ORIGINAL RESEARCH
Nursing diagnoses and interventions in postoperative alveolar bone graft patients
Marli Luiz BeluciI; Suely Prieto de BarrosII; Cassiana Mendes Bertoncello FontesIII; Armando dos Santos TretteneIV; Cleide Carolina da Silva Demoro Mondini V
I
PhD in Sciences by the Postgraduate Program in Rehabilitation Sciences,
University of São Paulo. Bauru, São Paulo, Brazil. E-mail: mlbeluci@hotmail.com
II
PhD in Pediatrics. Head of Clinical Nutrition, Hospital for Rehabilitation
of Anomalies
Craniofacial, University of São Paulo.
Brazil.
E-mail: suelyprieto@yahoo.com.br
III
PhD in Nursing. PhD Assistant Professor, Paulista State University Júlio de Mesquita Filho, Botucatu, São Paulo, Brazil.
E-mail: cmbf@fmb.unesp.br
IV
PhD in Sciences. Head of the Intensive Care Unit, Hospital for
Rehabilitation of Craniofacial Anomalies, University of São Paulo.
E-mail: armandotrettene@hotmail.com
V
PhD in Sciences. Head of the Nursing Service, Hospital for Rehabilitation
of Craniofacial Anomalies, University of São Paulo. Brazil. E-mail:cmondi ni@usp.br
VI
Financial Support: Coordination of Improvement of Higher Education
Personnel
DOI: http://dx.doi.org/10.12957/reuerj.2017.19872
ABSTRACT
Objective: to identify the frequency of nutrition-related nursing diagnoses and postoperative nursing interventions in alveolar bone graft surgery during hospitalization. Method: this descriptive, quantitative study took place at a specialized public hospital in a sample of 150 patients evaluated by anamnesis and observation focusing on food acceptance. Results: the nutrition-related nursing diagnoses were prepared according to the taxonomy of the North American Nursing Diagnosis Association-International (NANDA-I), and displayed a predominant willingness to improve nutrition. The interventions proposed according to the frame of reference of Nursing Interventions Classifications (NIC) related to teaching prescribed diet, promoting self-care, and monitoring nutrition. Conclusion: this study contributed to interdisciplinary work between nutrition and nursing in the care process.
Keywords: Cleft lip; surgery, oral; nursing diagnosis; patient care team.
INTRODUCTION
The rehabilitation of the patient with cleft lip and palate is complex due to the great morphological variation, anatomical and functional impairment, being the cleft lip and palate one of the most common craniofacial malformations.1 In the surgical rehabilitation, in cases where the cleft involves the alveolar ridge, the alveolar bone graft (ABG) is indicated for the filling of the bone discontinuity with autogenous medullary bone, removed from the iliac crest.2
In the Brazilian hospital environment, the prevalence of protein-energy malnutrition ranges from 20% to 50%3, being possibly aggravated by a surgical trauma with increased nutritional needs.4,5 Thus, it is important to be cautious so that, in oral surgeries, the nutritional status is monitored. The patient's eating pattern is completely altered, which may predispose the individual to insufficient nutrient intake, further aggravated by pain and discomfort in the feeding process. 4-7
In the rehabilitation context of the patient with cleft lip and palate, the care process presupposes the interdisciplinary action between nursing and nutrition.8 The Nursing Process is organized in five stages: data collection or nursing history, nursing diagnosis, nursing planning, nursing implementation and assessment.9 The Nursing Classifications, North American Nursing Diagnosis Association-International (NANDA-I)10 and Nursing Interventions Classifications (NIC)11, respectively, are classifications of languages used as theoretical references in health, teaching and research institutions, being essential in the naming and determination of standardized nursing terminologies.10,11
The Nursing Interventions (NI) should be directed towards the resolution of factors related to Nursing Diagnoses (ND). These links have the purpose of relating a diagnosis to one or more interventions, contributing to the clinical decision making of the nurse.12 It is necessary to characterize and adapt the care planning to the population assisted by the nurse.13
The identification of the ND related to nutrition, its defining characteristics10 and the intervention
proposals11 in patients submitted to the ABG surgery may contribute to the identification of care needs related to the patient's feeding, surgical convalescence and rehabilitation. The objective of the present studyVI was to identify the frequency of ND related to nutrition and NI in the postoperative period of ABG.
