
ORIGINAL RESEARCH
Prevalence of adverse events in a hemodialysis unit
Maiana Regina Gomes de SousaI; Ana Elisa Bauer de Camargo SilvaII; Ana Lúcia Queiroz BezerraIII; Juliana Santana de FreitasIV; Gustavo Edreira NevesV; Thatianny Tanferri de Brito ParanaguáVI
I
Nurse. Master. Coordinator of the Patient Safety Center of the Emergency
Hospital of Goiânia. Brazil. E-mail: maianaregina@gmail.com
II
Nurse. PhD. Associate Professor, Faculty of Nursing, Federal University of
Goiás. Goiania, Brazil. E-mail: anaelisa@terra.com.br
III
Nurse. PhD. Associate Professor. Faculty of Nursing, Federal University of
Goiás. Goiania, Brazil. E-mail: analuciaqueiroz@uol.com.br
IV
Nurse. Master. PhD student, Faculty of Nursing, Federal University of
Goiás. Goiania, Brazil. E-mail:
ju.santana.freitas@gmail.com
V
Physician. Substitute Professor, Pontifical Catholic University of Goiás.
Goiania, Brazil. E-mail:
gustavo_edreira@hotmail.com
VI
Nurse. PhD. Adjunct Professor, Faculty of Health Sciences, University of
Brasília. Brazil. E-mail: ttb.paranagua@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.18237
ABSTRACT
Objective: to estimate and analyze the prevalence of adverse events related to hemodialysis treatment. Method: in this cross-sectional, documentary analysis study, data was collected using a structured instrument on records of 117 patients treated at a hemodialysis unit in Goiás State, between January and December 2012. Statistical analysis was performed using SPSS version 19.0. The study was approved by the Human and Animal Medical Research Ethics Committee (protocol 064/2008). Results: 1,272 adverse events were identified, and prevalence was 80.3%. The most prevalent adverse event was inadequate blood flow (40.6%). Of harm caused, 76.1% was classified as mild, 22.9% as moderate, 0.9% as severe, and 0.1% fatal. Conclusion: the study identified high prevalence (80.3%) of adverse events, pointing to a need to review the care processes and take action to diagnose and control treatment risk situations, so as to ensure patient safety.
Keywords: Patient safety; patient harm; hemodialysis units, hospital; quality of health care.
INTRODUCTION
Health care involves caring for the human being, including actions to promote, protect, maintain, rehabilitate health and treat diseases, always seeking to benefit the patient. However, health care has the potential to cause adverse events (AEs) and compromise patients safety.
Adverse events are incidents that occur during care provision that result in harm to the patient, which can be physical, social or psychological, including illness, injury, suffering, disability or death1.
A study conducted in the United States of America estimated that more than 400,000 patient die due to AEs, pointing to the urgency for changes and improvements in patient safety2.
In Brazil, a study analyzed the medical records of 1,103 patients in three hospitals in Rio de Janeiro and identified 65 preventable AEs, which were responsible for 373 additional days of hospitalization3.
These events may occur in a variety of health facility services, including hemodialysis units.
More than 1.5 million kidney failure patients in the world are estimated to undergo hemodialysis treatment4. In Brazil, approximately 112,004 patients undergo dialysis, of which 91.4% undergo hemodialysis, and this modality is mostly prescribed in the country5. These patients present characteristics that make them more vulnerable to the occurrence of AE. These include: critical health status due to the physiological consequences of renal failure, hemodynamic instability, multiple comorbidities, polypharmacy, among others6.
Furthermore, there are aspects related to the treatment itself that cause vulnerability, among which the following stand out: use of high technology equipment, such as hemodialysis machine and dialyzer filters; need for specialized multiprofessional teams; performance of invasive procedures; administration of Potentially Hazardous Medicines (PHM); and great turnover of patients.
This context suggests that providing safe care to the population that depends on hemodialysis presents some unique challenges, in addition to the general patient safety issues common to all health facilities6. Therefore, the timely detection of situations that can prompt AE is essential to understand its causes, calculate the risks and control them by means of preventive and corrective measures7.
Considering that the occurrence of AE in hemodialysis is common, often with fatal clinical complications, and also that there is a shortage of studies on this subject in Brazil, the present study aimed to estimate and analyze the prevalence of adverse events related to hemodialysis treatment, identifying their categories, severity and associated factors.
