(*)Teste exato de fisher; (**) Elastic bands and protective plate
ORIGINAL RESEARCH
Sociodemographic, clinical and self-care aspects of persons with intestinal stoma
Rosane Sousa de AndradeI; Jéssica Martinelli Martins II; Lays Pinheiro de MedeirosIII; Amanda Jéssica Gomes de SouzaIV; Gilson de Vasconcelos TorresV; Isabelle Katherinne Fernandes CostaVI
I
Stomal therapy nurse. Master, Federal University of Rio Grande do Norte.
Natal, Brazil. E-mail: rosanesousa@yahoo.com.br
II
Nurse of the Rio Grande do Norte League Against Cancer. Natal, Brazil.
E-mail:
jessicamartinellim@hotmail.com
III
Nurse. PhD student in nursing, Federal University of Rio Grande do Norte.
Natal, Brazil. E-mail: laysp_medeiros@hotmail.com
IV
Nurse. PhD student in nursing, Federal University of Rio Grande do Norte.
Natal, Brazil. E-mail:
amandajessicags@yahoo.com.br
V
Nurse. Post-Doctor in Nursing. Full Professor, Federal University of Rio
Grande do Norte. Natal, Brazil. E-mail: gilsonvtorres@hotmail.com
VI
Nurse. PhD in Nursing. Adjunct Professor, Federal University of Rio Grande
do Norte. Natal, Brazil. E-mail: isabellekfc@yahoo.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.19368
ABSTRACT
Objective: to examine sociodemographic, clinical and self-care aspects of patients with intestinal stoma. Method: this cross-sectional study of 89 ostomized persons in Rio Grande do Norte State, from January to March 2015, used a sociodemographic, clinical and selfcare assessment instrument, and calculated descriptive and inferential statistics. Approved by the research ethics committee (CAAE: 19866413.3.0000.5537). Results: predominantly males (51, 57.3%), older than 50 years (51, 57.3%), with companion (51, 57.3%) and with stoma for more than 6 months (71, 79.8%), permanent (51, 57.3%), and caused by neoplasms (53, 59.6%). In self-care, 83 (93.3%) emptied their pouch unaided and 67 (75.3%) attached the new pouch to the skin during changeover. Having a stoma for more than 6 months and no companion were found to associate positively with self-care. Conclusion: persons with a stoma for more than 6 months and no companion returned better scores for hygiene- and pouch-related self-care.
Keywords: Ostomy; health profile; self-care; nursing.
INTRODUCTION
Stoma originates from the Greek word stoma, meaning an artificial opening surgically created when there is a need to divert the normal transit of food and/or eliminations1.
When undergoing surgery, the individual may receive the news that they will have a stoma, and this is a difficult situation to be experienced. In this context, the creation of a stoma is a unique moment in the life of a patient and his family, marked by the feeling of insecurity. Having to live with a stoma significantly affects the intimate, familial and social relationships of the individual2,3.
The problems caused by the stoma are related to personal conditions and external variable factors such as quality of housing, financial conditions and family dynamics. The experience of cancer and a colostomy has a two-fold impact on the person's life; the first is caused by the uncertainty of healing and the possibility of imminent death, and the second by the deterioration of the image, problems with the stoma, excretion, shame, denial, distress, fear of rejection or even coping with the situation2,4.
Therefore, it was considered relevant to carry out this study in order to obtain data of epidemiological importance for a better knowledge of individuals enrolled in the Specialized Center for Habilitation and Rehabilitation of Rio Grande do Norte (CERHRN), which provides assistance to stoma patients. Therefore, this study aimed to analyze the sociodemographic, clinical and self-care aspects of patients with an intestinal stoma (IS) assisted at the Reference Center for Rehabilitation of Rio Grande do Norte.
