Note: (*) PR: Prevalence ratio / (**)CI: Confidence interval.
ORIGINAL RESEARCH
Hepatitis B vaccination and associated factors among nursing personnel at a university hospital
Mônica Ferreira de AguiarI; Cássio de Almeida LimaII; Jair Almeida CarneiroIII; Andréa Maria Eleutério de Barros Lima MartinsIV; Jaciara Aparecida Dias SantosV; Fernanda Marques da CostaVI
I
Specialist in Surveillance and Control of Infections Related to Health Care
by the State University of Montes Claros. Montes Claros, Minas Gerais,
Brazil. E-mail: mofeag@yahoo.com.br
II
Master in Health, Society and Environment from the Federal University of
the Jequitinhonha and Mucuri Valleys. Montes Claros, Minas Gerais, Brazil.
E-mail: cassioenf2014@gmail.com
III
PhD student in the Graduate Program in Health Sciences of the State
University of Montes Claros. Professor of the Integrated Colleges
Pythagoras of Montes Claros. Montes Claros, Minas Gerais, Brazil. E-mail: jairjota@yahoo.com.br
IV
PhD in Epidemiology. Professor of the Graduate Program in Health Sciences
of the State University of Montes Claros. Montes Claros, Minas Gerais,
Brazil. E-mail:
martins.andreamebl@gmail.com
V
Academic of the Undergraduate Medicine Course of the State University of
Montes Claros. Montes Claros, Minas Gerais, Brazil. E-mail: jaciarapds@gmail.com
VI
PhD in Health Sciences. Professor of the Integrated Colleges Pythagoras of
Montes Claros. Montes Claros, Minas Gerais, Brazil. E-mail: fernandafjjf@yahoo.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.18856
ABSTRACT
Objective: to identify Hepatitis B vaccination coverage of nursing personnel at a university hospital and investigate the factors associated with HB vaccination among them. Method: this quantitative cross-sectional analytical study was conducted between August and November 2013 in Montes Claros, Minas Gerais. A questionnaire addressing sociodemographic and occupational variables was applied. Associations were investigated by multivariate analysis (Poisson regression), using the Statistical Package for the Social Sciences 18.0. The project was approved by the Research Ethics Committee (Documented Opinion 2882/2011). Results: participants were 399 nursing personnel, 71% of whom reported having taken three doses of the vaccine. Associations were found between vaccination prevalence and age, professional category, weekly workload, work shift, job satisfaction and training. Conclusion: hepatitis B vaccination prevalence did not meet recommended goals and was associated with important sociodemographic and occupational factors.
Keywords: Vaccination; hepatitis B; nursing; occupational health.
INTRODUCTION
Hepatitis B (HB) represents one of the most important pathologies in public health in all continents. HB virus (HBV) infection is considered a major cause of acute and chronic liver disease. Its transmission is maily caused by contact with body fluids, by parenteral, sexual and vertical routes. Contamination also occurs by vehicles such as blood, and can be spread by contact with semen, saliva, sweat, tears, breast milk and pathological effusions1-3.
There are approximately 325 million chronic HBV carriers in several regions of the world and it is estimated that more than 500,000 people die annually from this disease1,4. In Brazil, the Ministry of Health estimates that 15% of the population has already been exposed to HBV, and that 1% suffer from chronic HB2. In the state of Minas Gerais (MG) - Brazil, 6,525 cases were reported between 2010-2015, with a higher frequency in the age group of 10 to 19 years and in the North region, besides a great lack of knowledge about the disease5.
However, the access to vaccination against HB in Brazil is public and has no cost to users of the Unified Health System (SUS). There has been a significant reduction in endemic levels in the country as a result of national control strategies, especially vaccination of infants, adolescents and adults aged 49 years or over. It is reported that health workers have been vaccinated since 1993 and the coverage of complete series ranged from 53% to 76% in the years 2005, 2006 and 20106.
