RESEARCH ARTICLES
Evaluation of waiting times for initial electrocardiogram in patients with Acute Coronary Syndrome
Karla Biancha Silva de AndradeI; Ana Paula Brito PinheiroII; Amanda Trindade Teixeira de BessaIII; Graciele Oroski PaesIV; Marluci Andrade Conceição StippV
I
Nurse at the National Cancer Institute. PhD in nursing. Adjunct Professor of the Cardiovascular Program of Nursing Residence at the Nursing School of Rio
de Janeiro State University. Brazil. E-mail: karla.biancha@gmail.com
II
Assistant Nurse at the Emergency Unit of the Pro-Cardiac Hospital. Master in Nursing by the Federal University of the State of Rio de Janeiro. Brazil.
E-mail: appinheiro@hotmail.com
III
Nursing Student and Scholar of the Institutional Scholarship Program for Scientific Initiation, National Scientific and Technological Development Council -
Anna Nery School of Nursing, Federal University of Rio de Janeiro. Brazil. E-mail: amandattb@gmail.com
IV
Adjunct Professor at Anna Nery School of Nursing, Federal University of Rio de Janeiro. Brazil. E-mail: inamachado@globo.com
V
Associate Professor at Anna Nery School of Nursing, Federal University of Rio de Janeiro. Brazil. E-mail: marlustipp@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.18332
ABSTRACT
This study examined waiting times to first electrocardiogram (ECG) in patients with suspected acute coronary syndrome in the emergency room, and discussed its implications in managed care for this clientele. A cross-sectional study was conducted at a private hospital in Rio de Janeiro municipality. In January and February 2010, 116 electrocardiograms were performed, and mean time to initial EEG was 22 minutes. In patients with acute ST segment elevation myocardial infarction (STEMI), mean time was 7.5 minutes. In the physicians' reports, 2.5% were diagnosed as STEMI; 7.1% as non-ST segment elevation myocardial infarction, and 16.6% as unstable angina. It was concluded that timely initial ECG contributes to the identification and early treatment of patients with STEMI. However, some adjustments are still needed to improve health teams' adherence to recommended times.
Keywords: Acute coronary syndrome; emergency service; professional practice management; nursing.
INTRODUCTION
Cardiovascular disease accounts for the major mortality data in developed countries, and coronary artery disease or acute coronary syndrome (ACS) accounts for 42% of such deaths1-3. In Brazil, recent data from the World Health Organization (WHO) show that cardiovascular diseases, particularly acute myocardial infarction (AMI), represent the main cause of mortality and disability, responsible for the occurrence of more than 100,000 deaths every year 4,5.
Among signs and symptoms experienced by individuals with acute myocardial infarction, chest pain is the most common. This pain is usually characterized by strong intensity, oppression, weight or burning sensation, radiating to the arms (usually the left arm), preceded by unusual effort and alleviated with rest. However, studies show that 40% of patients diagnosed with AMI may not present the typical chest pain but, instead, stomach pain, sensation of indigestion, chest discomfort and pain in the dorsal region6-8.
Therefore, by obtaining detailed history of the pain characteristics, evaluating the presence of factors of risk for coronary artery disease, documented previous myocardial infarction and atherosclerotic disease as well by performing the electrocardiogram (ECG) as soon as possible, early diagnosis of AMI is made more likely8-11.
Many therapeutic strategies have modified the clinical evolution of patients with AMI at the hospital setting. However, effectiveness of the majority of such strategies and the best results depend on the time elapsed before its implementation. Thus, early identification and treatment of individuals who are developing AMI are crucial for the best management of care toward ACS patients in health institutions10-13.
Associated with this understanding, studies show that ECG is the most informative procedure for initial diagnosis of patients with non-traumatic chest pain treated at emergency services9-15. A delayed time preceding the realization of ECG may result in worse prognosis in these patients, as consequence of a greater area of cardiac muscle affected14-17. Due to this, the following question was raised: How much time does it take to perform the initial ECG in patients with suspected acute coronary syndrome in the emergency room?
The result of the ECG is the key for therapeutic strategy in patients with chest pain in this setting13,15. In this perspective, the present study purposed to document the time preceding the first ECG in patients with suspected acute coronary syndrome in emergency rooms and to discuss its implications for the process of managed care directed to this clientele.