LITERATURE REVIEW
The postoperative period of ABG surgeries is characterized by the use of a homogeneous liquid diet for 20 days, followed by 20 days of pasty diet, and 20 days of a soft diet in small pieces.5 In the postoperative period, patients receive only the homogenous liquid diet, consisting of juices, smoothies, yogurts and liquefied and fried soups, added daily of 400 ml of food supplements of 1.5 calories per kg of body weight.4,5
In the multidisciplinary team, the nursing team is responsible for monitoring the daily intake and acceptance of food through observation, record in the care records and actions, and assessment according to the planning, represented by the Nursing Care Systematization (NCS). The nutrition team is responsible for THE nutritional status assessment, diet definition and calculation, meal supervision, preparation and distribution.8
For the identification of nutrition-related NDs, with their defining characteristics and the proposed interventions, the NANDA-I and NIC Nursing taxonomies are used.10,11 The interdisciplinary action between nursing and nutrition in the care process, during the postoperative period, can be performed with interdependence and complementarity.14
METHODOLOGY
Descriptive and quantitative study, carried out in a specialized public hospital. The study began after the approval of the project by the Ethics Committee in Research with Human Beings of the Institution, according to Official Letter No. 381/2008-SVAPEPE-CEP, and formalization of the acceptance of participation through the signing of the Free and Informed Consent Term by the patient's caregiver. The inclusion criteria were: patients aged between 10 and 20 years old, who underwent an ABG surgery and were in the postoperative period. The data collection was performed by the researcher, in the presence of the patient's caregiver, through anamnesis and observation, focusing on the description of food acceptance, of 150 patients submitted to an alveolar bone graft surgery, who were in the mediate postoperative period. The collection instrument was developed for this purpose. With the data obtained, the nutritional related NDs were listed, according to the NANDA-I classification10, and the interventions were proposed, according to the NIC classification. 11 The data were tabulated using an Excel spreadsheet, analyzed by descriptive statistics and the results presented in tabular form.
RESULTS AND DISCUSSION
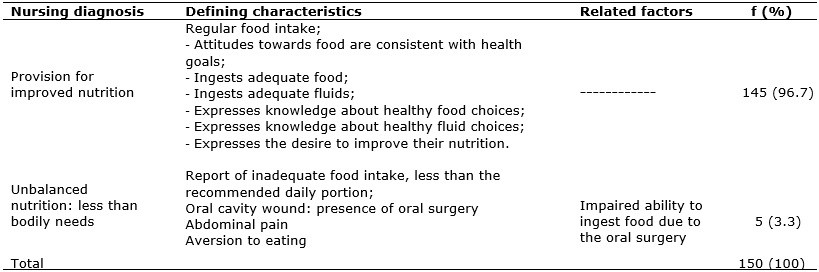
Fifty patients undergoing an ABG surgery with an average age of 13.9 years old were included in the study, of which 95 (63.3%) were male. Two NDs related to nutrition were identified:provision for improved nutrition, with more frequency, and unbalanced nutrition: less than the bodily needs, using the NANDA-I referential10, according to Table 1:
TABLE 1:
Frequency of nursing diagnoses related to nutrition, respective defining
characteristics and related factors, according to NANDA-I.