When health workers carry out their activities, they are exposed to contamination, mainly due to contact with biological material. This may predispose to the risk of acquiring blood-borne infections, including HBV infection, as their activities require frequent contact with patients, especially the handling of piercing materials and body fluids7. For being unhealthy places, hospitals pose a risk of occupational hazards to health workers8. Among these workers, nursing professionals get exposed to several risks during patient care: physical, chemical, mechanical, biological, and ergonomic risks that may compromise their health and cause occupational accidents4.
The risk situation of nursing workers deserves special attention in HBV prevention measures, with vaccination being the best form of protection and one of the most relevant public health interventions. Vaccination of health workers can reduce the incidence of HBV infection by up to 95%2. The Regulatory Norm 32 (RN 32) establishes basic guidelines for implementing measures to protect the safety and health of health workers, as well as of those who carry out health promotion and care activities. The use of PPE, hand hygiene, HB vaccination, among others, are recommended9.
Given this reality, updated epidemiological information is essential and necessary, and research investigating the vaccination status of professionals is relevant. The literature3,6,8,10-14 has strongly recommended the study of the prevalence and of factors associated with HB vaccination among nursing professionals, characterizing those who have not yet been vaccinated, in order to contribute to targeting the actions aimed at reducing the incidence of this serious disease. A better understanding of the determinants of vaccination is necessary to deepen the knowledge about the problem and to make investments in the workers' health, according to the characteristics of those who have not been vaccinated3,6,8,10-14.
Such studies may also contribute to prevent and control risks in the workplace, plan effective actions and strategies to raise awareness about the ways of controlling and preventing infections, and promote worker health3,13,14. Moreover, considering the high vulnerability of nursing professionals to HB, it is believed that the present work can provide subsidies to epidemiological surveillance related to HB and worker health. This study aimed to: identify the HB vaccination coverage of nursing professionals in a university hospital and investigate the factors associated with HB vaccination among such professionals.
LITERATURE REVIEW
In the last decades, many initiatives of the Brazilian society have tried to consolidate and to implement advances in the public policies of integral attention to worker health. This was especially so in the 1970s, when the worker health movement gained strength in Brazil, guided by the defense of the right to decent and healthy work, with the participation of professionals in the decisions related to the management of productive processes and in the search for the guarantee of integral health care. However, it is noteworthy that the State policy that was in force back then prevails until the present day without substantial changes10,11.
In this sense, the investment of managers in human resources with a view to their professional stimulation and development is necessary along with the re-structuring of organizational norms and mobilization of workers. By doing so, improvements in their health practices in terms of self-care can be achieved, and workers can have the possibility to express their potentialities and difficulties at work15,16. However, in spite of efforts to formulate policies to protect the workers' health, whose most recent expression was the RN 32, there are still shortcomings with regard to the surveillance of workers in the context of vaccination and accidents with exposure to biological materials 7,17.
It is necessary that worker health surveillance be a structured element in the Unified Health System (SUS). Therefore, it is imperative that its actions be inserted in the daily life of health teams, as a mandatory element for the construction of integrality in health care. Complete vaccination and serological evidence is an essential condition among health professionals to prevent the occupational transmission of HB. There is, therefore, the possibility of expanding prevention and protection interventions18.
Among the various practices of worker health protection, it is worth noting that vaccination is a practical and efficient preventive measure against certain diseases present in the hospital environment. Immunization is a means of protection against several serious diseases to which nursing workers are constantly exposed. We stress that this is an action that must precede the occupational exams, being a specific intervention for immunopreventable biological risk factors1,10.
Currently, HBV is considered the virus with the greatest possibility of occupational transmission, but there is already protection guaranteed by the immunizing agent. However, in order to have such a guarantee, it is necessary that the professionals not only be immunized, but also perform the serological examination for detection of circulating antibodies that provide protection against HB, since not all the vaccinated individuals are seroconverted18. HB is a relevant occupational disease in the health environment and nurses are likely to acquire it if precautionary measures, both collective and individual, are not implemented. It is therefore recommended to expand on-going education strategies as well as the development of worker health surveys14.
Despite the universalization of immunization, many professionals are below the minimum required to guarantee protection against HB18. The confrontation of the barriers related to the act of immunization is still a task that demands a continuous commitment of worker health surveillance, so as to ensure the real character of protection to this professional group 17,18.