The culture of making sure that the best practices proposed by scientific evidence and guidelines are actually being adopted by health teams is incipient in Brazil. In contrast, government agencies of developed countries have health care quality indicators that can be used by institutions for continuous improvement of the process care and this way adopt a better management9-17. Therefore, there is an imperative need for raising information on the results of the assistance in order to make possible an enhanced provision of care.
LITERATURE REVIEW
The ACS is defined as the rupture of an unstable atherosclerotic plaque with possibility of thrombus formation, embolism or obstruction of coronary artery. Total occlusion of the blood vessel configures an acute ST Elevation Myocardial Infarction (STEMI). Partial occlusion of the vessel constitutes a Non-ST-Elevation Acute Myocardial Infarction (NSTEMI) also denominated unstable angina14-16.
Management of the process of care in cases of AMI is based on rapid diagnosis, immediate clearance of the affected coronary artery and maintenance of optimal blood flow, which are all directly linked to the patient's prognosis and must be performed as soon as possible in order to reduce the injury of the myocardium and enhance survival14-16,18.
In contrast, an strategy of care that aims early identification or discard of an AMI was elaborated by the American Heart Association (AHA) for approaching patients with suspected AMI. According to the American guidelines and the Brazilian Society of Cardiology (Sociedade Brasileira de Cardiologia - SBC), the health team must perform the initial ECG as soon as the patient arrives at the hospital informing chest pain complaint13,15,16.
The electrocardiogram is the most widely used diagnostic test in the initial evaluation of patients with chest pain and suspected ACS because it is a low-cost, noninvasive and readily available method in emergency rooms, and it must be the first examination of this clientele7,10, 12-13,15.
The standardization of specific quality indicators for the care process directed to patients with ACS has been organized and implemented by the American Heart Association through the Clinical Practice Guidelines of the American Heart Association (ACC/AHA)14,15. Since then, the SBC in Brazil has followed and recommended professionals to use these indicators to manage and evaluate care in patients with ACS14-16.
Examples of indicators used to assess the processes related to care in cases of ACS in the hospital setting that have been formalized by national and international guidelines include counseling for smoking cessation, the time between onset of symptoms and arrival for medical care, time preceding the first ECG, time between onset of symptoms and management of venous thrombolytic or the first balloon inflation, in case of percutaneous coronary intervention9,12-18.
A ACC/AHA, juntamente com a SBC, preconiza que todos os pacientes com SCA ou suspeita de SCA precisam realizar ECG. E idealmente o ECG deve ser realizado e interpretado em até 10 minutos após a chegada do paciente ao hospital, tornando-se o ponto central do processo decisório inicial em pacientes com suspeita de IAM14-16.
The ACC/AHA, along with the SBC, recommends that all patients with ACS or suspected ACS must perform ECG. Ideally, the ECG should be performed and interpreted up to 10 minutes after arrival of the patient to the hospital, becoming a central point of the initial decision making in patients with suspected AMI14-16.
The suitability of this strategy has justification in the fact that electrocardiographic changes of myocardial ischemia happen before the area of necrosis or infarction is installed, giving the health team the opportunity to intervene and restore blood flow before death of myocardial cells 6-8, 12,14,17.
Despite this recommendation, only a third of the patients have their ECG performed and interpreted within 10 minutes after arrival in the emergency room 14,17.
A long duration of time preceding ECG may contribute to poor clinical outcome in patients with ACS, since the delay in the acquisition of ECG may result in late action, impacting directly on decisive actions that may save the myocardium, such as administration of venous thrombolytic or for performing percutaneous coronary angioplasty 7,9,12-15,17.
The success of care provided to a patient with STEMI is time dependent. Ideally, this person must receive the treatment of reperfusion of the affected coronary artery by primary angioplasty within 90 minutes (door-to-balloon time) or through the administration of intravenous thrombolytic therapy within 30 minutes after arrival at hospital (door-to-needle time)7, 13-17.