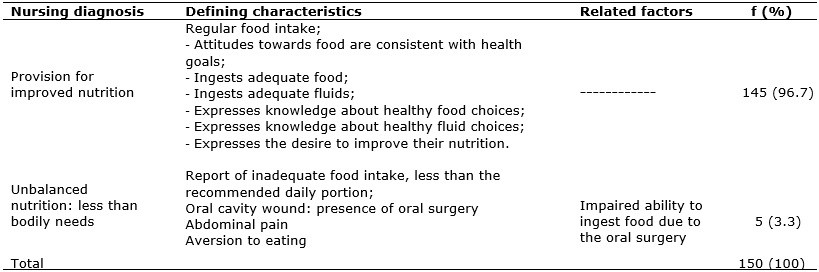
The proposed nursing interventions and activities for nursing diagnoses:provision for improved nutrition and unbalanced nutrition: less than the bodily needs, using the NIC referential11, are presented in Figure 1:
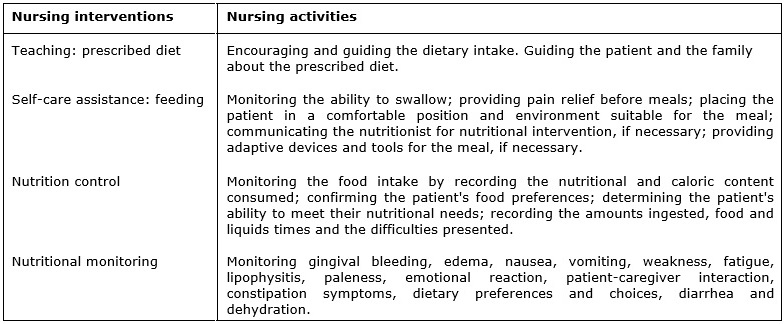
FIGURE 1:
Interventions and nursing activities proposed for the nursing diagnoses
provision for improved nutrition and unbalanced nutrition: less than the
bodily needs according to the NIC.
In the present study, both NDs demonstrate a profile of postoperative nursing care needs, different from the usual, relating to experiences acquired in previous surgeries, considering the long rehabilitation process that begins at the age of three months when, not only the patient, but also the family, acquire training for self-care.
The ND provision for improved nutrition is a ND rated in health promotion10, justified by the need to maintain the adequate intake for the maintenance of convalescence in the postoperative period of oral surgery. Thus, since it is a diagnosis that does not have related factors developed, according to NANDA, and because it is an expected phenomenon, the NI should support and reinforce its maintenance.
Regarding the ND unbalanced nutrition: less than the bodily needs 10, the surgery in the oral cavity was evidenced as the main related factor and, among the defining characteristics, it was verified the difficulty in accepting the diet, injuries in the oral cavity, abdominal pain and food aversion.
The alveolar bone graft contributes effectively to the rehabilitation process of patients with cleft lip and palate, because it allows the filling of the residual bone defect caused by the fissure and the dental eruption in that region, as well as a more favorable orthodontic treatment.15 Associating the benefits of this surgical procedure to the craniofacial growth, it was observed in the present study that, in relation to age, the result corroborated with the recommendation of the literature.2
The systematic observation of care protocols related to the rehabilitation quality of patients with cleft lip and palate has been pointed out as an important instrument for the therapeutic success16; as well as the importance of multidisciplinary and interdisciplinary care in the rehabilitation process and health promotion to the patient with cleft lip and palate.17
The postoperative period is the best moment for the orientations to the patient and the family caregiver, performed by the nursing, regarding the care related to the surgery, aiming at the maintenance of these after discharge, including the bleeding prevention, pain control, feeding, hydration, surgical incision care and physical restraint.18 The concern regarding the feeding is referred to as one of the main nursing care in the postoperative period; therefore, adequate food acceptance may interfere significantly in the postoperative recovery.19
Considering that the quality of the nursing care provided implies directly in the rehabilitation process20, the description of the nursing care needs from the nursing diagnoses, as well as the proposed interventions, can contribute to the planning of the specific nursing care in the postoperative alveolar bone graft.21
During the postoperative period, the liquid diet is recommended to avoid the accumulation of residues in the operated region and bacterial proliferation, and to favor the rest of the location, including the use of dietary supplements. The benefits related to the addition of food supplements in the postoperative period were evidenced in a study in which the reduction of body mass loss and maintenance of adequate nutritional biological indexes was observed, favoring the homeostasis22.
The hospitalization is a break with the daily routine and habits, including eating habits, and it is necessary for the patient to accept and adapt to the standards for the postoperative recovery. However, individualities should be considered and the hospital routines should be made as close as possible to the household routines.23
These factors facilitate the process of adaptation and coping of the patient. Thus, a more flexible and humanistic view of hospital feeding is advocated, considering not only biological but also emotional needs.24
The standardization of a diet manual exists to improve the quality of care, rationalize the service and reduce its costs; however, some flexibilization should be considered.25
In the present study, a great majority (96.7%) of the patients presented good food acceptance, not mentioning pain, nausea or vomiting. This is in line with the work carried out by the nursing and nutrition teams in the search for greater food safety for the patients, involving increased attention to the adherence to the diet.