LITERATURE REVIEW
Hemodialysis is used by acute renal failure (ARF) patients who require short-term treatment, and by chronic renal failure (CRF) patients who undergo long-term treatment.
The benefits of hemodialysis depend on adequate physical structure, a specialized and trained multiprofessional team, well-designed and standardized processes, and a risk management system capable of detecting and controlling situations that may cause harm to the patient.
A study conducted in Scotland to estimate the incidence and nature of AE that contributed to the death of patients treated with renal replacement therapy revealed that, from January 2008 to June 2011, there were 1551 deaths, of which 2.1 % were caused by complications such as venous access hemorrhage and fall. Factors such as health care-related infections (9.6%) and failure or infection of the venous access (9.3%) also contributed to death in 506 cases6.
The analysis of 526 reports of hemodialysis incidents in Pennsylvania, USA, pointed out that medication errors were the most prevalent (28.5%), followed by failure to follow the protocol (12.9%), laboratory or blood bank error (9.9%), procedure complication (8.6%), needle disconnection (6.1%), puncture infiltration (6.1%), falls (5.9%), equipment failure (4.8%), extracorporeal clotting (4.4%), post-hemodialysis events (3.8%), pressure ulcers (3.8%), skin lesions (1.9%) and others (3.3%)8.
Study in four hemodialysis units in the US found the following problems in 64,541 dialysis sessions: 35 medication errors; 31 infiltrations of venous access; 30 dialysis equipment malfunction events, where 18 were related to dialysis filters, six to hemodialysis machines and six to blood lines; 19 extracorporeal system clotting events, and nine falls of patients 9.
The occurrence of AE in hemodialysis units is cause of concern because the patients are in a vulnerable situation, often dealing with unfavorable clinical conditions and critical health; any type of error can have serious consequences for their health. Therefore, preventive measures must be developed and adopted by health institutions.
In 2013, in Brazil, the Ministry of Health launched the National Patient Safety Program, representing an important health initiative in the country. The program aims to contribute to the qualification of health care in all health facilities in the national territory10.
The RDC nº 11 was created in the following year, which specifically sets out the requirements for good operating practices in dialysis services. According to this resolution, hemodialysis units must have a Patient Safety Center responsible for creating and implementing a safety plan to indicate risk situations and propose strategies for their management, seeking the prevention and reduction of AE11.
Therefore, it is necessary to know the adverse events in hemodialysis in order to work on improvements of the care practice and promotion of patient safety.
METHODOLOGY
Cross-sectional study developed through documentary analysis in the hemodialysis unit of a teaching hospital in Goiás.
The population was represented by medical charts of patients assisted from January to December 2012. All records of the care provided during the hemodialysis sessions were analyzed.
The records of 38 patients from other hemodialysis units and 18 patients that lacked information on hemodialysis sessions were excluded from the study. Thus, among 173 patients assisted during 2012, 117 (67.6%) were included in the study, resulting in the analysis of 5,938 sessions.
Data collection took place between March and September 2013 and was guided by a structured instrument with investigative questions on patients' characteristics, dialysis treatment and possible AE occurred during the care.
Data were analyzed in the Statistical Package For The Social Sciences (SPSS), version 19.0 for Windows. Records of AE represented a corpus of analysis submitted to evaluation by the researcher and by two specialists in the subject for their validation.
The AE were classified into categories according to type and severity, following the World Health Organization1 definition for classification of damage as mild, moderate, severe or death.
For exemplification of findings, excerpts were transcribed and identified by the letters P for patient and R for record, followed by a cardinal number according to the order of the medical chart.
Prevalence of AE was calculated per patient and per session, with their respective 95% confidence intervals. In the first case, the number of patients with at least one AE record was used as numerator and the total number of patients as denominator. In the second, the number of sessions with at least one EA record was used as numerator and the total number of sessions analyzed as denominator.
In order to identify the factors associated with the occurrence of the AE, a univariate analysis was performed using the Chi-square test or the Fisher's Test when necessary, and the Odds Ratio as measure of association. A multivariate logistic regression analysis was carried out with the variables gender, age and those that had p < 0.10 in the univariate analysis. The 95% confidence intervals were calculated and the associations that obtained p < 0.05 were considered statistically significant.