LITERATURE REVIEW
The stoma consists of a communication between organs or viscera and the external environment created by means of surgical techniques, aiming at feeding, breathing, drainage and elimination. Intestinal stoma or colostomy is one of the elimination ostomies, and refers to an exteriorized colon; there are also ostomies relating to the ileum. They can be temporary or permanent5-7.
The main complications related to the surgical technique include an inadequate adaptation of the ostomy appliance due to a poor stomal location in the abdominal wall, dermatitis, fistula, peristomal hernia and abscess, ischemic necrosis, retraction, prolapse and stenosis, among others 8.
Regardless of the type of stoma, the patient may feel strangeness, for the mutilation of the body and the use of a collecting bag imposes the need to reconstruct the own identity. There is the loss of the highly valued organ, and consequently a loss of self-esteem, self-concept, social status, leading to depression, anger, disgust and sense of worthlessness, as well as changes in sex life, and concerns about odors and feces elimination during intercourse9,10. However, the difficulties faced by stomized people vary from one individual to another.
METHODOLOGY
This is a cross-sectional, analytical and quantitative study. A convenience sample was used, resulting in 89 people with IS assisted in the CERHRN. The inclusion criteria were: 18 years old or older, receiving care in the CERHRN, presenting a colostomy or ileostomy and being able to answer the research questions. The exclusion criteria were: concomitant presence of feeding and elimination stoma or two types of elimination stoma (urinary + intestinal) or wet colostomy. The project obtained a favorable Opinion from the Research Ethics Committee of the Federal University of Rio Grande do Norte, CAAE: 19866413.3.0000.5537.
Data collection was performed from January to March 2015 and a clinical evaluation instrument with adaptation was used11, with items related to sociodemographic and clinical aspects, material for cleaning of the stoma and exchange of collection bag and self-care with cleaning and collecting device.
The sociodemographic variables included in the instrument were: sex, age, occupation, schooling, marital status, religion and monthly income. Clinical variables included: time elapsed after the creation of the stoma, cause, permanence, location, used/adjuvant devices. Regarding the variables related to the cleaning material and exchange of collection bag, the following were highlighted: material used in the washing, material to remove the device, and how the stoma is measured.
Regarding self-care with the stoma and collection devices, four were related to hygiene and focused on emptying, washing, and cleaning the stoma, and drying the peristomal skin; and six were related to the bag - on handling the fastener, removing the bag, measurement, base molding, trimming and attachment of the bag to the skin. For all of these variables, a positive value of one was given to patients who performed self-care without assistance and zero to those who needed help.
The collected data were entered into a database and exported to a software for statistical analyses. Descriptive analysis was performed with absolute and relative frequencies, as well as inferential analysis. The Fisher's exact and chi-square tests were used in some associations, and the Mann Whitney test was used to verify associations between self-care variables and sociodemographic aspects. The statistical significance level adopted was p-value ≤ 0.05 for all tests.
RESULTS AND DISCUSSION
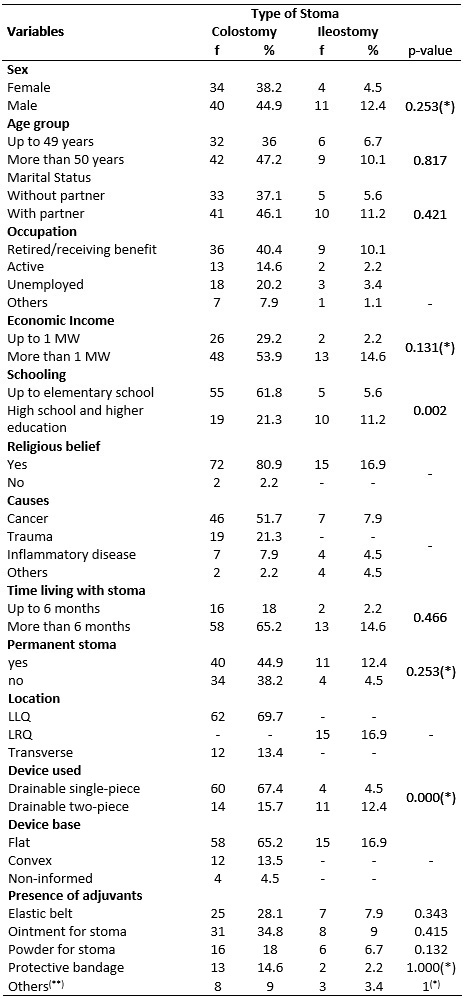
In this study, the sample consisted of 89 people, of whom 74 (83.1%) had a colostomy and 15 (16.9%) ileostomy. In the sociodemographic characterization, there was a predominance of males - 51 (57.3%), over 50 years of age - 51 (57.3%), with a partner - 51 (57.3%), retired/receiving benefit - (50.5%), with a monthly income of at least one minimum wage - 61 (68.5%), with schooling up to elementary school - 60 (67.4%), and declared religiosity - 87 (97.8%), as shown Table 1.