Thus, the formulation of protocols and guidelines that conduct and manage the care process, as well as monitor the results, is essential to improve the quality of assistance provided by the health team that operates the initial treatment of this clientele. Concomitantly, research works focusing on the improvement of quality of health care try to bridge the gap and establish a link between the ideal and the practiced care in the health system 6,7,10,12,13,18 .
In addition, non-adherence to guideline recommendations and consensus that guide good clinical practice may cause negligence during the professional performance and also real harm to treated patients (adverse events and/or sentinels)9-10,12-14,17-18.
The level of desirable quality of care provided to patients with ACS is determined by the obtainment of information on the performance of the health team and interpreting this information in order to identify opportunities for improvement in the care process10,18,19.
METHODOLOGY
This is a cross-sectional study of descriptive type and document analysis, conducted between January and February 2010 in a private hospital in the city of Rio de Janeiro.
The survey was conducted in a setting specialized in cardiology, a reference in the State of Rio de Janeiro, with 20 beds, electronic medical records and the use of a systematic protocol for care of patients with suspected ACS, according to the guidelines of the ACC/AHA/SBC.
Nursing staff that works in this scenario consists of 10 nurses and operates all stages of systematic protocol, speeds up diagnostic and therapeutic procedures as well as manages the care directed to this clientele by the health team. Management occurs through monitoring quality indicators of care, namely, waiting time to perform the first ECG, Time Gate balloon and counseling for smoking cessation.
Documental analysis was done on 116 ECGs of patients with suspected ACS in the emergency room and, later on, records were evaluated in order to gather sociodemographic and comorbidity variables.
Initial ECGs of patients over the age of 18 with chest pain treated at the emergency service were included. Electrocardiograms of patients who were transferred to another institution and ECGs without service identification tag were excluded due to impossibility of measuring the indicator.
A structured form with 12 questions related to socio-demographic data including age, sex and comorbidities, and information on the waiting time for completion of the ECG was designed.
Waiting time for ECG was assessed considering the time interval (Δt) between the time of arrival and time of completion of ECG. For this, the time specified in the ID tag given at the reception (which record the date, time, age and sex) and the time of completion of ECG recorded in the electrocardiogram itself were consulted.
A search on medical records of individuals who underwent ECG was performed in order to survey comorbidities.
According to research procedures, the clinical engineering staff of the institution synchronized the clock time of the electrocardiogram device with the clock of the information system of the emergency reception room so that it was possible to assess the precise time elapsed between arrival of the patient and completion of the first ECG. This was done during the two months of data collection of the present study.
According to ethical research procedures19, the study was submitted to the Research Ethics Committee of the institution concerned and approved under the Opinion No. 246 on March 12, 2008. The study was initiated after approval by the head of the unit.
Data were collected and analyzed using simple statistics. Information obtained generated a database, basing the creation of charts and graphs, using MS-Excel software version 2007.
RESULTS AND DISCUSSION
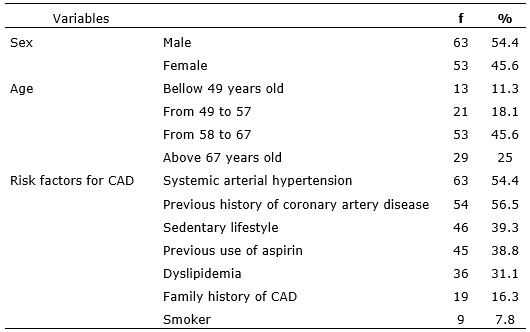
Among 116 (100%) patients who had their first EGC evaluated, 63 (54.4%) were male and 53 (45.6%) were female and the average age was 66.3 years. Sixty-three (54.4%) patients had systemic arterial hypertension, and 54 (56.5%) had a previous history of coronary artery disease (CAD). See Table 1.
TABLE 1: Demographic and clinical profile of patients who had
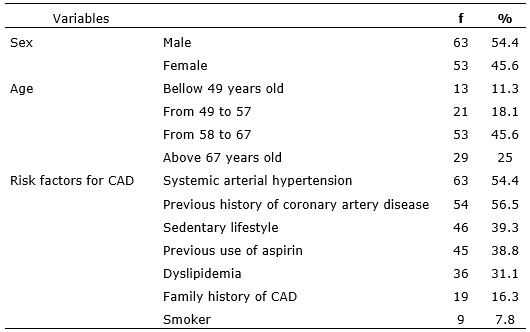
Results of the survey show that there were differences between sexes, with 63 (54.4%) male and 53 (45.6%) female patients. The mean age was 66.3 years. This is consistent with findings in literature concerning incidence of cardiovascular disease, which are equal in women in the menopausal stage, and may experience risk increased up to three times when compared to men of the same age20,21.