Exposure variables corresponded to those related to the patient (age, gender, type of renal failure and presence of other pathologies) and to treatment (treatment time, number of sessions performed, weekly frequency and duration of each session).
The research was approved by the Ethics Committee in Human and Animal Medical Research under protocol 064/2008 and complied with the precepts of Resolution nº 466/2012 of the National Health Council12.
RESULTS AND DISCUSSION
The analysis of 117 (100%) medical charts allowed us to identify that 71 (60.7%) patients were male; age varied between 1 and 89 years, with mean of 42 years and median of 45 years, and the most frequent age group was between 20 and 59 years, the case of 64 (54.7%) people; and 93 (79.5%) patients had CRF. A study with 48 CRF patients undergoing hemodialysis found that 58.3% were female and the mean age was 49 years13, different from the present results with respect to sex, and similar with respect to age.
The present study identified that the hemodialysis session duration was 3 and a half hours in the case of 59 (50.4%) patients, and 4 hours in the case of 48 (41.0%) patients; 102 (87.2%) patients received 3 sessions per week; 66 (56.4%) had been under treatment for up to three months, with a median of 2 months, but 11 (9.4%) patients had been undergoing treatment for more than 5 years.
The hemodialysis regimen of three sessions per week with duration of about 4 hours is the most commonly used in the world, called conventional hemodialysis. However, it is doubtful if this is in fact the best alternative for regular treatment. Such questioning is based on the high mortality rate and low life expectancy of patients undergoing conventional hemodialysis. In this scheme, sessions are asymmetrically distributed through the week. There is 68-hour interval without dialysis at the end of the week, when leisure and social life of patients are more intense and their demand for fluid consumption is usually increased. Thus, a consequent increasing number of complications at the beginning of the weeks is observed14.
An ideal schedule should include more frequent and/or longer hemodialysis sessions. It would be necessary to overcome economic limitations in order to offer greater safety and life expectancy to this population. In France, about four decades ago, a three-session-per-week schedule of up to 8 hours each was implemented and highly favorable results were observed. Patients' survival after 10 and 20 years was about 75% and 43%, respectively 15.
The analysis of the 5,938 hemodialysis sessions resulted in the registration of 1,272 (100%) AE, which were classified into 25 types and sorted according to severity of damages, as presented in Table 1.
TABLE 1: Distribution of adverse event types and severity of damage resulting from
assistance in the hemodialysis unit of a teaching hospital. Goiânia, GO,
Brazil, 2012

Inadequate blood flow was the most prevalent type of AE - 517 (41%) - and refers to the improper velocity of blood flow through the venous access to the extracorporeal system, including flow obstruction, reflux and flow below the prescribed level.
Double lumen catheter (DLC) with reflux without improvement with maneuvers. The patient underwent about 2 hours of hemodialysis, blood flow = 160 mL/min. Instructed to return tomorrow for DLC replacement and extra hemodialysis. (P43, R2)
Study analyzed 618 hemodialysis sessions recorded in 85 medical charts and found complications in 282 sessions; lack of flow through the venous access occurred in 24.1% of the sessions16.
Incidents related to catheter malfunction are very frequent and may be related to the patient's clinical condition, the professional's technical ability, catheter permanence time, inadequate catheter tip position, among others17.
Heparin is generally used to prevent catheter obstruction due to clot formation. However, a study indicated that the use of recombinant tissue plasminogen activator (rt-PA) once a week in the place of heparin reduced the incidence of inadequate catheter function by approximately 34% 18.
Bleeding from venous access was the second most prevalent type of AE - 148 (12%) - and severe damage was reported in two cases. This type of event may be related to the use of heparin, whose purpose is preventing blood clotting through the extracorporeal circulation system.
Child, coming from home, without complaints, in the company of his brother. He bleed throughout the session, in a surgical site opening. It was turned off with 2:36 hours, ultrafiltration = 1650 mL. The child was referred for admission to the pediatrics and awaits evaluation of the pediatric surgery. (P78, R1)
Heparin is a MPP that has the potential to cause serious injury to patients or even death if the use process fails19. Therefore, patient safety requires much attention from professionals who use heparin, from the professional who prescribes it to the one who administers it. The use of low molecular weight heparin is an alternative because this form is more effective and safe; it has a high cost tough, making it difficult to use it frequently20. Any anticoagulant is contraindicated in cases of patients with active bleeding, bleeding risk, pericarditis, in the postoperative or immediate preoperative period. High blood flow must be maintained and the circuit must be washed every 30 minutes during the session with 200 mL of saline solution20.
