ORIGINAL RESEARCH
Assessment of short-term central venous catheter dressing practices
Maria Laura Silva GomesI; Gabriel Angelo de Aquino II; Lívia Moreira BarrosIII; Patrícia Aquino de QueirozIV; Francisca Jane Gomes de OliveiraV; Joselany Áfio CaetanoVI
I
Student, Nursing degree, Universidade Federal do Ceará. Education
Scholar Tutorial. Fortaleza, Ceará, Brazil. E-mail: mlaura_gomes@hotmail.com
II
Student, Nursing degree, Universidade Federal do Ceará. Nursing
technician at the University Hospital. Fortaleza, Ceará, Brazil. E-mail:
gabrielangeloaqui@hotmail.com
III
Nurse. Doctoral candidate, Post graduate program in Nursing, Universidade
Federal do Ceará. Brazil. E-mail: livia.moreirab@hotmail.com
IV
Nurse. Intensive Clinic Care Unit Coordinator, University Hospital Walter
Cantídio. Fortaleza, Ceará, Brazil. E-mail: patriciaaqui@hotmail.com
V
Nurse, Master degree in Nursing. Monte Klinikum Hospital nurse. Fortaleza,
Ceará, Brazil. E-mail: jane3876@gmail.com
VI
Nurse, Doctor degree, Professor of undergraduate and Post graduate program
in Nursing at the Universidade Federal do Ceará, Brazil. E-mail: joselany@ufc.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.18196
ABSTRACT
Objective : to assess conformity with bloodstream infection prevention practices relating to dressing the short-term central venous catheter. Method: structured observational study of 30 nurses changing dressings on short-term central venous catheters in inpatients at a hospital in Fortaleza, Ceará, from 2014 to 2015. Data were collected using a check-list and subjected to descriptive statistical analysis. The results were displayed as absolute and relative frequencies. The study was approved by Opinion No. 488.788. Results: in 30 direct observations, 163 non-conformities were recorded, relating mostly to: presentation and explanation of the procedure to the patient, positioning of the head, hand hygiene after disposal, cleaning of the catheter connections, identification of the dressing and immediate completion of the nursing record. Conclusion: many nonconformities were found in performance of the procedure, evidencing the need to incorporate scientific evidence-based practice to minimize the risk of infections from dressing this device.
Keywords : Nursing, therapeutics, disease prevention; catheters.
INTRODUCTION
The use of central venous catheters (CVC) are essential for the health care of critically ill people1. They provide a consistent method to access the vascular system and infuse medications, fluids and electrolytes, blood and its derivatives, intravenous drugs, chemotherapy and parenteral nutrition for extended periods of time, and allow the application of diagnostic and therapeutic methods as hemodialysis, monitoring venous and arterial hemodynamic and contrast infusion to visualize the structures 2.
However, complications during its use may occur, especially: bloodstream infection (BSI), thrombosis, occlusion, dislocation, breakage and skin irritation1,2. It is estimated that 12% of all infections acquired in intensive care units (ICU) are related to the use of CVC and the average time in the hospital may be extended for more 10 to 20 days 3,4. However, when behavioral and technological interventions are put into practice, such as hands hygiene, training, use of personal protective equipment (PPE), use of checklists, skin preparation with chlorhexidine aqueous solutions and dressings impregnated with antiseptic or antibiotic, it is noticeable that such practices and devices prevent the development of infections and are in compliance with the CVC use1,4-6.
That conformity is associated with a structure of human and material resources and a process that encompasses actions so healthcare care is efficiently executed, according to what is stated in the technical standards, with satisfactory results7. With respect to the dressing, the nurse must have attention and care during the process, considering that the technique and the cover used influence the effective protection of the catheter insertion site and prevents micro-organisms colonization, as it is occluded.
Currently, there are different dressings available in the market and the use of simple gauze with tape and transparent polyurethane film are the most common8. However, there are still other practices that do not follow the main guidelines related to CVC dressing
In this context, the nursing professional's awareness for a health care based on scientific evidence and the proper follow-up of the guidelines on literature1-6 is still a challenge to be overcome. It is believed that identifying the main actions of non-compliance related to CVC dressing exchange can contribute to both reduce complications associated with the use of CVC, and improve the professionals' knowledge about the appropriate management of these devices.
In this perspective, this study aims to assess the prevention of bloodstream infection related to dressing practices in short-term central venous catheter.
LITERATURE REVIEW
The safe handling of the catheter should be a priority of the entire nursing staff assisting the patient, with technical rigor and surveillance, in order to prevent and control possible complications or adverse events. The presence of complications, such as BSI, thrombosis, occlusion, dislocation or breakage of a CVC, could result in the treatment interruption and insertion of a new device, in addition to increasing hospital costs and the morbidity and mortality of the patient2,9 .