METHODOLOGY
This is a cross-sectional, descriptive and analytical study conducted between August and November 2013 among nursing professionals from a university hospital in Montes Claros, MG - Brazil.
There were 487 nursing professionals in the university hospital, of which 93 were nursing assistants, 296 were nursing technicians and 98 were nurses. The number of subjects investigated was defined by a sample calculation using the following parameters: 95% confidence level, 50% ratio, and 2% error. In this sense, the estimated sample was 406 workers. Professionals who accepted to answer the proposed questionnaire and who were present in the work place were included in the investigation. Up three attempts of application of the questionnaire were made in different moments. The exclusion criteria were: being on vacation or sick leave.
The data were collected through a self-applied questionnaire. The dependent variable was investigated through the self-report of vaccination; workers who took three doses of the vaccine against HB were considered vaccinated, and those who took one, two or no doses were considered non-vaccinated. The independent variables were grouped as follows:
- Socio-demographic aspects: age, sex, marital status (with partner and without partner), schooling, monthly income. Except for sex and marital status, the other variables were categorized with the median as the cutoff point.
- Occupational history: position in the hospital, categorized into three levels: superior (nurse), middle (nursing technicians) and fundamental (nursing assistant); time working in the profession; time working in the hospital; work regime (dichotomized in peremament or hired); weekly workload (up to 39 hours and 40 hours or more); work shift (morning, night, morning and night); self-report of contact with sharps. The quantitative variables time working in the profession, time working in the hospital, and weekly workload were categorized considering the median as cutoff point.
- Satisfaction with work: satisfied (considering the categories very satisfied and satisfied) or dissatisfied (considering the categories moderately satisfied and dissatisfied). It was also investigated whether the worker had been invited to be vaccinated against HB after he entered the hospital or not, and if he had participated in any training course and/or discussion on worker health promoted by the institution.
After the collection, an electronic database was built in the Excel® software. The collected data were double entered and later validated to verify the consistency between the two bases. This bank was then imported to the Statistical Package for the Social Sciences (SPSS) version 18.0 to carry out the analyses. Absolute and percentage frequencies were used for descriptive analysis. After descriptive analysis, the association between the self-report of vaccination and the independent variables was checked through bivariate analysis and multivariate Poisson regression (with robust estimator), with estimates of gross and adjusted prevalence ratios. Variables associated with self-report of vaccination which had a p-value ≤ 0.20 in the bivariate analysis were included in the multivariate analysis. The final model was adjusted, and the variables associated with a p-value ≤ 0.05 were maintained in the model. The significance level of 95% was adopted.
The ethical aspects of the research were respected, according to Resolution 466/2012 of the National Health Council. The research project was approved by the Research Ethics Committee of the institution by means of the Consubstantiated Opinion 2882. All participants signed an informed consent form.