Extracorporeal clotting is a frequent AE and damages caused to the patient involve reduction of effective dialysis time due to interruption of the session and blood loss, which can lead to anemia and need for blood transfusion. It also increases the work for the nursing team and the costs of therapy20,21.
Patient coming from the emergency room, installed in hemodialysis via DLC, according to medical prescription without heparin. The whole system coagulated. The doctor [...] interrupted the session and decided not to resume the procedure. She requested an extra hemodialysis session for tomorrow, in the 2nd shift. Blood was collected for hemoglobin assessment, there is need for blood transfusion tomorrow on hemodialysis. (P6, R2)
Extracorporeal clotting may be related to inadequate dosage or contraindication of heparin, low blood flow, high ultrafiltration rate, the clinical condition of the patient, problems with the hemodialysis catheter or with the dialysis technique itself and the materials used21.
As for infections/signs of infection, venous access and hemodialysis units are always linked with such risk, especially due to the need for arteriovenous fistula (AVF) puncture and manipulation of the central venous catheter (CVC).
Surgical site opening with presence of purulent exudate, shown to the doctor. [...], directed to take it, what was made by me (sent to culture), results will be ready next Tuesday at 11:00, ask another test. Note: Memo of the hospital infection control service for the hemodialysis service - We declare that the following agent has been isolated in culture: Acinetobacter baumanni ( multiresistant ) in catheter from a patient of this unit. In this case, we indicate contact precautions. (P33, R4)
The risk of infection is lower for patients who use AVF. The CVCs should be used as the last alternative for long-term vascular access in order to reduce the overall risk of infectious complications in hemodialysis patients4.
Research with 156 patients on hemodialysis treatment using CVC identified that 94 had bloodstream infection. Among complications related to infection, there were 35 cases of septicemia and 27 cases of endocarditis, of which 15 progresses to death22.
Preventing and controling venous access-related infections is largely the responsibility of nursing professionals. They can guarantee a safe practice through elaboration and follow-up of protocols for handling the access 23.
Regarding the severity of the damage, the results were similar to the study that identified 218 AE in a surgical center and, of these, 170 (78.0%) were considered mild, 36 (16.5%) moderate, 5 (2.3 %) severe and 7 (3.2%) fatal 24. Serious damage and death were less prevalent, but the most important.
It is noteworthy that 3 (20%) of the AE resulting from inadequate catheter implant caused serious damage.
Suspended hemodialysis, active bleeding in the DLC and hematuria. Note: Medical record on the intensive care unit admission sheet - I receive patient from medical clinic with history of shock [...], followed-up by residents of the specialties. There was an inadvertent puncture accident of the left femoral artery - catheter was removed in this intensive care unit without complications. Nephrology team, puncture new femoral access for hemodialysis. The patient has several hematomas at the former puncture site in the right jugular vein and crust at the puncture site. (P108, R1)
Risks at CVC insertion procedure can be reduced with the use of ultrasonography, which makes it possible to evaluate the location of the vein, its diameter and adverse situations, ensuring accurate visualization of the target, as well as the progression of the needle and the guidewire. The use of this technology reduces puncture attempts, improves implant success rates, minimizes catheter-related complications, and decreases the procedure time, especially in patients with poor vascular access 25.
From all AVF rupture events, 2 (66.7%) were considered serious and 1 (33.3%) caused the death of the patient, in which AVF rupture followed the puncture in an aneurysm region.
Hemodialysis was initiated by AVF, it presents an aneurysm, the vascular physician aproved the session, I mean, punctured in the AVF. After approximately one hour of the session, the aneurysm ruptured, the patient was referred to the surgical center, accompanied by the nurse [...] and the doctor. [...] where the vascular team was waiting for him. The patient was medicated in the room, one ampoule of morphine 2 mg/2mL and protamine, one ampoule in 100 mL of saline 0.9%. (P22, R22)
The aneurysm can be caused by repetition of punctures, making the vein wall to weaken and expand26. The presence of this complication increases the risk of rupture of the fistula, requiring surgical intervention to save the life of the patient4.