Clinical manifestations of coronary artery disease in women appear nearly 10 to 15 years later than in men, probably due to estrogenic protection. Women who are obese, sedentary and smoke more than men show higher incidence of hypertension after 45 years old, and nearly half present hypercholesterolemia after 55 years old6,20,21.
This research showed a considerable number of patients with more than one factor of risk for cardiovascular disease, representing 63 (54.4%) of the population. Among risk factors, hypertension and previous family history of CAD prevailed. Other parallel cardiovascular risk factors can make these more complex and make the person vulnerable to the development of a new cardiac event.
It is noteworthy that 46 (39.3%) participants did not practice any physical activity. This represents an important piece of information, taking into account that the practice of physical exercise has a protective effect against cardiovascular diseases22.
Regular practice of aerobic physical activity is indicated for prevention of cardiovascular disease when performed at least five times per week 17, 19-21.
Furthermore, physical inactivity is included in the list of the major risk factors for cardiovascular diseases and high blood pressure, diabetes mellitus, obesity and dyslipidemia20-24.
Regarding the waiting time for completion of ECG, 22 minutes in average elapsed between arrival of the patient with suspected ACS and completion of the first ECG. This average was 7.5 minutes in the case of patients with STEMI. According to medical records, 33 (26.1%) assessed ECGs had final medical diagnosis of ACS, 3 (2.5%) were diagnosed with STEMI, 9 (7.1%) were diagnosed with NSTEMI and 21 (16.6%) were diagnosed with unstable angina (UA). It is noteworthy that 83 (71.5%) patients had diagnoses other than ACS.
Many factors may have contributed to difficult to reach the time recommend by national and international guidelines. These are overcrowding in the unit, systematic care protocol yet not adjusted, decreased sense of urgency in patients whose pain seems mitigated during the period of waiting for initial treatment in the emergency room and the non-continuous evaluation of instituted care process10,12,16.
Another possibility is the non-appreciation of the ACC/AHA and SBC recommendations by the health team, as well as lack of appreciation of the consequences of this delay in the outcome of patients with ACS8,10,11,15,17,24.
Despite the fact that the time elapsed for the first ECG in patients with suspected ACS did not follow the recommendations of guidelines, it was observed that patients with STEMI had the average ECG time of 7.5 minutes.
It is easy to understand this difference in time when we realize that individuals who develop STEMI in the initial ECG arrive at emergency rooms with stronger symptoms typical of an urgent situation25, which seems to be better understood by the health staff and lead it to rapidly perform the ECG in this population.
Increased importance has been given to early and efficient identification of patients with acute myocardial ischemia in emergency services and in spite of the presence of various forms of clinical symptoms, nearly 80% of them manifest chest pain as the first symptom7-12,26.
These data showed that, although the institution studied has a systematic protocol of care for patients with chest pain, there are still adjustments to be made in order to improve the process of care directed to ACS.
This understanding strengthens the need for health services not only to instruct the managed care through care protocols based on the best scientific evidence in order to minimize failures and increase service quality, but also to carry out continuous evaluation of the process in search for weaknesses and opportunities to implement improvements 27.
Care is considered appropriate when an intervention has an expected health benefit and is greater than the risk for those who need the care system 10,12,27.
Adherence to standards can be ensured by maintaining the process of care offered to a certain selected population under continuous observation, and comparing this care to a list of quality indicators and pre-established guidelines27.
The health team must focus on systems that give subsidies for acquisition of initial ECG within ideal time frame. This structure requires efforts of a multidisciplinary group and of care providers working in the emergency room, including doctors, nurses and hospital administrators16.
Emergency nurses are professionals who make a difference in the care for patients with suspected ACS and can contribute to the achievement of stablished times, whether through the operation of steps of systematized protocols, or through management of the process of care aiming at improvement in the unit 10,13,16.
