( *) Chi-square test (†) Fisher's exact test
ORIGINAL RESEARCH
Prevalence and epidemiological aspects of HIV/tuberculosis coinfection
Carolina de Castro CastrighiniI; Renata Karina Reis II; Lis Aparecida de Souza NevesIII; Marli Teresinha Gimeniz GalvãoIV; Elucir GirV
I
Nurse. PhD student in the Graduate Studies Program in Basic Nursing,
University of São Paulo. Ribeirão Preto, São Paulo, Brazil. Email: carolcastrousp@hotmail.com
II
Nurse. Professor (PhD) in the Department of General and Specialized
Nursing, University of São Paulo. Ribeirão Preto, São Paulo, Brazil. Email: rkreis@eerp.usp.br
III
Nurse. PhD in Sciences. Coordinator of the Municipal STD/AIDS and
Tuberculosis Program, Ribeirão Preto, São Paulo, Brazil. Email: lisapneves@yahoo.com.br
IV
Nurse. Professor (PhD) at the Federal University of Ceará. Fortaleza,
Ceará, Brazil. Email: marligalvao@gmail.com
V
Nurse. Full Professor (PhD) in the Department of General and Specialized
Nursing, University of São Paulo. Ribeirão Preto, São Paulo, Brazil. Email: egir@eerp.usp.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.17432
ABSTRACT
Objective: to evaluate the prevalence and epidemiological aspects of human immunodeficiency virus (HIV)/tuberculosis coinfection in the municipality of Ribeirão Preto, São Paulo. Method: retrospective study involving all cases of HIV-tuberculosis coinfected residents in the municipality, notified in the São Paulo State Tuberculosis Information System (TBweb) between 2003 and 2011. Data were obtained from the TBweb and its linkages with HIV information systems. The study population consisted of 338 coinfected. Chi-square and Fisher's exact test were performed. The study was approved by the research ethics committee (protocol CAAE 02789012.4.0000.5393). Results: of the 1,277 cases of tuberculosis registered in the TBweb, 338 presented coinfection with HIV, a prevalence of 26.5%; of these, 244 (72.2%) were men. The predominant clinical form of the disease was pulmonary TB (201 cases; 59.5%). Conclusion: the prevalence of coinfected individuals was 26.5%, of whom most were men. These data point to the need for interventions to prevent both diseases.
Keywords: Prevalence; HIV; tuberculosis; epidemiology.
INTRODUCTION
According to the World Health Organization (WHO), the risk of people with the human immunodeficiency virus (HIV) developing tuberculosis is much higher than among uninfected individuals1. According to the WHO, there were around 36.7 million people worldwide living with HIV in 2016 1. In Brazil, the first case of the acquired immunodeficiency syndrome (AIDS) was reported in 1982 in the city of São Paulo; since then and up to June 2016, the total number of reported cases was 842,710 2.
With respect to tuberculosis, it is estimated that one-third of the world's population is infected with M. tuberculosis, with approximately 10.4 million new cases per year3. Among the 22 countries responsible for 80% of the total cases of tuberculosis in the world, Brazil ranks in the twentieth position4.
In 2015, of the 10.4 million new cases of tuberculosis in the world, 11%
(approximately 1.2 million) had HIV/TB coinfection3. In Brazil,
tuberculosis is the leading cause of death among AIDS cases5.
Given the relevance of HIV/TB coinfection and how one disease affects the evolution of the other, the identification of this prevalence is an important indicator for programs to prevent and control these diseases, implement health programs and assess strategies.
The objective of this study was to evaluate the prevalence and epidemiological aspects of HIV/TB coinfection in the city of Ribeirão Preto, in the state of São Paulo.
LITERATURE REVIEW
The introduction of the antiretroviral therapy (ART) associated with knowledge of the disease, monitoring of infection through counts of clusters of differentiation 4 with T lymphocytes (TCD4 +) and viral load, resulted in the chronicity of the disease6,7. Since 1996, the Brazilian Ministry of Health has guaranteed universal treatment for all people living with HIV/AIDS, in order to reduce the morbidity and mortality associated with HIV, improve quality of life, preserve and, if possible, restore these people's immune system, and suppress viral replication 7.