RESULTS
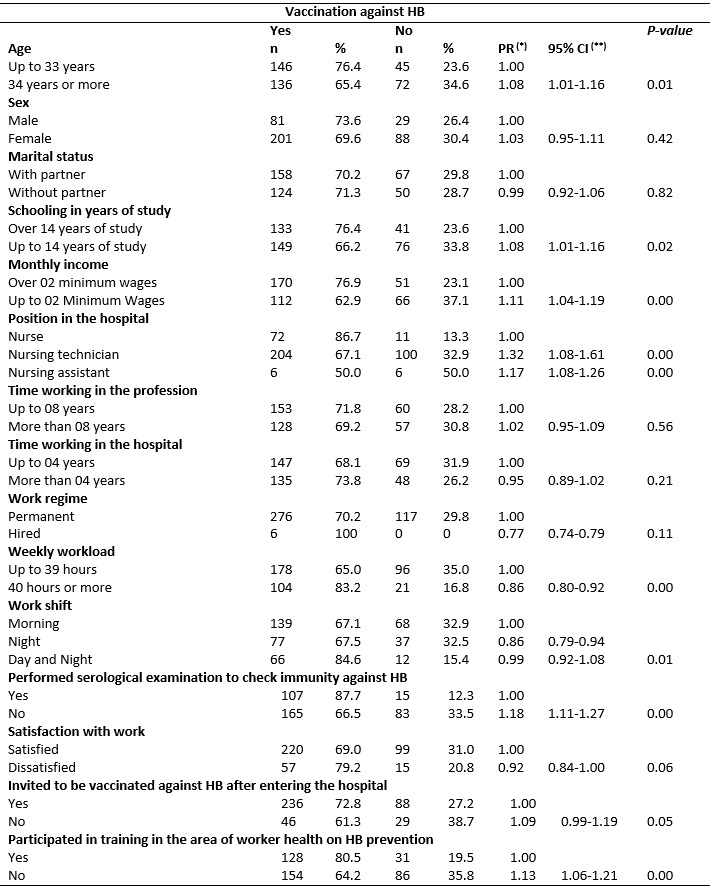
Of the 487 nursing professionals in the university hospital, 406 were drawn from the sample calculation. Of these, 400 (98.5%) accepted to respond to the proposed questionnaire and 399 (98.2%) answered the question about vaccination against HB. Among the participants, 282 (71%) reported having taken three doses of the HB vaccine and 117 (29%) received no dose or did not complete the vaccination schedule. The factors associated with the report of HB vaccination in the bivariate analysis (p ≤ 0.20) were: age, schooling, monthly income, position in the hospital, work regime, weekly workload, work shift, immunization against HB, satisfaction with work, having been invited to be vaccinated when entered the hospital, and having participated in training courses in the area of worker health with emphasis on HB prevention, as shown in Table 1.
TABLE 1:
Results of the bivariate analysis of the variables of reports of
vaccination against HB among nursing professionals of a school hospital.
Montes Claros, MG, 2013. (N = 399).
Note: (*) PR: Prevalence ratio / (**)CI: Confidence
interval.
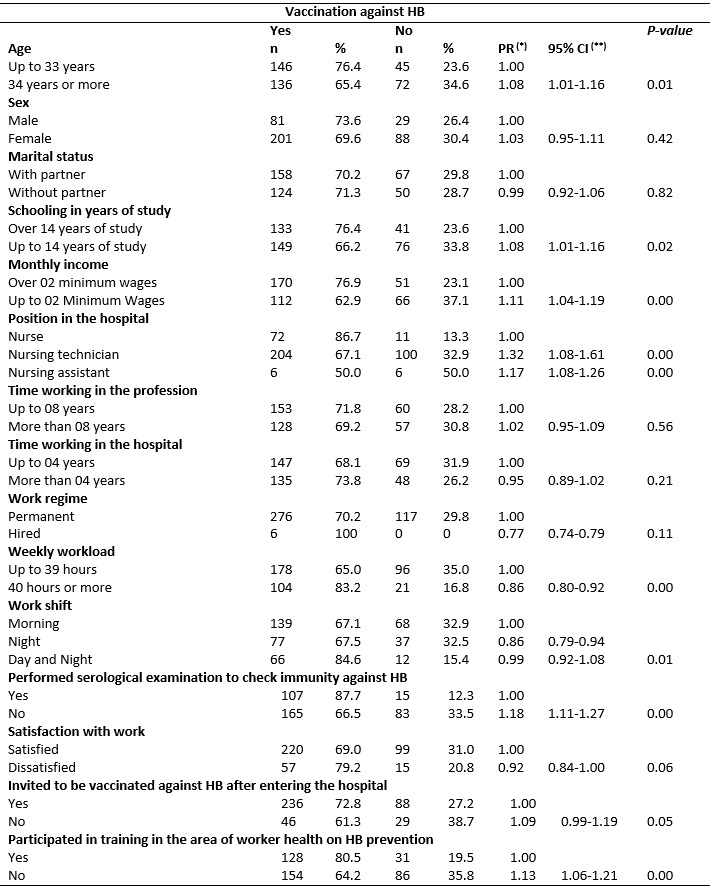
The multivariate analysis showed a lower prevalence of self-report of vaccination among professionals: younger professionals, nursing technicians or assistants, who work up to 39 hours a week, in the night shift or day and night shift, dissatisfied with work activities, and who participated in training related to HB, as shown in Table 2. Therefore, these professionals are not vaccinated against HB.