Prevention of aneurysm formation relies on in good puncture technique. This prevention is fundamental for the preservation of the AVF. The recommended puncture technique is called Buttonhole2. Needles with blunt edges are used in this technique; they are introduced through a tunnel previously constructed by repeated punctures in the same place, preventing damage to the endothelium26.
Ninety-four (80.3%) out of the total of 117 (100%) patients had record of one or more hemodialysis-related AE. Thus, this represents the prevalence. Such prevalence - 80.3% - corresponds to 95% CI: 72.4% - 86.8%; 94/117. The mean of AE per patient was 10.9 (standard deviation = 14.9) and the median was 5 (minimum = 0, maximum = 65, IIQ = 1-13). It was also found that one or more AE was present in 1,036 (17.4%) out of the 5,938 sessions analyzed; the prevalence of AE per hemodialysis session was 17.4% (95% CI: 16.5% -18.4%, 1,036/5,398). The mean AE per session was 0.21 (standard deviation = 0.52) and the median was equal to zero (minimum = 0, maximum = 5; IIQ = 0-5).
It is worth noting that the prevalence of AE per patient in this study was much higher than the estimated 10.5 percent of a survey conducted in 35 hospitals of Latin America27. This can be explained by the complexity of the assistance offered in hemodialysis units, which deserves an in-depth analysis of causative factors.
The univariate and multivariate associations between exposure variables and the types of AE that occurred during hospitalizations are presented in Table 2.
TABLE 2:
Univariate association between the exposure variables and the occurrence of
adverse event in the hemodialysis unit of a teaching hospital. Goiânia, GO,
Brazil, 2012
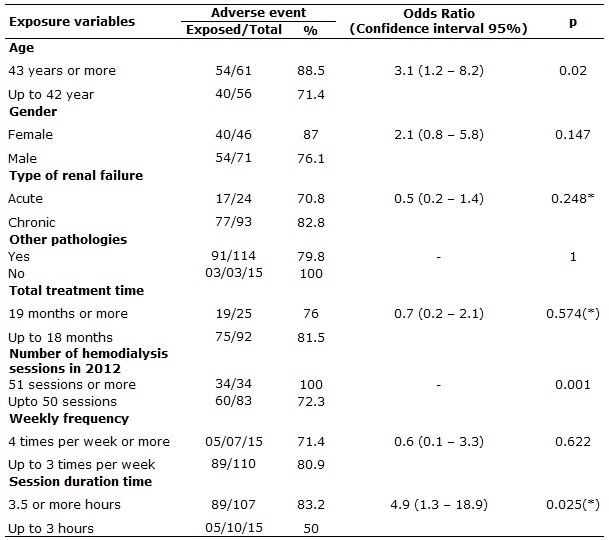
(*) Fisher exact test
Possible factors associated with the AE occurrence were: age of 43 years or more, performance of 51 or more hemodialysis sessions, and session duration equal to or greater than 3.5 hours. See Table 2.
The adjusted values of the variables that were statistically significant in the univariate analysis for exposure to AE are shown in Table 3.
TABLE 3:
Associated factors and respective odds ratio for the occurrence of adverse
event in the hemodialysis unit of a teaching hospital. Goiânia, GO, Brazil,
2012
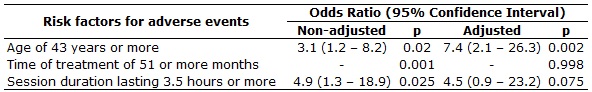
It was evident that being 43 years old or older was a risk factor for AE occurrence, increasing the chance by 7.4 times in relation to younger patients; that risk, in certain situations, was up to 26.3 times greater. See Table 3
This data may be related to the fact that older patients are, in most cases, those who have more comorbidities and a greater number of risk factors, becoming more susceptible to suffer damage from AE28.
Sessions lasting 3.5 hours or more was not statistically significant, according to Table 3, but the low p value suggests a tendency for exposure to AE. These factors indicate the need to pay more attention to the patients who present these characteristics and to prepare specific protocols for their safety during hemodialysis sessions.
CONCLUSION
This study found a prevalence of 80.3% of AE in patients undergoing hemodialysis. The most prevalent type of AE was inadequate blood flow that; most damages were classified as mild; and age equal to 43 years or more represented an independent variable associated with the AE occurrence.