TABLE 1: Distribution of sociodemographic and clinical characteristics
per type of stoma. Natal, RN, Brazil, 2015. (N = 89)
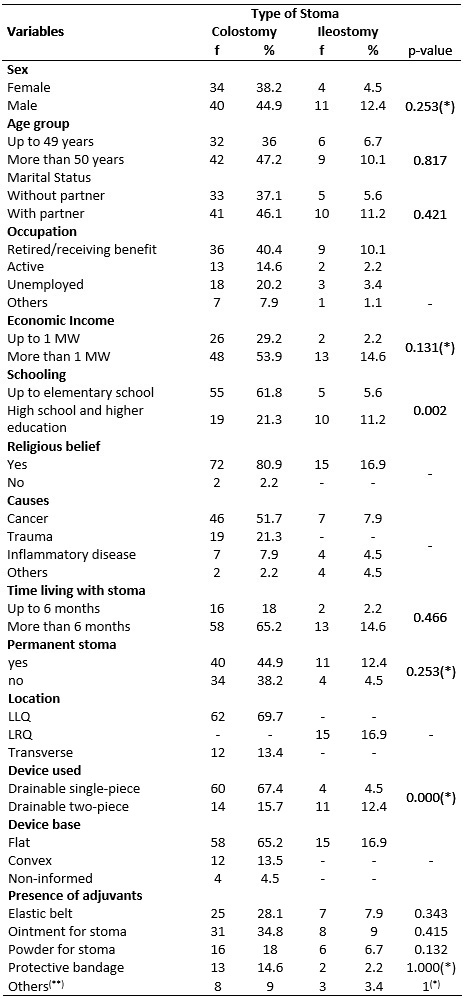
(*)Teste exato de fisher; (**) Elastic bands and protective plate
Studies show that in 2010, there were 190,755,799 inhabitants in Brazil, of which 51% of the population were women. In addition, data from the National Cancer Institute report that about 17,530 women would develop colorectal cancer in 2014, in contrast to 15,070 men12,13. Such a finding may be explained by the use of a convenience sample, because during the data collection, the invited participants who were willing to answer the questionnaire were mostly men. Moreover, trauma (motor vehicle accidents, firearm perforations, and damage caused by firearm projectilesand melee weapons) was the second cause of stomization, and such events affect more men than women.
As for age, people over 50 years old predominated, in line with some articles analyzed14. It is noted that associated with this age group, neoplasias appear as the main motivating cause for intestinal shunting. This can be observed, among many factors, due to inappropriate feeding. Contemporary society shows to make use of easy fast foods, which have low fiber, vitamin and mineral contents, and increase the propensity to develop gastrointestinal diseases. Older age groups also reflect the increased life expectancy of the population and advances in treatment technologies15,16. Furthermore, there is evidence that the consumption of red meat and processed meat is also a risk factor for the development of colorectal cancer that can culminate in the need for stomization17.