TABLE 2:
Factors associated with the report of vaccination against hepatitis b among
nursing professionals in a school hospital. Montes Claros, MG, 2013. (N =
399).
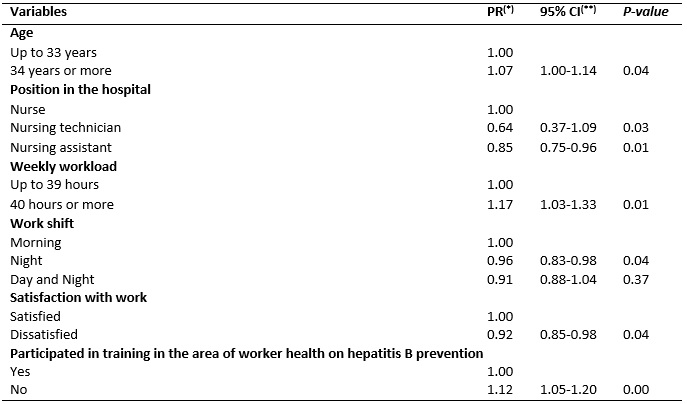
Note: (*) PR: Prevalence ratio / (**)CI: Confidence
interval.
DISCUSSION
This work allowed knowing the prevalence and the factors related to the report of vaccination against HB among the nursing professionals of a university hospital, as well as the characteristics associated to the lower prevalence of this report. Thus, younger professionals, who were nursing technicians and assistants, who work up to 39 hours a week, in the night shift or day and night shift, who are dissatisfied with the work and participated in training related to HB are the main non-vaccinated against HB.
Among the participants, 282 (71%) reported having taken three doses of the HB vaccine and 117 (29%) received no dose or did not complete the vaccination schedule. In other university hospitals, the prevalence of vaccination was 73.9%3, 64.2%8 and 53.2%19 .
Thus, the hospital did not achieve the desired levels. A disturbing reality is presented herein, because the article 168 of Law 7,855/89 recommends the realization of admission tests only after confirmation of complete vaccination schedule against HB20. Vaccination coverage of nursing professionals can be improved because the vaccine against HB is available in the public system and is the most effective way to prevent HB, since the vaccine response in immunocompetent adults is 90 to 95%21,22.
Therefore, such findings require a detained discussion. The lack of information, lack of training and low educational level are the main factors that lead to non-vaccination against HB15. According to studies, low level of education among healthcare workers may be related to low knowledge and consequently, a smaller percentage of vaccination and serologic testing; these workers are therefore the less protected among their peers3. Professionals who are not vaccinated may be unaware of the forms of HB transmission, or of the number of doses recommended by the Ministry of Health to obtain the immunization, besides having little knowledge and self-care toward their own health, neglecting important measures such as vaccination3,23. Additionally, the training of health professionals is still focused on technicality. Gaps between patient care and the caregiver's self-care still persist, making it difficult to promote worker health23.
Situations such as lack of an adequate worker health plan with protocols to guide and monitor the implementation of the complete HB vaccination schedule may translate into important occupational risks, considering that the chance of HBV infection is very high for non-immune professionals. It has been estimated that workers in the hospital network who are contaminated with contaminated percutaneous materials have a higher risk of being infected with HBV (6% to 30%), while the rates of contamination with hepatitis C virus (0.5% to 2% %) and with HIV/AIDS (0.3%) are lower , thus reiterating the need for 100% of vaccination and monitoring for HB immunization among health workers23,24. Thus, the role of the Epidemiological Surveillance Center in this research scenario should stand out. This organ should be aware of the vaccination status of institutional professionals, monitoring of HB, and implementation of preventive measures.