Many of the complications related to CVC are considered preventable with the consistent application of strategies based on scientific evidence which causes a significant impact in reducing rates of BSI when following clinic guidelines8.
In addition, another important factor is that during CVC dressing the nurse should use personal protection equipment and carry out an aseptic technique, always paying attention to identify redness, swelling, or heat, patient's chills or tremors and the occurrence of secretions in the catheter insertion site which are characteristic signs of infection 2.
Thus, considering the complexity to implement and use this type of vascular access, it is imperative the technical standardization to prevent and control complications related to its use, that are, mostly, the nursing staff responsibility, to promote patients' and professionals' safety by providing quality health care9,10.
On the exposed, although vascular access practices have become a routine and apparently simple activity of nursing staff, it requires specific care and strict observation of preventive measures in order to avoid iatrogeny, ensure the quality of assistance as well as patients' and professionals' safety11.
When it comes to patient's safety, it is crucial to understand that human error can be linked to several factors, such as institutional, financial and structural issues. The occurrence of errors should be interpreted as faults arising from technical and organizational systems breakdowns related to health care, and not because of isolated actions of the profissionals 12.
Currently, one of the health organizations challenges is to evaluate the assistance provided through the implementation of quality indicators, which are screening tools that have the purpose of identifying potential areas of concern in health care, reflecting the quality of assistance in the hospitals. That way, the adoption of good practices handling CVC becomes a powerful tool to fight against the prevention of BSI, promoting a safe and quality service13.
METHODOLOGY
This is an observational and sectional study with a quantitative approach, held from June 2014 to January 2015, in a medium-sized teaching hospital, located in the municipality of Fortaleza-CE/Brazil, with 16 clinics and 242 inpatient beds. The study was carried out in the inpatient units of the hospital (medical clinic, surgical clinic and intensive care unit).
Compliance practices for dressing of CVC have been selected and established from the related manual in health care assistance to prevent infections 14, which has operational definitions for the indicators, as records of indication and permanence of the central vascular catheterization and short-term CVC insertion and maintenance aim at the prevention of bloodstream infections.
The manual presents variables to be observed as to the indication, installation, maintenance and permanence time of CVC and includes, mainly, direct observation of the short-term CVC insertion dressing exchange, which corresponds to devices that reach the central vessels (subclavian, jugular and femoral), installed by venipuncture, without tunneling and, in general, remain for a period of 10 to 14 days15.
Data collection and the records observation were carried out in the early hours. The inclusion criteria were established as follows: dressing practices performed in patients over 18 years old who had a short-term CVC for more than 24 hours. The excluded were dressings not performed by nurses and dressing practices not related to short-term CVC. The non-probabilistic sample was composed of 30 direct observations of different nurses, in which the selection was performed through spontaneous demand and there is no sample calculation. For data collection we used a check-list instrument, which was divided into three stages (variables): dressing preparation, dressing procedure and the unit organization; it contained items relating to the time of the CVC dressing exchange, advocated by the institution and to the personal protective equipment used by professionals in the procedure.
The observations were arranged in a database using the Excel program, and were summarized by means of percent absolute and relative frequency distributions. The results were presented through tables and discussed according to the relevant literature. To calculate conformity indexes of the practices we used the formula in which the numerator was the total number of short-term CVC with correct actions observed x 100 and, the denominator was the total number of assessed CVC.
The study followed the recommendations of resolution No. 466/12, being approved under paragraph of the opinion 488,788. All professionals knew about the purpose of the study and the need to observe the procedures directly, without a description of the activities to be observed, and before the data collection they were asked to sign the informed consent form.
RESULTS AND DISCUSSION
CVC treatment can be taken as a simple procedure and the concern to promote measures to reduce the infection associated with the device, is justified by the high rates of morbidity and mortality associated with it. A patient affected by this complication increases hospital costs in about $3,700 to $29,000 dollars and the mortality is of 18%6.