As for marital status, a great part of the interviewees had a companion, a finding similar to some studies8,14. The importance of such information comes from the fact that the support provided by a partner is a relevant and fundamental factor for the psychosocial adaptation, exerting positive effects on the quality of life of the couple. This is important because, besides instrumental support, it shows that having a stoma does not undermine the value that the person has, or the feeling that the partner has towards the patient. Likewise, lack of support has a negative impact on the adaptive processes of the person with a stoma. They experience negative changes in the patterns regarding sexuality in marriage, culminating in disgust in the process of adaptation18-21.
Regarding occupation and schooling, it was noticed that the majority of people with stoma were retired or unemployed and had studied until elementary school, data that are in consonance with other studies1,14.
The average monthly income of the group analyzed was around R$ 1,800.00. Such a finding can be explained by the fact that it is a heterogeneous clientele in its social aspect. These people are forwarded from both public/philanthropic and private hospitals. Customers from private hospitals have higher purchasing power. Also, the number of retirees prevailed because this is a sample with a predominant age range of 50 to 70 years. These findings corroborate studies conducted in another state22. Religiosity stood out in the study population, for the majority has a religious link. Spiritual support is a source of resilience and is fundamental in the process of adaptation of people with a stoma, helping to promote positive expectations in this new phase of life23.
Regarding the clinical characteristics, it was observed that the most common cause of stomization was cancer - 53 (59.6%), and there was a prevalence of people with stoma for more than six months - 71 (79.8%), with permanent stoma - 51 (57.3%), using a single-piece device - 64 (68.5%) with a flat base - 73 (82.0%), using stomal ointment as an adjunct, applied in less than half the sample - 39 (43.8%), according to Table 1.
Such findings are similar to other studies involving people with an intestinal stoma, in which permanent colostomies due to colorectal neoplasia and created for more than two years pravailed24,25.
Regarding questions on self-care related to hygiene, it was observed that 83 (93.3%) participants emptied and washed the bag without the assistance of other people. However, 74 (84.3%) cleaned the stoma and peristomal skin and 72 (80.9%) dried the peristomal skin. Regarding self-care related to the bag, 83 (93.3%) handled the fastener and 75 (84.3%) removed the bag for exchange. Sixty-six (74.2%) participants measured the stoma and cut the base without assistance and 67 (75.3%) did the molding of the base, as well as fixed it on the skin, as shown in Table 2.
TABLE 2:
Distribution of self-care measures with the stoma/device. Natal, RN,
Brazil, 2015. (N = 89)
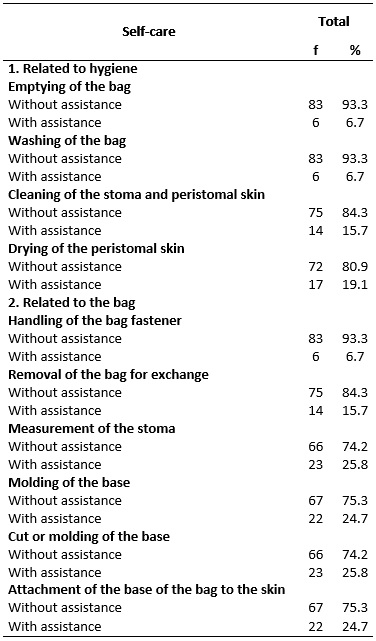
It is important to emphasize that the ability to perform self-care should be assessed based on the skills of the patients and relatives to do these measures, so that they may come to a consensus about the care measures that they are able to assume. The role of nursing in this process is also noteworthy. Nurses seek to support patients at all times to favor the planning of teaching the persons with a stoma and their families. They provide also professional support to enable the physiological recovery and rehabilitation reach of the patient26,27.
As the correlation of sociodemographic and clinical variables with self-care variables, statistical significance was observed in the association between time after creation of the stoma and marital status. Patients living for more than 6 months with the stoma and who had no partner obtained better self-care scores related to hygiene and the bag, as shown in Table 3.