CONCLUSION
In the current global scenario, monitoring indicators that translate the actual outcome of care ministered to patients with ACS is a growing concern of health care institutions that focus on continuously improving quality of care.
Thus, the systematization of health care actions through treatment protocols for these patients in order to provide a thorough assessment of pain, aiming at early recognition and treatment of individuals who are developing AMI is important for a safer care process.
A careful process directed to rapid and correct management of patients with chest pain in the emergency room must be adopted. This approach needs to have structure, organization and incorporation of current guidelines, ensuring realization of optimal therapy for symptoms suggestive of ACS.
Timely completion of the initial ECG contributes to the early identification and treatment of patients with STEMI and reduces mortality. Good results of reperfusion therapy depend on the time spent for ECG diagnosis. However, this time is still unfrequently mentioned in reports of care quality management of patients with ACS by health institutions, what makes the findings of the present research important.
The discussion about the results of the present research considered that the methods used to measure the quality of the process of care in cases of ACS include continuous assessment and adherence to standards established for professional practice.
Thus, the management of care directed to this clientele should be focused on identifying opportunities for improvement, making the necessary interventions, reassessing and restructuring it in order to enhance safety and quality of care processes in acute coronary syndrome.
This study has some limitations. First, the results may apply for a given specific institution, but cannot be generalized to all hospitals that treat patients with suspected ACS. This study was restricted to an emergency room of a private hospital, where the main feature is the specialized care through protocol for patients with chest pain. Second, barriers impeding the realization of initial ECG within the desired time were not discussed, as they require further research to address this dimension.
In this way, new studies related to the theme are needed, with other methodologies, in order to evaluate control interventions and reduce the time for initial ECG. New studies must also cover a more representative sample, thus contributing to strengthening of adherence to standards set out in care management ACS.
REFERENCES
1.Labarthe DR, Dunbar SB. Global cardiovascular health promotion and disease prevention: 2011 and beyond. Circulation. 2012;125:2667-76.
2.Vedantham R, Seligmam B, Fuster V. Global perspective on acute coronary syndrome a burden on the young and poor. Circulation Research. 2014; 114: 1959-75.
3.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988-2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation. 2012;125:2595-602.
4.Ministério da Saúde. Datasus. Mortalidade geral. [citado em 30 out 2014]. Disponível em http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sim/cnv/ obt10uf.def.
5.World Health Organization. Global status report on noncommunicable diseases 2014.Attaining the nine global noncommunicable diseases targets; a shared responsibility. Geneva (Swi). WHO; 2014.
6.DeVon HA, Ryan CJ, Rankin SH, Cooper BA. Classifying subgroups of patients with symptoms of acute coronary syndromes: a cluster analysis. Res Nurs Health. 2010; 33: 386-97.
7.Kamali1 A, Söderholm M, Ekelund U. What decides the suspicion of acute coronary syndrome in acute chest pain patients? BMC Emergency Medicine. [cited in 2014 Oct 21] 2014; 14:9. http://www.biomedcentral.com.
8.Lemos DM, Teixeira CSS, Polanczy CA, Rabelo ER. Gatilho da dor em pacientes com síndrome coronariana aguda. Rev Enferm UFSM. 2012;2(3):480-6.
9.Rocha ASC, Araújo MP, Volscham A, Carvalho LAF, Ribeiro A, Mesquita ET. Melhora assistencial no infarto do miocárdio. Full texts in English. [citado em 12 out 2014]. Disponível em http://www.arquivosonline.com.br.
10.Ruth RFF, Silva LP. Estudo exploratório das iniciativas acerca da segurança do paciente em hospitais do Rio de Janeiro. Rev enferm UERJ. 2014; 22:22-8.
11.Viviane Rassele Silva VR, Cade NV, Molina MCB. Risco coronariano e fatores associados em hipertensos de uma unidade de saúde da família. Rev enferm UERJ. 2012; 20:439-44 .
12.Hamilton AJ, Swales LA, Neill J, Murphy JC, Darragh KM, Rocke LG, et al. Risk stratification of patients with ischaemic type chest pain assessed in the emergency department utilizing a point of care (POC) protocol. European Journal of Emergency Medicine. 2008;15(1):9-15.