As the HIV infection progresses and immunity declines, individuals become more susceptible to infections. The opportunistic infections that stand out are toxoplasmosis of the central nervous system, Pneumocystis jiroveci pneumonia, atypical or disseminated pulmonary tuberculosis, cryptococcal meningitis, and cytomegalovirus retinitis8.
Tuberculosis is one of the most ancient diseases of humanity. It is caused by Mycobacterium tuberculosis, also known as Koch's Bacillus, and is the most common opportunistic infection associated with AIDS9.
METHODOLOGY
This analytical, retrospective study was based on secondary data and conducted in the city of Ribeirão Preto-SP.
The city had an estimated population of 674,405 inhabitants in 2016 10 and its health network is organized into five Health Districts - North, South, East, West, and Central. Each one has a specialized outpatient clinic to care for people with HIV/AIDS, sexually transmitted infections, and tuberculosis, namely: José Roberto Campi Reference Center, Alexander Fleming Reference Center, Reference Center for Central Specialties, Castelo Branco Basic and District Health Unit, and Sumarezinho Basic and District Health Unit, in addition to the Infectious Disease Special Treatment Unit and the Hospital das Clínicas of Ribeirão Preto11.
For data collection, cases registered from December 2012 to April 2013 were first identified. The study population was made up of 338 individuals with HIV/TB coinfection living in the city of Ribeirão Preto, who had reported the disease and been registered in the TBweb program from 2003 to 2011, and met the following inclusion criteria: having HIV/TB coinfection; having been diagnosed with tuberculosis and reported the disease in the period from 2003 to 2011, living in Ribeirão Preto, being 18 years of age or older, and not being in a situation of confinement. The exclusion criterion was defined as only having tuberculosis.
The information was collected in 2012 from a database resulting from the linkage between the Tuberculosis Information System of the state of São Paulo (TBweb) and the Information System for Notifiable Diseases (SINAN), Control System for Laboratory Tests (SISCEL) and Logistical Control System for Medications (SICLOM) which contains information about HIV/AIDS.
Of the total 1,756 notifications registered in the TBweb system from 2003 to 2011, researchers excluded 939 cases of tuberculosis monoinfection, 110 relapses, 58 retreatments, 65 duplicate records and 246 for other reasons, such as being under 18 years old or being in confinement, resulting in a total study population of 338 individuals.
The variables of interest in the present study were: sex, age, race/color, education, type of case, clinical form, clinical classification, tests performed (acid-fast bacilli smear, sputum culture and X-rays), HIV testing, outcome, and type of tuberculosis treatment.
The linkage technique entails the unification of two or more databases 12. This technique was adopted to enable crossing tuberculosis databases with HIV/AIDS databases. The procedure for comparing the data and the manual revision were performed by RecLink III software. The criterion of confirmation of pairs was based on the fields: patient's name, mother's name, date of birth, address, and city of residence.
The data were analyzed using the program Statistical Package for the Social Sciences (SPSS), Version 17.0 for Windows. Descriptive statistics through frequencies were used for all the variables. Afterwards, the chi-square test and Fisher's exact test were performed to check for statistically significant differences. A significance level of 5% was used for all the tests performed.
Ethical aspects were considered and the research project was approved by the Research Ethics Committee of the Ribeirão Preto College of Nursing at the University of São Paulo, Opinion No. 135/201, CAAE Protocol 02789012.4.0000.5393, in accordance with the recommendations from Resolution No. 466/12 of the National Health Council. Authorizations were obtained for use of the databases.
RESULTS AND DISCUSSION
The prevalence of HIV/TB coinfection was 26.5%, i.e., of the 1,277 individuals with tuberculosis, 338 were coinfected.
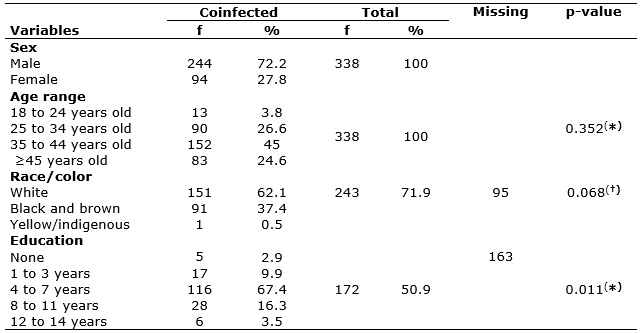
In relation to demographic characteristics, 244 (72.2%) were men and 94 (27.8%) were women, with a predominant age range of 35 to 44 years old (45%). In terms of race/color, 151 (62.1%) were white and 116 (67.4%) had 4 to 7 years of education; for both variables there was a high index of people who did not fill in this information, as shown in Table 1.