In cases of low food acceptance, it is recommended the acceptance of food supplements that are a necessary alternative in the face of hyper metabolism conditions, weight loss, low food acceptance, among other clinical situations.4
Considering the impact of adequate food acceptance in the postoperative recovery process and in the promotion of well-being to the patient and their relatives, it is believed that the present study has contributed to the identification of nursing diagnoses, interventions and activities, making it possible to plan and implement interventions that will further improve the patients' adherence.
The interdisciplinary perspective on health is a promising way to improve the quality of care and to contribute to a satisfactory and collaborative work.26,27
CONCLUSION
Most of the patients submitted to the alveolar bone graft surgery, presented the ND for improved nutrition, which reflects a collaborative state in the surgical reestablishment. The interventions proposed were related to the teaching of the prescribed diet, to the promotion of self-care and to nutritional monitoring. The present study contributed to the interdisciplinary work between nutrition and nursing in the care process. Future interdisciplinary investigations may be implemented to other populations of patients with craniofacial malformations.
REFERENCES
1.Freitas JAS, Neves LT, Almeida ALPF, Garib DG, Trindade-Suedam IK, Yaedú RYF, et al. Rehabilitative treatment of cleft lip and palate: experience of the Hospital for Rehabilitation of Craniofacial Anomalies/USP (HRAC/USP) - part 1: overall aspects. J. Appl. Oral Sci. 2012; 20(1):9-15.
2.Freitas JAS, Garib DG, Trindade-Suedam IK, Carvalho RM, Oliveira TM, Lauris RCMC, et al. Rehabilitative treatment of cleft lip and palate: experience of Hospital for Rehabilitation of Craniofacial Anomalies-USP (HRAC-USP) - part 3: oral and maxillofacial surgery. J. Appl. Oral Sci. 2012; 20(6):673-9.
3. Raslan M, Gonzalez MC, Dias MCG, Paes-Barbosa FC, Cecconello I, Waitzberg DL. Aplicabilidade dos métodos de triagem nutricional no paciente hospitalizado. Rev. Nutr. 2008; 21(5):553-61.
4. Peres SPBA, Arena EP, Burini RC, Suguimoto RM. Uso de suplementos alimentares e estado nutricional de pacientes submetidos à cirurgia ortognática com bloqueio maxilo-mandibular. Rev. Bras. Nutr. Clín. 2006; 21(1):28-32.
5. Barros SP, Watanabe SN, Xavier N, Castro CHBC, Borgo HC. Nutritional evolution after alveolar bone grafting followed by oral nutritional supplementation. Rev. Nutrol. 2009; 2(Esp):11- 5.
6. Buckley MJ, Tulloch JFC, White Junior RP, Tucker MR. Complications of orthognathic surgery: a comparison between wire fixation and rigid internal fixation. Int. J. Adult Orthodon. Orthognath. Surg. 1989; 4(2):69-74.
7. Priore SE, Franceschini SCC. Nutrição na adolescência. In: Silva SMCS, Mura JDP. Tratado de alimentação, nutrição e dietoterapia. São Paulo: Roca; 2007. p. 364-79.
8. Beluci ML, Barros SP, Borgo HC, Fontes CMB, Arena EP. Postsurgical alveolar bone graft patients: elaboration and application of a data-gathering instrument for nutrition and nursing. Cleft Palate Craniofac J. 2014; 51(2):172-7.
9. Conselho Federal de Enfermagem. Resolução COFEN-358/2009. Dispõe sobre a Sistematização da Assistência de Enfermagem e a implementação do Processo de Enfermagem em ambientes, públicos ou privados, em que ocorre o cuidado profissional de Enfermagem, e dá outrasprovidências [Internet]. [citado em 10 out 2016]. Disponível em: http://www.cofen.gov.br/resoluo-cofen-3582009_4384.html
10. NANDA International. Diagnósticos de enfermagem da NANDA: definições e classificação 2009-2011. Porto Alegre (RS): Artmed; 2010.