Contrary to expectations, there was a lower prevalence of reporting of HB vaccination among professionals under 34 years of age who participated in training in the area of worker health. Therefore, younger nurses should be the primary target for HB prevention and control actions. Investments in training and vaccination campaigns against HB need to be increased, focusing also on the importance of knowledge and awareness on disease prevention. It is essential to strengthen continuing and permanent education, emphasizing this vaccination, prevention of work-related accidents, attention in the moment of carrying out the procedures, as well as compliance with biosafety standards8,25.
Nursing professionals with higher education had a higher prevalence of reported vaccination compared to those of technical and auxiliary levels. This can be explained by the fact that they are more aware of occupational risks9,16,23,24, have greater knowledge of occupational health3,13,15,23 or because they were vaccinated during graduation3,15. A similar situation of higher frequency of vaccination among professionals with better schooling has been found in other studies3,13,14,19,26-28.
The recommendation of the need to complete the vaccination schedule against HB is already a reality in some higher education institutions. This may be one of the reasons that contributed to a higher prevalence of vaccination among workers with this type of training29. However, a study that investigated the knowledge of nursing students about HB vaccination found that the knowledge of these students was partial and varied among universities. Therefore, the determination of a specific and clear protocol to be followed by all institutions of higher education during nursing training is advisable30.
The prevalence of HB vaccination was lower among nursing professionals who worked up to 39 hours per week, among those who worked at night or day/night shifts, and among those who reported being dissatisfied with work. It is probable that professionals who work at night shifts suffer from work overload, are dissatisfied with the activity performed, and end up postponing self-care23. Similar results were found in health units located in the northern region of the state of Ceará, where the members of the nursing team who work between 30 and 88 hours a week also adopt less care measures with their health compared to those who work with a lower weekly workload31.
The work overload associated with the work shift, especially during the night shift, may interfere with the quality of life of these individuals. Such a situation can deteriorate the health of the workers, lead to increased accidents, risk of disease, dangerous exposures, and less concern with occupational safety and health, as well as lower vaccination rates against HB19. This study found that, although the investigated workers have a stable bond with the institution, low remuneration is present and this interferes negatively in the satisfaction with the work and consequently in the quality of life and self-care, also reducing the adherence to the vaccination against HB.
It is necessary and urgent that nursing professionals recognize their vulnerability and take on a preventive stance toward biosafety and their own health. It is also important that these professionals be aware of issues related to the prevention of work-related diseases, as it is well known that occupational risks in this profession are present, as well as precarious working conditions32,33.
As concrete proposals, this research evidences the need for protocols to promote worker health, with general measures that include: complete vaccination schedule, moments to carry out post-immunization verification, moments for stress reduction. Programs to stimulate physical activity and the adoption of a healthy lifestyle should be implemented, instigating workers to incorporate self-care measures toward their health that may be a way to positively influence the satisfaction with the work, which was so impaired among the professionals investigated.
In addition, there is a need to stimulate workers with career plans, programs that avoid wage losses over time, allowing them to remain satisfied at work. It should be stressed that the implementation of these protocols will contribute to meeting what was recommended by the Ministry of Health through the National Policy on Worker Health in 2011, when the "National Policy Guidelines for Promotion of Worker Health in the Unified Health System" were published. Such guidelines recognize that work quality and health promotion are associated with the deprecarization of work and the establishment of a consistent health plan for workers34.
CONCLUSION
The prevalence of HB vaccination among the nursing professionals of the university hospital has not yet reached the levels recommended to ensure their health with regard to HBV infection. Thus, younger professionals, who were nursing technicians and assistants, who worked up to 39 hours a week, in the night shift or day and night shift, who were dissatisfied with the work and who participated in training related to HB are the ones that are most often non-vaccinated against HB.
It is recommended that all workers provide a confirmation of vaccination at the moment of admission to health services and that the institution be attentive to the vaccination and occupational health status of its professionals. This deserves special mention in the scenario of the present work, since it is a teaching hospital that should be a model for undergraduates, whose training must include a clear emphasis on prevention through an effective action to break the epidemiological chain of communicable diseases, namely, vaccination. The need for more information about the importance of the HB vaccine and the verification of post-vaccination immunization is reiterated.