TABLE 1:
Distribution of cases of HIV/TB coinfection and demographic variables.
Ribeirão Preto, São Paulo, 2003-2011. (n=338).
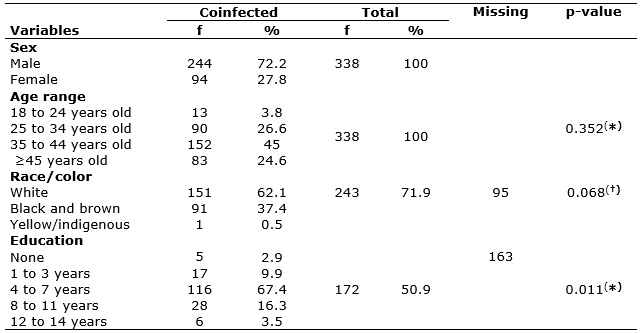
(
*) Chi-square test (†) Fisher's exact test
In reference to the type of case, new cases were identified in 222 (91%) men and in 86 (91.5%) women (p=1.000). Being cured was the most common outcome for both men (149 cases; 61.3%) and women (50 cases; 53.2%), followed by death with 74 (30.3%) in men and 37 (39.4%) in women. In relation to clinical form, pulmonary was found the most in both sexes, but extrapulmonary was also high in men (71 cases; 29.1%) and women (30 cases; 31.9%) (p= 0.691). With respect to tests that helped confirm the diagnosis, negative acid-fast bacilli smear was the most common in both sexes (p=0.464). As far as chest X-rays, in 137 (71%) of the men and 55 (72.4%) of the women, the image suggested tuberculosis (p=0.762). A sputum culture was done on 161 individuals, with positive results in 56 (48.3%) men and 18 (40%) women (p=0.624). There were 191 (56.5%) (p=0.910) supervised treatments given, according to Table 2.
TABLE 2:
Distribution of cases of HIV/tuberculosis coinfection by sex according to
clinical variables. Ribeirão Preto, São Paulo, 2003-2011. (n=338)
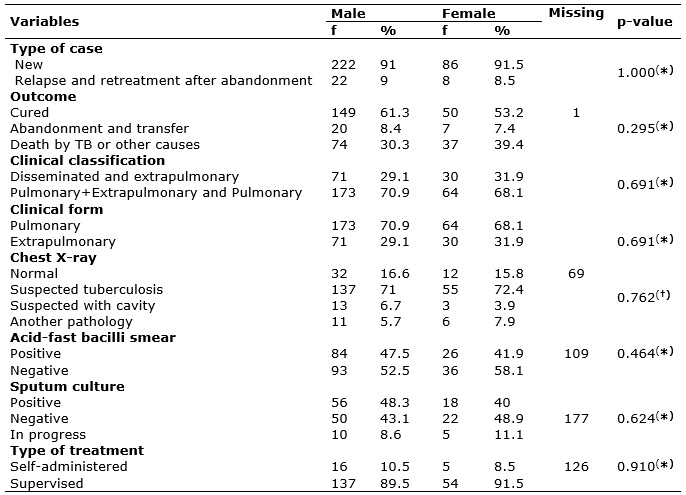
(*) Chi-square test (†) Fisher's
exact test
The prevalence of HIV/TB coinfection was 26.5%, which coincides with other findings in the national13,14 and international15 literature.
The demographic characteristics of the participants were similar to other studies in terms of predominance of men16-20. The reasons for greater sickness among tuberculosis cases in men may possibly be due to their behavioral tendencies, such as higher exposure to disease or greater difficulty in adherence to treatment21.
The predominant age range was 35 to 44 years old, corresponding to a productive age range. Other studies, however, presented different findings in relation to the same population22-24. Contracting the disease during the productive age range can have an impact on the personal and professional lives of these individuals, as well as bear social consequences for the person, family members and society22.
The predominant race/color was white, but in 28.1% of the total number of cases it was not possible to identify this variable, since this information was not included in the TBweb and SINAN information systems. In other studies, white was also the predominant color22,23. The race/color classification is very subjective, and in a study that uses secondary data, it cannot be confirmed that the race individuals assign to themselves is correct, but it is a result that helps characterize this population.