TABLE 3:
Association between time since the creation of the stoma and marital status
with self-care, Natal, RN, Brazil, 2015. (N = 89)

This finding shows that adaptation to self-care arises over time. The absence of a companion in this context encourages the person with a stoma to seek support to learn how to perform hygiene and handle the device, since there is no partner to take care of such a procedure.
It is worth mentioning that when health professionals assist stomized patients, they should be aware of the types of intestinal stomies and the care measures needed during the change of the collecting bag and hygiene, as well as early detection of complications and prevention measures to avoid changes in the stoma and, above all, they should provide guidance to the client/family aimed at self-care. Therefore, it is essential to empower the persons with IS for self-care28,29.
CONCLUSION
The study showed that the majority of stomized patients were males over 50 years old, had a partner, were retired/received benefit, had a monthly income of at least one minimum wage, level of education up to elementary school, and declared to be religious. It was also observed that the most frequent cause of creation of stoma was cancer, and individuals had the stoma for more than six months, had permanent stomies, use of flat-base drainable single-piece device and used adjuvant ointment.
With regard to self-care related to hygiene, it was observed that most participants emptied and washed the bag and cleaned the stoma without assistance, in addition to cleaning and drying the peristomal skin. Most participants handled the fastener and removed the bag for exchange, measured the stoma, cut the base, did the molding of the base, and fixed it on the skin without assistance.
In the association tests, it was evidenced that the patients living for more than 6 months with the stoma and who did not have a partner reached better self-care scores related to hygiene and the bag.
Regarding the limitations of this research, the selected sample represents a local reality and, thus, the findings can not be generalized.
REFERENCES
1.Stumm EMF, Oliveira ERA, Kirschner RM. Profile of ostomized patients. Scientia Medica. 2008; 18(1): 26-30.
2.Paula RAB, Santos VLCG. Estudo retrospectivo sobre as complicações do estoma e da pele periestomal. Rev. Bras. Coloproct. 1999; 19(Esp.): 155-63.
3.Teles AAS, Eltink CF, Martins LM, Lenza NFB, Ssali VDM, Snobe HM. Physical, psychosocial changes and feelings generated by intestinal ostomy for the patient: integrative review. Rev enferm UFPE on line. 2017; 11(Supl.2): 1062-72.
4.Kimura CA, Kamada I, Guilhem DB, Modesto KR, Abreu BS. Perceptions of ostomized persons due to colorectal cancer on their quality of life.J. coloproctol. 2017; 37(1):1-7.
5 .Kamada I, Faustino AM, Silva AL, Vieira ABD, Borges CT. Conhecimento acerca da estomia intestinal por pacientes acompanhados em um serviço ambulatorial de enfermagem em estomaterapia: estudo qualitativo. Rev Estima. 2011; 9(4): 21-7.
6.Sampaio FAA, Aquino PS, Araújo TL, Galvão MTG. Nursing care to an ostomy patient: application of the Orem´s theory. Acta Paul. Enferm. (Online) 2008; 21(1): 94-100.
7.Oliveira G. Impacto da ostomia: sentimentos e habilidades desenvolvidos frente à nova condição de vida. Rev Estima. 2010; 8(1):18-24.
8.Santos CHMS, Bezerra MM, Bezerra FMM, Paraguassú BR. Profile of the pacient with stoma and complications related to stoma. Rev. Bras. Coloprocto. 2007;27(1): 9-16.
9.Cascais AFMV, Martini JG, Almeida PJS. Ostomy impact in the process of human living (Online ).2007;16(1):163-7.
10.Freire DA, Angelim RCM, Souza NR, Brandão BMGM, Torres KMS, Serrano SQ. Self-image and self-care in the experience of ostomy patients: the nursing look. REME – rev min enferm. 2017; 21: 1019.
11.Silva J. Education for self-care of the intestinal ostomy patient at home: from planning to evaluation results [masters dissertation]. Ribeirão Preto,(SP): Universidade de São Paulo; 2013.