This work presents limitations because it was based on self-reported data. Therefore, the results may be overestimated, since it takes into account the workers' reports, who may opt for answers that are considered correct, even if they do not represent the reality of their practice. The interviewers were trained to minimize this bias, ensuring participants of the confidentiality of the information. However, self-reported information is commonly used in epidemiological studies. Longitudinal surveys should be performed in order to clarify the factors associated with non-vaccination and to establish a causal relationship.
REFERENCES
1.Fraguás SA, Silvino ZR, Flach DMAM, Reis IR, Andrades M. Immunization against Hepatitis B: a matter of occupational health nursing. Rev pesq cuid fundam online [online journal]. 2013 [cited in Jan 22, 2014]; 5(1):3150-8. Available at: http://www.seer.unirio.br/index.php/cuidadofundamental/article/view/1865/pdf_671
2.Ministry of Health (Br). Health Surveillance Secretariat. Epidemiological Surveillance Department. Viral hepatitis: Brazil is alert. Brasília (DF): Ministry of Health; 2008.
3.Soares DM, Lima CA, Costa FM, Carneiro JA. Nursing: reality of immunization against Hepatitis B in a hospital of the north of Minas Gerais. Esc Anna Nery. 2015; 19(4):692-701.
4.Simão SAF, Soares CRG, Souza V, Borges RAA, Cortez EA. Occupational accidents with sharp materials involving nursing professionals of the emergency unit. Rev enferm UERJ. 2010; 18(3):400-4.
5.Minas Gerais. State Health Secretariat of Minas Gerais. Subsecretariat for Health Surveillance and Protection. Superintendence of Epidemiological, Environmental and Occupational Health Surveillance. Epidemiological surveillance directorate. Epidemiological warning - Yellow June, 2017. Belo Horizonte (MG): State Health Secretariat of Minas Gerais; 2017.
6.Álvarez AMR, Pérez-Vilar S, Pacis-Tirso C, Contreras M, Nathalie El O, Cuauhtémoc Ruiz-Matus, et al. Progress in vaccination towards hepatitis B control and elimination in the Region of the Americas. BMC Public Health. 2017; 17: 1-10.
7.Paiva MHRS, Oliveira AC. Determining factors and conducts after accidents with biological materials among prehospital care professionals. Rev Bras Enferm. 2011; 64 (2): 268-73.
8.Ruas EFG, Santos LS, Barbosa DA, Belasco AGS, Bettencourt ARC. Occupational Accidents with Sharpening Materials in Montes Claros-MG Hospitals. Rev Min Enferm. 2012; 16(3):437-43.
9. Ministry of Labor (Br). Regulatory Norm 32, of November 11, 2005: provides on health and safety at work in health services. Brasília (DF): Ministry of Labor; 2005.
10.Dias MP, Lima CJM, Nobre CS, Feijão AR. Vaccine profile of nursing professional in a hospital reference in infectious diseases in Fortaleza - Ceará. Cienc Cuid Saude. 2013; 12(3):475-82.
11.Costa D, Lacaz FAC, Filho JMJ, Vilela RAG. Worker health in the SUS: challenges for a policy. Rev Bras Saúde Ocup. 2013; 38(127):11-30.
12.Dannetun E, Tegnell A, Torner A, Giesecke J. Coverage of hepatitis B vaccination in Swedish health care workers. J Hosp Infect. 2006; 63(1):201-4.
13.Costa FM, Martins AMEBL, Santos NPE, Veloso DNP, Magalhães VS, Ferreira RC. Is vaccination against hepatitis B a reality among Primary Health Care workers? Rev Latino-Am Enfermagem. 2013; 21(1):316-24.
14. Araújo TME, Costa e Silva N. Accidents with sharps and preventive measures for hepatitis B adopted by nursing professionals in the urgency and emergency services of Teresina, Piauí. Rev Bras Saúde Ocup. 2014; 39(130):175-83.
15.Martins AMEBL, Costa FM, Ferreira RC, Santos-Neto PE, Magalhães TA, Barbosa de Sá MA, et al. Factors associated with immunization against Hepatitis B among workers of the Family Health Strategy Program. Rev Bras Enferm. 2015; 68(1):84-92.