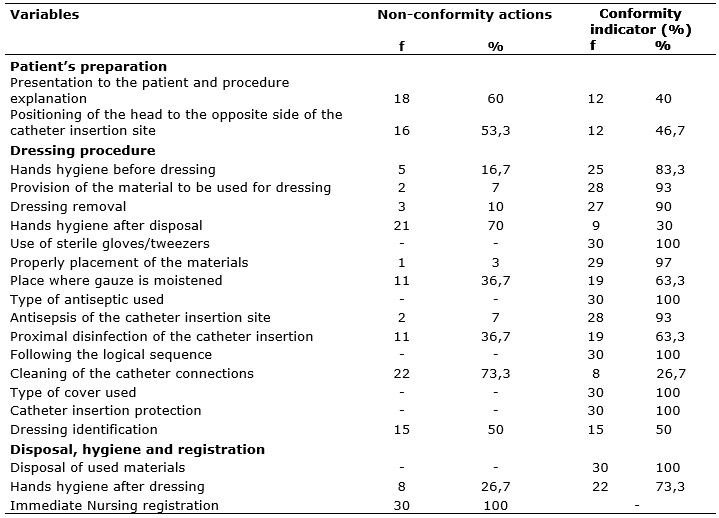
Among the variables of 30 observations in this study, a total of 443 (73%) conformities and 163 (27%) non-conformities were obtained. It was found that nurses used individual protection equipment: mask, gloves, hat and apron to perform the dressings. As for the type of antiseptic and dressing cover used, 30 (100%) opted for 0.5% alcoholic chlorhexidine, 27 (90%) used the sterile gauze to cover and 3 (10%) the transparent film, 19 (63%) carried out the proximal disinfection of the catheter insertion, 25 (83.3%) carried out hands hygiene before the dressing and 22 (73.3%) after the procedure; The clothes used during the dressing were in accordance with the guidelines recommended by the evidence-based practices. The non-conformity actions identified and the corresponding indicators of compliance, are showed in Table 1.
TABLE 1:
Distribution of variables related to the dressing practice of short-term
central venous catheter. Fortaleza, CE, Brazil, 2015.( N= 30)
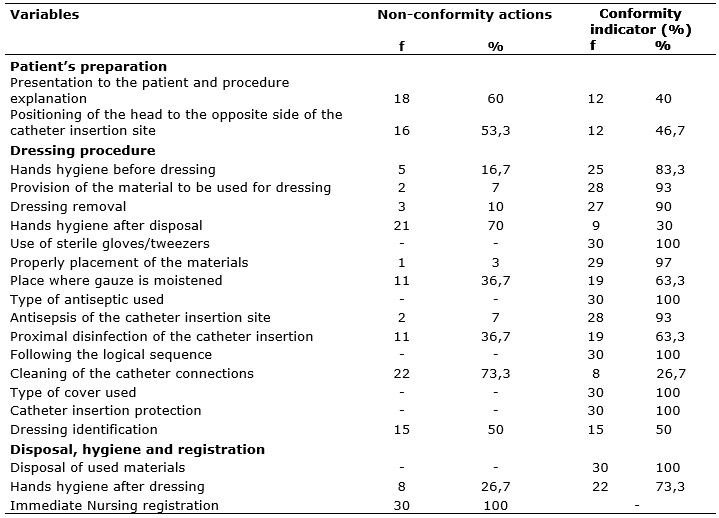
This study identified some failures in the communication with the patient and shows that most professionals promoted the preparation explaining the procedure, as shown in Table 1. Besides, the patient preparation represents an important moment for the humanization of health care, considering that the explanation of what will be done can reduce anxiety, fear and insecurity, as well as enables the clarification of doubts and increases the patient's knowledge on the need of CVC16.
About the dressing procedure, the main actions of non-compliances were related to hands hygiene after the disposal; the place where gauze is moistened (inside the dressing tray); proximal disinfection of catheter insertion; cleaning of the catheter connections and dressing identification. About disposal, hands hygiene after the disposal and registration presented low compliance indicators as none of the professionals realize nursing registration immediately after the dressing exchange, according to Table 1. Continuous monitoring and registration of complications are the most crucial factors for health care quality control and improvement3.
Nursing registration is the main form of communication among professionals about the health care provided to the patient, and it is necessary to make the notes soon after the procedure. However, due to factors such as overload of activities, excess hours of working, lack of interest or because they simply forget, the professionals do not register their services, and, in this way, they harm the health care plan due to lack of informtion17.
Another highlight action of non-compliance was the failure on the proximal disinfection of the catheter insertion. Cannulation area should be disinfected with a full application of alcoholic chlorhexidine and the professional should wait the solution to evaporate before handling the CVC 4. In addition, the care with the catheter asepsis should be a priority, also during the dressing replacement, and must be performed by a properly trained and qualified professional12.
The guidelines recommend the use of semi-permeable, sterile and transparent (for example, in polyurethane) dressings as they allow to see the ostium of the catheter insertion and they also point out the importance of changing the dressing. Simple gauze with tape can also be used, especially in the case of patients with active bleeding or that sweat where the catheter is placedt12.