The high prevalence of AE is an alarming finding. It indicates the need to review the care processes in hemodialysis units and the development of actions to diagnose and control the risks in order to promote patient safety.
This research has a pioneer nature in Brazil, according to the proposed objective. Further studies seeking to evaluate causal factors are encouraged. They may point to opportunities for improvement of care, so as to meet the needs of nephropathy patients and guarantee the quality of the care provided.
Because this was a study with secondary data source, there were limitations related to the quality of the notes in the medical charts, since detailed and important information was not always present, posing a difficulty to deepen the investigation.
REFERENCES
1.World Health Organization (WHO). Conceptual framework for the international classification for patient safety. Taxonomy. World Alliance for Patient Safety. 2009 [cited in 2016 Fev 19]. Availabe from: http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf
2.John TJ. A New, Evidence-based Estimate of Patient Harms Associated with Hospital Care. J Patient Saf. 2013 [cited in 2016 Feb19]; 9(3):122-8. Availabe from: http://journals.lww.com/journalpatientsafety/Fulltext/2013/09000/A_New,_Evidence_based_Estimate_of_Patient_Harms.2.aspx
3.Mendes W, Pavão ALB, Martins M, Moura MLO, Travassos C. The feature of preventable adverse events in hospitals in the State of Rio de Janeiro, Brazil. Rev Assoc Med Bras. 2013 [cited in 2016 Feb 19 ]; 59(5):421-8. Available from: http://www.scielo.br/pdf/ramb/v59n5/v59n5a06.pdf
4.The Renal Association. RA Guidelines – haemodialysis. Renal Association.2009 [cited in 2016 Feb 19]. Availabe form: http://www.renal.org/docs/default-source/guidelines-resources/Haemodialysis_-_Current_version_-_01_December_2009_FINAL.pdf?sfvrsn=0
5.Sesso RC, Lopes AA, Thomé FS, Lugon JR, Martins CT. Brazilian Chronic Dialysis Census 2014. J Bras Nefrol 2016 [cited in 2016 Feb 19]; 38(1):54-61. Available from: http://www.scielo.br/pdf/jbn/v38n1/0101-2800-jbn-38-01-0054.pdf
6.Bray BD, Boyd J, Daly C, Doyle A, Donalson K, Fox JG, et al. How safe is renal replacement therapy? A national study of mortality and adverse events contributing to the death of renal replacement therapy recipients. Nephrol Dial Transplant. 2014 [cited in 2016 Feb 19]; 29(3):681-7. Availabe form: http://ndt.oxfordjournals.org/content/29/3/681.long
7.Feldman LB. Gestão de risco: implicações para a prática. In: Harada MJCS. Gestão em enfermagem: ferramenta para prática segura. São Caetano do Sul.(SP): Yendis Editora; 2011. p. 325-38.
8.Pennsylvania Patient Safety Authority. Hemodialysis administration: strategies to ensure safe patient care. Patient Saf Advis. 2010 [cited in 2016 Feb 19]; 7(3):87-96. Availabe from: http://patientsafetyauthority.org/ADVISORIES/AdvisoryLibrary/2010/Sep7(3)/documents/87.pdf
9.Holley JL. A descriptive report of errors and adverse events in chronic hemodialysis units. Nephrol News Issues. 2006; 20(12):57-67.
10.Ministério da Saúde (Br). Agência Nacional de Vigilância Sanitária. Portaria nº 529, de 1º de abril de 2013. Institui o Programa Nacional de Segurança do Paciente. Brasília (DF): ANVISA, 2013.
11.Ministério da Saúde (Br). Agência Nacional de Vigilância Sanitária. Resolução RDC nº 11 de 13 de março de 2014. Dispõe sobre os requisitos de boas práticas de funcionamento para os serviços de diálise e dá outras providências. Brasília (DF): ANVISA; 2014.
12.Ministério da Saúde(Br). Conselho Nacional de Saúde. Resolução nº 466 de 12 de dezembro de 2012. Regulamenta pesquisas envolvendo seres humanos. Brasília (DF): CNS; 2012.
