagnosing professional or the teacher teaching them to diagnose are responsible for evidence-based estimates of a DC.
Another particularity in some ND of NANDA International Inc. is the high number of DC. This hypothetically may lead nurses to consider that DC indeed have a lot of evidence to support them. Official NANDA-I publication highlights the desire to limit the number of diagnostic indicators though, believing that long lists of signs/symptoms are not that useful clinically 3.
Regarding the difference between Tsup and Tsub for the same group, it can be affirmed that the difference did not happen at random only for those who do not use ND, indicating a clear predominance of the trend to overestimate versus the trend to underestimate. It may be assumed that ignorance of NANDA-I DC further increases this predominance of granting relevance to data that do not support the diagnosis.
The absence of statistical significance between overestimation and underestimation for those using ND only communicates a greater balance in their disagreements with the experts, nullifying a trend towards one of both sides of the disagreement. In terms of performance, however, this does not make them better than the professionals who do not use ND (lack of statistical significance in the intergroup difference in efficiency).
CONCLUSION
It is concluded that the clinical nurses in cardiology nursing not experts in ND efficiently classify a set of indicators, similarly to experts in ND. This is even more prominent among the indicators validated by experts than among those considered invalid.
In the disagreements between study participants and experts in the reference study about the strength of a given indicator serving as evidence for DCO, the trend was towards overestimation, both for those who claimed to use the diagnosis in practice and those who did not. It is only in the group of non-users that a significant trend to overestimate was observed in function of the underestimation.
Based on the results, it is clear that the highest performance of the participants is in the clinical indicators considered validated and dependent on evaluation by invasive hemodynamic monitoring and/or dependent on clinical evaluation.
The research was limited by the nurses' interruption in answering the forms because, during the completion, the nurses were summoned by the team/patients or admissions in the sector. The respondents' pauses may have caused a bias in this study.
The results of this study instigate and foment the discussion about the importance of expertise based on academic criteria in the ND, to the detriment of the value of specialized clinical practice.
REFERENCES
1.Benedet SA, Hermida PMV, Sell BT, Padilha MI, Borenstein MS. Produção científica da reben sobre diagnóstico de enfermagem no recorte histórico de 2003-2010. Hist. enferm. Rev eletronica. 2012; 3(2): 125-40.
2.Conselho Federal de Enfermagem. Regulamentação do exercício profissional. Resolução nº 358/2009. Rio de Janeiro: COFEn; 2009.
3.North American Nursing Diagnosis Association. Diagnóstico de enfermagem da NANDA internacional: definições e classificações (2015-2017). Porto Alegre (RS): Artmed; 2015.
4.Powers P. A discourse analysis of nursing diagnosis. Qualitative health research [Online]. 2002; 12(7): 945-65. Doi: 10.1177/104973202129120377
5.Fehring RJ. Methods to validate nursing diagnoses. Heart Lung.1987; 16(6): 625-9.
6.Oliveira ARS, Costa AGS, Freitas JG, Lima FET, Damasceno MMC, Araujo TL. Validação clínica dos diagnósticos, intervenções e resultados de enfermagem: revisão narrativa da literatura. Rev. enferm. UERJ. 2013; 21(1): 113-20.
7.Lopes MVO, Silva VM, Araujo TL. Methods for establishing the accuracy of clinical indicators in predicting nursing diagnoses. Int. Jnl. Nurs. Knowledge [Online].2012; 23(3): 134–9. Doi: 10.1111/j.2047-3095.2012.01213.x
8.Pereira JMV, Cavalcanti ACD, Lopes MVO, Silva VG, Souza RO, Gonçalves LC. Acurácia na inferência de diagnósticos de enfermagem de pacientes com insuficiência cardíaca. Rev. bras. Enferm[Online]. 2015; 68(4): 690-6. Doi: http://dx.doi.org/10.1590/0034-7167.2015680417i
9.Borsato FG, Vannuchi MTO, Haddad MCFL. Qualidade da assistência de enfermagem: ambiente do paciente em hospital público de média complexidade. Rev. enferm. UERJ [Online]. 2016; 24(2): e6222. Doi: https://doi.org/10.12957/reuerj.2016.6222
10.Bitencourt GR, Felippe NHMD, Santana RF. Diagnóstico de enfermagem eliminação urinária prejudicada em idosos no pós-operatório: um estudo transversal. Rev. enferm. UERJ [Online]. 2016; 24(3): e16629. Doi: https://doi.org/10.12957/reuerj.2016.16629
11.Galvão PCC, Gomes ET, Figueirêdo TR, Bezerra SMMS. Diagnósticos de enfermagem aplicados a pacientes com insuficiência cardíaca descompensada. Cogitare enferm [Online]. Rev. 2016; 21(2): 01-8. Doi: http://dx.doi.org/10.5380/ce.v21i2.44646
12.Lopes JL, Altino D, Silva RCGS. Content validation of current and new defining characteristics of the nursing diagnosis: decreased cardiac output. Acta paul. Enferm [Online]. 2010; 23(6): 764-8 Doi: http://dx.doi.org/10.1590/S0103-21002010000600008
13.Carvalho EC, Cruz DALM, Herdman TH. Contribuição das linguagens padronizadas para a produção do conhecimento, raciocínio clínico e prática clínica da Enfermagem. Rev. bras. Enferm [Online]. 2013; 66(esp): 134-41. Doi: http://dx.doi.org/10.1590/S0034-71672013000700017
14.Matos LN; Guimarães TCF; Brandão MAG; Santoro DC. Prevalence of nursing diagnosis of decreased cardiac output and the predictive value of defining characteristics in patients under evaluation for heart transplant. Rev. latinoam. Enferm[Online]. 2012; 20(2): 307-15. Doi: http://dx.doi.org/10.1590/S0104-11692012000200013
15.Dror IE. The paradox of human expertise: why experts get it wrong. In: Dror IE. Paradoxal brain. Cambridge: Cambridge University Press; 2011.p177-87. Doi: https://doi.org/10.1017/CBO9780511978098.011