12.Instituto Brasileiro de Geografia e Estatística (IBGE). Demographic Census 2010. Brasília: IBGE; 2010.
13.Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimate 2014: incidence of cancer in Brazil. Rio de Janeiro: INCA; 2014.
14.Silva ACS, Silva GNS, Cunha RR. Caracterização de pessoas estomizadas atendidas em consulta de enfermagem do Serviço de Estomaterapia do Município de Belém-PA. Rev Estima 2012; 10(1):12-19.
15.Macedo TMB, Schmourlo G, Viana KDAL. Fibra alimentar como mecanismo preventivo de doenças crônicas e distúrbios metabólicos. Rev. UNI. 2012: 2 (2): 67-77.
16.Melotti LF, Bueno IM, Silveira GV, Silva MEN, Fedosse E. Characterization of patients with ostomy treated at a public municipal and regional reference center. J. Coloproctol. 2013; 33(2): 70-4.
17.Zandonai AP, Sonobe HM, Sawada NO. The dietary risk factors for colorectal cancer related to meat consumption. Rev. Esc. Enferm. USP. 2012; 46(1): 234-9.
18.Karabulut HK, Dinic L, Karadag L. Effects of planned group interactions on the social adaptation of individuals with an intestinal stoma: a quantitative study. J. Clin. Nurs. 2014; 23: 2800-13.
19.Sousa AFL, Queiroz AAFLN, Mourão LF, Oliveira LB, Marques ADB, Nascimento LC. Sexuality for the ostomized woman: contribution to nursing care. Rev. pesqi. cuid. fundam. (Online). 2013; 5(6): 74-8.
20.Altschuler A, Ramirez M, Grant M, Wendel C, Hornbrook MC, Herrinton L, et al. The influence of husbands' or male partners' support on women's psychosocial adjustment to having an ostomy resulting from colorectal cancer. J. Wound Ostomy Continence Nurs. 2009; 36(3): 299-305.
21.Vera SO, Sousa GN, Araújo SNM, Sexuality of patients with bowel elimination ostomy. Rev. Fund. Care. (Online) 2017; 9(2): 495-502.
22.Aguiar JC, Pereira APS, Galisteu KJ, Lourenção LG, Pinto MH. Clinical and sociodemographic aspects of people with a temporary intestinal stoma. REME – rev min enferm. 2017; 21:1013.
23.Bulkley J, McMullen CK, Hornbrook MC, Grant M, AltschulerA, Wendel CS, Krouse RS. Spiritual well-being in long-term colorectal cancer survivors with ostomies. Psychooncology. 2013; 22(11): 2513–21.
24.Violin MR, Mathias TAF, Uchimura TT. Profile of colostomized clients enrolled in program of attention to the ostomized. Rev. eletrônica enferm. 2008; 10(4): 924-32.
25.Sasaki VDM, Pereira APS, Ferreira AM, Pinto MH, Gomes JJ. Health care service for ostomy patients: profile of the clientele. J. Coloproctol. 2012; 32(3): 232-9.
26.Silva J, Sonobe HM, BuettoLS , Santos MG, Lima MS, Sasaki VDM. Teaching strategies for self-care of the intestinal stoma patients. Rev. Rene. 2014; 15(1): 166-73.
27.Moraes JT, Santos CF, Borges EL. From training to practice: nurse supervisors' perceptions of ostomy care. Rev. enferm. UERJ. 2016; 24(2): 14733.
28.Farias RCM, Souza NVDO, Gonçalves FGA, David HMSL, Pires AS, Amorim LKA. Resident nurses' knowledge of care for people with intestinal ostomy. Rev. enferm. UERJ. 2015; 23(5): 656-61.
29.Borges EL. The role of nurses in stomatherapy and Brazilian law: progress and growth area. Rev. enferm. Cent. O. Min. 2016; 6(2).