13.Xavier BLS, Santos I, Almeida RF, Clos AC, Santos MT. Individual and clinical characteristics of clients with chronic kidney disease on renal replacement therapy. Rev enferm UERJ. 2014 [cited in 2016 Feb 19]; 22(3):314-20. Availabe from: http://www.e-publicacoes.uerj.br/index.php/enfermagemuerj/article/view/13683/10474
14.Matos JPS, Lugon JR. Alternative hemodialysis regimens. J Bras Nefrol. 2010 [cited in 2016 Feb 19]; 32(1):114-19. Availabe form: http://www.scielo.br/pdf/jbn/v32n1/v32n1a18.pdf
15.Innes A, Charra B, Burden RP, Morgan AG, Laurent G. The effect of long, slow haemodialysis on patient survival. Nephrol Dial Transplant. 1999; 14(4):919-22.
16.Silva GLDF, Thomé EGR. Complicações do procedimento hemodialítico em pacientes com insufuciência renal aguda: intervenções de enfermagem. Rev Gaúcha Enferm. 2009 [citado em 19 fev 2017]; 30(1):33-9. Disponível em: http://seer.ufrgs.br/index.php/RevistaGauchadeEnfermagem/article/view/3844/6557
17.Ferreira V, Andrade D. Catheters for hemodialysis: a reality report. Medicina (Ribeirão Preto). 2007 [cited in 2016 Feb 19]; 40(4):582-8. Availabe from: http://www.revistas.usp.br/rmrp/article/view/355/356
18.Hemmelgarn BR, Moist LM, Lok CE, Tonelli M, Manns BJ, Holden RM et al. Prevention of dialysis catheter malfunction with recombinant tissue plasminogen activator. New Eng J Med. 2011 [cited in 2016 Feb 19]; 364:302-12. Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa1011376#t=article
19.Instituto Para Práticas Seguras no Uso de Medicamentos (ISMP). Medicamentos potencialmente perigosos de uso hospitalar e ambulatorial: listas atualizadas 2015; 2015 [citado em 19 fev 2016]; 4(3):1-8. Disponível em: http://www.ismp-brasil.org/site/wp-content/uploads/2015/12/V4N3.pdf
20.Fermi MRV. Diálise para enfermagem. 2ª ed. Rio de Janeiro: Guanabara Koogan; 2010.
21.Manfredi SR, Nadaletto MAJ, Draibe AS, Canziani MEF. Técnicas dialíticas na doença renal crônica. In: Ajzen H, SChor N. Guias de medicina ambulatorial e hospitalar da UNIFESP-EPM. Nefrologia. 3ª ed. Barueri (SP): Manole; 2011. p. 449-59.
22.Grothe C, Belasco AGS, Bittencourt ARC, Vianna LAC, Sesso RCC, Barbosa DA. Incidence of bloodstream infection among patients on hemodialysis by central venous catheter. Rev Latino-Am Enfermagem. 2010 [cited in 2016 Feb 19]; 18(1):73-80. Available from: http://www.scielo.br/pdf/rlae/v18n1/12.pdf
23.Mendonça KM, Neves HCC, Barbosa DFS, Souza ACSe, Tipple AFV, Prado MA. Nursing care in the prevention and control of catheter – related bloodstream infections. Rev enferm UERJ. 2011 [cited in 2016 Feb 19]; 19(2):330-3. Available form: http://www.facenf.uerj.br/v19n2/v19n2a26.pdf
24.Paranaguá TT, Bezerra AL, Silva AE, Azevedo Filho FM. Prevalence of no harm incidents and adverse events in a surgical clinic. Acta Paul Enferm. 2013 [citaded in 2016 Feb 19]; 26(3):256-62. Available from: http://www.scielo.br/pdf/ape/v26n3/09.pdf
25.Flato UAP, Petisco GM, Santos FB. Ultrasound-guided venous cannulation in a critical care unit. Rev bras ter intensiva. 2009 [cited in 2016 Feb 19]; 21(2):190-6. Available from: http://www.scielo.br/pdf/rbti/v21n2/12.pdf
26.Ball LK. The buttonhole technique for arteriovenous fistula cannulation. Nephrol Nurs J 2006; 33:299-304.
27.Aranaz-Andrés JM, Aibar-Remón C, Limón-Ramírez R, Amarilla A, Restrepo FR, Urroz O, et al. Prevalence of adverse events in the hospitals of five Latin American countries: results of the Iberoamerican study of adverse events (IBEAS). BMJ Qual Saf. 2011; 20(12):1043-51.
28.Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2012 [cited in 2016 Feb 19]; 470(2):490-6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3254770/