On the other hand, the use of semi-permeable polyurethane dressings (transparent), despite increasing the incidence of colonization, is not consistently associated with the increased incidence of catheter-related infections. Their advantage compared with gauze dressing it is the possibility to observe the catheter insertion site, which facilitates the early preview of local signals of infection8.
Daily maintenance, regular disinfection, CVC coupling changes and following the basic hygiene measures are the most important interventions to prevent complications related to the use of the CVC. Such interventions should include the daily evaluation of individual requirements of a central venous catheter in hospitalized patients using the device3.
It is important to note that hands hygiene after disposing the material used in the dressing also presented low compliance. A total of 17 hand hygiene with alcohol-gel and 41 with soap and water were observed, which made it possible to infer the existence of gaps about the professional's behavior on hand hygiene after removing the primary wound dressing, as showed in the Table 2.
TABLE 2:
Distribution of variables related to hand hygiene during dressing practices
of short-term central venous catheter. Fortaleza, CE, Brasil, 2015.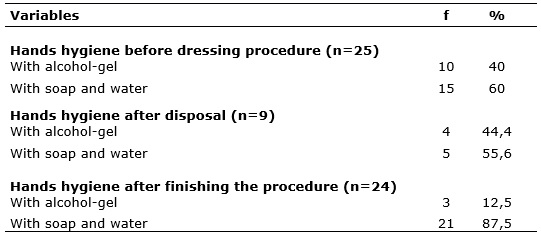
Hands hygiene is, isolated, the most important action to prevent and control hospital infections18,19. This can be done with soap and water or with alcohol-gel, and should occur before and after contact with the patient, before putting on the gloves and after removing them, between a patient and another, between a procedure and another, or on occasions in which pathogens may be transfer to the patient and/or environments, between procedures with the same patient, after contact with blood, body fluid, secretions, excretions and contaminated articles or equipment11.
An observational study, carried out to evaluate the adherence to the hands hygiene practices related to vascular access in an ICU, in which 25 nursing professionals participated, five nurses and 20 nurse technicians, showed that most of the professionals never carried out hands hygiene, with high rates of non-compliance relating to the following practices: changing the infusion system, drug delivery and central venous catheter dressing exchange20.
Another research, conducted in the ICU, aimed to evaluate the technical compliance of handwashing in invasive and non-invasive procedures. It was found that only 50% of health professionals performed hands hygiene before invasive procedures, and 44% during invasive procedures21.
Several are the factors, mentioned by health professionals, that interfere in decision-making about following or not HH practice: because they forget or they ignore its importance, the sink is distant, skin irritation, they do not have enough time and lack of materials19.
In a study conducted at eight American hospitals, the findings showed discouraging performance in the amount of compliance carrying out the practice of hand hygiene by the health professionals22. There are other researches that point to the use of technologies and electronic and video systems to monitor hand hygiene to improve its practice and reduce the incidence of hospital infections. However, there is still no evidence that this may impact positively23.
The change in the behavior of health professionals is a major challenge for government agencies, institutions, managers and workers, since it is imperative to adhere to the recommendations and protocols directed to improve health care practices, above all, the hand hygiene that contributes to patient's and professional's safety.
CONCLUSION
This study made it possible to identify the non-conformities related to short-term CVC dressing exchange practices, in which the most important focused on the presentation and explanation of the procedure, the patient position with the head to the opposite side of the catheter insertion place, hands hygiene after the disposal, catheter connections cleaning, dressing identification and immediately nursing registration.
It is expected that the results may contribute to the development of actions aimed at enhancing the practice, such as the creation of educational programs that combine theory to practice, to change the reality. It is crucial that the theoretical and practical contents are accessible and disseminated to other sectors that assist critically ill patients. It is important to note that the BSI causes damage both to the patient and to the institution, being the responsibility of the health care team to guarantee quality care, according to what is stated in the hospital guidelines.
It is necessary to develop actions to improve health care practices, in addition to the educational strategies such as health care continuous assessment aiming at reducing BSI related to the use of CVC, which will lead to an effective assistance, free of adverse events. This article presents some limitations such as: only one direct observation of each nurse was performed, and the researcher was observing the performance. It is recommended, in another study, to increase the number of direct observations and perform the observations with video recordings to eliminate the presence of the researcher interference in the behavior of the professional during the procedure.
REFERENCES
1.Walz JM, Ellison RT, Mack DA, Flaherty HM, McIlwaine JK, Whyte KG, et al. The Bundle plus: the effect of a multidisciplinary team approach to eradicate central line-associated bloodstream infections. Anesth Analg. 2015;20(4):868-76.