13.Felices–Abad F, Latufo-Pérez J, Fuset-Cabanes MP, Ruano-Marco M, Cuñat-de la Hoz J, Nogal-Sáez F, et al. Indicadores de calidad en el sindrome coronario agudo para el analisis del proceso asistencial pre e intrahospitalario. Medicina Intensiva. 2010; 34:397- 417.
14.Nicolau JC, Franken M, Lotufo PA , Carvalho AC, Neto JAM , Felipe Gallego Lima1, Dutra O et cols. Tratamento da coronariopatia aguda no Brasil. Arq Bras Cardio. 2012;98:282-9.
15.Nicolau JC, Timerman A, Piegas LS, Marin-Neto JA, Rassi Jr A. Guidelines for unstable angina and non-st-segment elevation myocardial infarction of the Brazilian Society of Cardiology. Arq Bras Cardiol. 2007; 89 (4): 89-131.
16.Piegas LS, Feitosa G, Mattos LA, Nicolau JC, Rossi Neto JM, et al. Sociedade Brasileira de Cardiologia. IV Diretriz da Sociedade Brasileira de Cardiologia sobre tratamento do infarto agudo do miocárdio com supradesnível do segmento ST. Arq Bras Cardiol.2009;93 (6 supl.2):179-264.
17.Hemsey JZ, Claire E, Sommargren CE, Drew BJ. Initial ECG acquisition within 10 minutes of arrival at the emergency department in persons with chest pain: time and gender differences. Journal of emergency nursing. 2011; 37(1):109-12.
18.Burman1 RA, Zakariassen E, Hunskaar S. Management of chest pain: a prospective study from Norwegian out-of-hours primary care. BMC Family Practice. 2014; [cited in 2014 Oct 20] 15:51. Available from http://www.biomedcentral.com.
19.Donabedian A. An introduction to quality assurance in health care. Oxford (USA): Oxford University Press; 2003.
20.Ministério da Saúde (Br). Conselho Nacional de Saúde. Resolução nº466/12: diretrizes e normas regulamentadoras de pesquisa envolvendo seres humanos. Brasília (DF): CNS; 2012.
21.Herdy AH, López-Jiménez F, Terzic CP, Milani M, Stein R, Carvalho T, et al. Diretriz sul-americana de prevenção e reabilitação cardiovascular. Arq Bras Cardiol. 2014; 103(2Supl.1): 1-31.
22.Shin JS, Martin R, Suls J. Meta-analytic evaluation of gender differences and symptom measurement strategies in acute coronary syndromes. Heart & Lung: The Journal of Acute and Critical Care. 2010; 39: 283-95.
23.Simão AF, Précoma DB, Andrade JP, Correa Filho H, Saraiva JFK, Oliveira GMM, et al. Sociedade Brasileira de Cardiologia. I Diretriz Brasileira de Prevenção cardiovascular. Arq Bras Cardiol. 2013; 101 (6 Supl.2): 1-63.
24.Rangul V, Bauman A, Holmen TL, Midthjell K. Is physical activity maintenance from adolescence to young adulthood associated with reduced CVD risk factors, improved mental health and satisfaction with life: the HUNT Study, Norway. International Journal of Behavioral Nutrition and Physical Activity. 2012; [cited 2015 Jul 10] 9:144. Available from: http://www.ijbnpa.org.
25.Reid RD, McDonnel LA, Riley DL, Mark AE , Mosca L, Beaton L, et al. Effect of an intervention to improve the cardiovascular health of family members of patients with coronary artery disease: a randomized trial. CMAJ. 7, 2014; 186: 23-30.
26.Franco B, Rabelo ER, Goldemeyer S, Souza EN. Pacientes com infarto agudo do miocárdio e os fatores que interferem na procura por serviço de emergência: implicações para a educação em saúde. Rev Latino-Am Enfermagem. 2008; 16: 414-18. Disponível em: http://www.eerp.usp.br/rlae.
27.Ballard N, Bairan A, Newberry L, Brackle LV, Barnett G. Effect of education on a chest pain mnemonic on door-to-ecg time. J Emerg Nurs.2011;37:220-4.