11. Dochterman JM, Bulechek GM. Classificação das intervenções de enfermagem (NIC). 4ª ed. Porto Alegre (RS): Artmed; 2008.
12. Fontes CMB, Cruz DALM. Diagnósticos de enfermagem documentados para pacientes de clínica médica. Rer. Esc.Enferm. USP. 2007; 41(3):395-402.
13. Rocha LA, Maia TF, Silva LF. Diagnósticos de enfermagem em pacientes submetidos à cirurgia cardíaca. Rev. bras. enferm. 2006; 59(3):321-6.
14. Cavalcante AMRZ, Nakatani AYK, Bachion MM, Garcia TR, Nunes DP, Nunes PS. Análise de atividades não realizadas pela equipe de enfermagem para o diagnóstico padrão respiratório ineficaz em idosos. Rev Esc. Enferm. USP. 2012; 46(3):604-11.
15. Roça GB, Freitas RS, Rodrigues LK, Busato LS, Canan L. Enxertia óssea alveolar: uma conduta para todas as fissuras alveolares. Rev. Bras. Cir. Plást. 2010; 25(Supl.):1-102.
16. Alonso N, Tanikawa DY, Lima Junior JE, Ferreira MC. Avaliação comparativa e evolutiva dos protocolos de atendimento dos pacientes fissurados. Rev Bras Cir Plást. 2010; 25(3):434-8.
17. Lorenzzone D, Carcereri DL. Locks A. The importance of multi-professional, interdisciplinary care in rehabilitation and health promotion directed at patients with cleft lip/palate. Rev Odonto Ciênc. 2010; 25(2):198-203.
18. Trettene AS, Razera AP, Maximiano TO, Luiz AG, Dalben GS, Gomide MR. Doubts of caregivers of children with cleft lip and palate on postoperative care after cheiloplasty and palatoplasty. Rev esc enferm USP. 2014; 48(6):993-8.
19. Trettene AS, Mondini CCDS, Marques IL. Feeding children in the immediate perioperative period after palatoplasty: a comparison between techniques using a cup and a spoon. Rev esc enferm USP. 2013; 47(6):1298-304.
20. Pongpagatip S, Pradubwong S, Jenwitheesuk K, Chowchuen B. Knowledge and satisfaction of caregivers of patients with cleft lip-palate at the Tawanchai Cleft Center. Plast. Surg. Nurs. 2012; 32(4):165-70.
21. Beluci ML, Barros SP, Fontes CMB, Genaro KF. Alveolar bone graft: diagnoses, interventions and results according to nursing classifications. J. Nurs. UFPE on line. 2014; 8(7):1876-81.
22. Figueiredo LMG, Carvalho MC, Sarmento VA, Brandão GRR, Oliveira TFL, Carneiro Junior B, et al. Avaliação do estado nutricional pré e pós-operatório em pacientes submetidos à cirurgia ortognática: estudo piloto. Rev. Cir. Traumatol. Buco-Maxilo-Fac. 2013; 13(4):79-88.
23. Demário RL, Sousa AA, Salles RK. Comida de hospital: percepções de pacientes em hospital público com proposta de atendimento humanizado. Ciênc. saúde coletiva. 2010; 15(Supl.1):1275-82.
24. Garcia RWD. A dieta hospitalar na perspectiva dos sujeitos envolvidos em sua produção e em seu planejamento. Rev Nutr. 2006; 19(2):129-44.
25. Diez-Garcia RW, Padilha M, Sanches M. Alimentação hospitalar: proposições para a qualificação do serviço de alimentação e nutrição, avaliadas pela comunidade científica. Ciênc. saúde coletiva. 2012; 17(2):473-80.
26. Matos E, Pires DEP. Práticas de cuidado na perspectiva interdisciplinar: um caminho promissor. Texto & contexto enferm. 2009; 18(2):338-46.
27. Santos LF, Oliveira LMAC, Montefusco SRA, Barbosa MA. Diagnósticos e intervenções de enfermagem em famílias de crianças hospitalizadas. Rev. enf. UERJ. 2016;24(4):e 8253