2.Ullman AJ, Cooke M, Rickard CM. Examining the role of securement and dressing products to prevent central venous access device failure: a narrative review. JAVA. 2015;20(2):99-110.
3. Lindgren S , Pikwer A , Ricksten SE , Åkeson J . Survey of central venous catheterisation practice in Sweden. Acta Anaesthesiol Scand. 2013;57(10):1237-44.
4. Frykholm P , Pikwer A , Hammarskjöld F , Larsson AT , Lindgren S , Lindwall R , et al. Clinical guidelines on central venous catheterisation. Swedish Society of Anesthesiology and Intensive Care Medicine. Acta Anaesthesiol Scand. 2014;58(5):508-24.
5.Osorio J, Álvarez D, Pacheco R, Gómez CA, Lozano A. Implementation of an insertion bundle for preventing central line-associated bloodstream infections in an intensive care unit in Colombia. Rev Chil Infectol. 2013;30(5):465-73.
6.Pedrolo E, Danski MTR, Vayego SA. Chlorhexidine and gauze and tape dressing for central venous catheter: randomized clinical trial. Latino-Am Enfermagem Magazine. 2014;22(5):764-71.
7.Vuori H. The quality of health. Saúde Debate. 1991;3:17-25.
8.Pedrolo E, Danski MTR, Mingorance P, De Lazzari LSM, Johann DA. Clinical controlled trial on central venous catheter dressings. Acta Paul Enferm. 2011;24(2):278-83.
9.Hebbar KB, Cunningham C, McCracken C, Kamat P, Fortenberry JD. Simulation-based pediatric intensive care unit central venous line maintenance bundle training. Intensive Crit Care Nurs. 2015;31(1):44-50.
10.Guimarães GL, Goveia VR, Mendonza IYQ, Corrêa AR, Matos SS, Guimarães JO. Nursing interventions in the patient in hemodialysis by central venous catheter. Rev enferm UFPE on line. 2017;11(3):1127-35.
11.Mendonça KM, Neves HCC, Barbosa DFS, Souza ACS, Tipple AFV, Prado MA. Nursing work in prevention and control of catheter related bloodstream infection. Rev enferm UERJ. 2011;19(2):330-3.
12.Pena MM, Braga AT, Meireles ES, Vassao LGC, Melleiro MM. Mapping of medication errors in a university hospital. Rev enferm UERJ. 2016;24(3):7095.
13.Lima CSP, Barbosa SFF. Occurrence of adverse events as indicators of quality care in intensive care unit. Rev enferm UERJ. 2015;23(2):222-8.
14.Ministry of Health (Br). Series patient safety and quality in health services. Manual of infection prevention measures related to health care. Brasília (DF) Editora MS; 2010.
15. The national health surveillance agency (Br). Guidelines for prevention of primary bloodstream infection. Brasília(DF): ANVISA; 2010.
16.Figueiredo SV, Gomes ILV, Pennafort VPS, Monteiro ARM, Figueiredo JV. Therapeutic communication between health professionals and mothers accompanying their child during the hospitalization. Esc Anna Nery. 2013; 17(4):690-97.
17.Figueiredo RM, Maroldi MAC. Home hospitalization: risk of exposure to biological health team. Rev esc enferm USP. 2012;46(1):145-50.
18.Cardoso ACM, Figueiredo RM. Biohazard situations present in nursing care in the family health units (USF). Rev Latino-Am Enfermagem. 2010;18(3).
19.Santos TCR, Roseira CE, Piai-Morais TH, Figueiredo RM. (2014). Hand hygiene in hospitals: use of compliance indicators. Rev Gaúcha Enferm. 2014; 35(1):70-7.
20.Oliveira FJG, Meneses LET, Silva VM, Oliveira MLB, Machado JJA. Evaluation of hand hygiene practices related to placement of intravascular lines in an intensive care unit. Rev vigil sanit debate. 2015;3(4):55-61.
21.Locks L, Lacerda Jt, Gomes E, Serratine ACP. Hands hygiene quality of working professionals in basic health units. Rev Gaúcha de Enferm. 2011;32(3):569-75.
22.Chassin MR, Mayer C, Nether K. Improving hand hygiene at eight hospitals in the United States by targeting specific causes of noncompliance. J Qual Paciente Saf. 2015;41(1):4-12.
23.Srigley JA, Gardam M, Fernie G, Lightfoot D, Lebovic G, Muller MP. Hand hygiene monitoring technology: a systematic review of efficacy. J Hosp Infect. 2015;89 (1):51-60.