16.Pinto IC, Panobianco CSMM, Zacharias FCM, Bulgarelli AF, Carneiro TSG, Gomide MFS, et al. Analysis of job satisfaction of the nursing staff of a primary health care unit. Rev Gaúcha Enferm. 2014; 35(4):20-7.
17.Siqueira Julio R, Filardi MBS, Marziale MHP. Occupational accidents with biological material in municipalities of Minas Gerais. Rev Bras Enferm. 2014; 67(1):119-26.
18.Souza FO, Freitas PSP, Araújo TM, Gomes MR. Vaccination against hepatitis B and anti-HBS among health workers. Cad Saúde Colet. 2015; 23(2):172-9.
19.Noronha DD, Vieira MRM, Vieira MM, Magalhães TA, Leite MTS. Occupational accidents occurred among the health professionals of the Clemente de Faria University Hospital - HUCF. Motri. 2012; 8(2):67-77.
20.Ministry of Health (Br). Law 7,855 of 1989. Brasília (DF): Ministry of Health; 1989.
21.Ministry of Health (Br). Manual of reference centers for special immunobiologicals. Brasília (DF): Ministry of Health; 2006.
22.Ministry of Health (Br). Fundacentro. Manual of implementation: program of prevention of accidents with sharps in health services. Brasília (DF): Ministry of Health; 2010.
23.Pinheiro J, Zeitoune RCG. Hepatitis B: knowledge and bio-security measures and the health of nursing workers. Esc Anna Nery. 2008; 12(2):258-64.
24.Oliveira AC, Gonçalves JA. Occupational accidents by sharp material among health professionals of a surgical center. Rev Esc Enferm USP. 2010; 44(2):482-7.
25.Sanches GBS, Honer MR, Pontes ER, Aguiar JI, Ivo ML. Seronoepidemiological characterization of hepatitis B virus infection in primary health care professionals in the State of Mato Grosso do Sul, Brazil. Rev Panam Infectol. 2008; 10(2):17-5.
26.Silva RJO, Athayde MJPM, Silva LGP, Braga EA, Giordano MV, Pedrosa ML. Anti-hepatitis B vaccination among healthcare professionals. DST J Bras Doenças Sex Transm. 2003; 15(1):51-5.
27.Vos D, Götz HM, Richardus JH. Needlestick injury and accidental exposure to blood: the need for improving the hepatitis B vaccination grade among health care workers outside the hospital. Am J Infect Control. 2006; 34(9):610-20.
28.Garcia LP, Facchini LA. Vaccination against hepatitis B among primary health care workers. Cad Saude Publica. 2008; 24(5):1130-40.
29.Ministry of Health (Br). Ordinance 597 / GM 08 April 2004. Brasília (DF): Ministry of Health; 2004.
30.Yamazhan T, Durusoy R, Tasbakan MI, Tokem Y, Pullukcu H, Sipahi OR, et al. Turkish Nursing Hepatitis Study Group. Nursing students' immunisation status and knowledge about viral hepatitis in Turkey: a multi-centre cross-sectional study. Int Nurs Rev. 2011; 58(2):181-5.
31.Caetano JA, Soares E, Braquehais AR. Occupational accidents with biological material in the routine of nursing in a high complexity unit. Enferm Glob. 2006; 1(9):1-12.
32.Moradi T, Maghaminejad F, Azizi FI. Quality of working life of nurses and its related factors. Nurs Midwifery Stud. 2014; 3(2):194-50.
33.Zimmerman RK, Raymund M, Janosky JE, Nowalk MP, Fine MJ. Sensitivity and specificity of patient self-report of influenza and pneumococcal polysaccharide vaccinations among elderly outpatients in diverse patient care strata. Vaccine. 2003; 21(13-14):1486-91.
34.Ministry of Health (Br). Management Secretariat of Health Work and Education, Secretariat Health Surveillance National Permanent Negotiation Committee of SUS. Protocol nº 8. Brasília (DF): Ministry of Health; 2011.