The degree of immunosuppression may be a factor in the clinical presentation of tuberculosis in coinfected individuals21. In the present study, the pulmonary form was found the most, followed by the extrapulmonary form. These findings match those in other studies which show that the pulmonary form is the most prevalent25-27, but the extrapulmonary form has also constantly appeared in individuals with HIV/tuberculosis22,25,26.
The new case type was the most prevalent. Other studies also found a high rate of identification of new cases18,28, although the present study opted to use the first tuberculosis treatment in the study period in order to characterize it in relation to HIV.
As for relapse cases, the rate was 8.9% in the studied population. Cases reported as relapses indicate that the individual had already been treated previously and contracted tuberculosis again. This shows that immune deficiency in individuals with coinfection often requires follow-up even after the person is cured at the end of the treatment. This finding demonstrates the need for initiatives that focus more on individuals with HIV/tuberculosis in terms of treatment, since they had already received treatment and were infected again.
In relation to outcome, most of the individuals were cured. This result coincides with findings of other studies22,26,29. The abandonment rate was 8% of the cases. The difficulties patients had in adhering to the treatment may have been related to the adverse effects of the drugs, alcoholism, drug addiction, failure to bond with health professionals, and refusal to accept supervised treatment30.
In these individuals, diagnosis becomes more difficult due to the ability of clinical aspects to be modified, atypical X-rays, low acid-fast bacilli smear sensitivity24,30, negative sputum culture, and higher rates of extrapulmonary tuberculosis31.
In the population studied it was noted that 56.5% of coinfected cases received supervised treatment, a finding that coincides with another study performed with the same population18.
The directly observed treatment, short-course (DOTS) strategy proposed by the World Health Organization in 1993 is comprised of the following components: detection of cases by acid-fast bacilli smear, standardized treatment with support for patients, supply of medication, monitoring of the evolution of the system, and political commitment to tuberculosis control32. The strategy focuses on prevention, adherence to treatment33,34, and reduction of abandonment rates35.
Among the tests conducted to diagnose tuberculosis, the most prevalent was chest X-rays, where 71.4% of the cases had images suggesting tuberculosis. However, all the other tests were also performed, since they are extremely important for diagnosing HIV/TB coinfection.
There was a high prevalence of negative acid-fast bacilli smear and sputum culture results.
CONCLUSION
The prevalence of HIV/TB coinfection was 26.5% of the individuals with tuberculosis.
HIV/TB coinfection is also a very important factor in public health, due to the implications of both of these pathologies and the more severe harm it causes to the population afflicted with the two diseases.
There must be a very close relationship between HIV and tuberculosis prevention policies, aimed at early diagnosis of HIV through testing and counseling, in addition to actively searching for symptoms of tuberculosis and providing such testing for individuals with HIV/AIDS.
The analysis of the profile of individuals with HIV/tuberculosis showed that it is still very prevalent in Ribeirão Preto, higher than in other cities in Brazil.
A limitation of the study was related to the use of information from databases, since there were errors in the filling out of information, which affected the analysis of the profile of the population studied.
The results of this study helped delineate the profile of this population over the course of a decade and indicated the need for more actions aimed at prevention of both diseases and the importance of closer interaction between the HIV/AIDS and tuberculosis programs.
It is suggested to provide training and raise awareness among professionals who care for this population, through the presentation of epidemiological data, together with prevention strategies, such as HIV testing in individuals with tuberculosis, in order to provide a level of care that can help lower this prevalence.
REFERENCES
1. World Health Organization. Global Health Observatory. [cited on Aug 16, 2016]. Available from: http://www.who.int/hiv/data/en .
2. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Boletim epidemiológico: AIDS DST. Brasil. Ministério da Saúde; 2017. [citado em ago 16, 2016]. Disponível em: http://portalarquivos.saude.gov.br/images/pdf/2017/marco/23/2017-V-48-N-8-Indicadores-priorit--rios-para-o-monitoramento-do-Plano-Nacional-pelo-Fim-da-Tuberculose-como-Problema-de-Sa--de-P--blica-no-Brasil.pdf .
3. World Health Organization [website]. World Health Organization 2016. Global Tuberculosis Report 2016. [cited on Aug 16, 2016]. Available from: http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1 .
4. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Tuberculose. [citado em ago 16, 2016]. Disponível em: http://portalsaude.saude.gov.br/index.php/o-ministerio/principal/secretarias/svs/tuberculose
5. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Boletim
epidemiológico: AIDS DST. Brasília (DF): Ministério da Saúde; 2012.
6. Alencar TMD, Nemes MIB, Velloso MA. From "acute AIDS" to "chronic AIDS": body perception and surgical interventions in people living with HIV and AIDS. Ciênc saúde coletiva. 2008; 13(6):1841-9.
7. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Recomendações para Terapia Anti-retroviral em Adultos Infectados pelo HIV. Brasília (DF): Ministério da Saúde; 2008.
8. Ministério da Saúde (Br). Secretaria de Atenção à Saúde, Protocolo clínico e diretrizes terapêuticas para manejo da infecção pelo HIV em adultos. Brasília (DF): Ministério da Saúde; 2013.
9. Rodrigues Júnior AL, Ruffino-Neto A, Castilho EA. Spatial distribution of M. tuberculosis/HIV coinfection in São Paulo State, Brazil, 1991-2001Distribuição espacial da coinfecção M. tuberculosis/HIV no Estado de São Paulo, 1991-2001. Rev Saude Publica. 2006; 40(2):265-70.
10. Instituto Brasileiro de Geografia e Estatística. [website]. 2016. [ciatdo em ago 16, 2016]. Disponível em: http://www.ibge.gov.br/cidadesat/xtras/perfil.php?r=2&codmun=354340 .
11. Ribeirão Preto(SP). Aconselhamento em DST, HIV e aids e Hepatites Virais. [citado em Jan 30, 2016]. Disponível em: http://www.ribeiraopreto.sp.gov.br/ssaude/programas/aids/i16aconselha.php .
12. Almeida MmF, Jorge MHPm. The use of the 'Linkage' of information systems in cohort studies of neonatal mortality. Rev Saude Publica. 1996; 30(2):141-7.
13. Brunello MAF, Chiaravalloti Neto F, Arcêncio RA, Andrade RLP, Magnabosco GT, Villa TCS. Areas of vulnerability to HIV/TB co-infection in Southeastern Brazil. Rev Saude Publica. 2011; 45(3):556-63.
14. Rodrigues MAS, Scatena LM, Vendramini SHF, Canini SRMS, Villa TCS, Gir E. Avaliação do acesso ao tratamento de tuberculose por coinfectados ou não pelo Vírus da Imunodeficiência Humana. Rev esc enferm USP. 2012; 46(5):1163-9.
15. Andrade FEM, Londoño CA, Acevedo CS, Echeverri AQ, Montaño CEB, Navas MAM, et al. Caracteristicas clínicas, factores de riesgo y perfil de susceptibilidad de las infecciones por micobacterias documentadas por cultivo, em um hospital universitário de lata complejidad em Medellín (Colombia). Rev chil Infectol. 2014; 31(6):735-42.
16. Coelho AB, Biberg CA. Perfil epidemiológico da coinfecção Tuberculose/HIV no munícipio de São Luís, Maranhão, Brasil. Cadernos ESP, Ceará. 2015; 9(1):19-26.
17. Lemos LA, Fiuza MLT, Reis RK, Ferrer AC, Gir E, Galvão MTG. Adherence to antiretrovirals in people coinfected with the human immunodeficiency virus and tuberculosis. e2691. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692016000100324&lng=pt . Epub 17-Maio-2016. http://dx.doi.org/10.1590/1518-8345.0537.2691 .
18. Santos Neto M, Sailva FL, Sousa KR, Yamamura M, Popolin MP, Arcêncio RA. Perfil clínico e epidemiológico e prevalência da coinfecção tuberculose/HIV em uma regional de saúde no Maranhão. J Bras Pneumol. 2012; 38(6):724-32.
19. Molaeipoor L, Poorolajal J, Mohraz M, Esmailnasab N. Predictors of tuberculosis and human immunodeficiency virus co-infection: a case-control study. Epidemiol Health. 2014; 36(1):1-6.
20. Babamahmoodi F, Alikhani A, Charati JY, Ghovvati A, Ahangarkani F, Delavarian L, et al. Clinical epidemiology and paraclinical findings in tuberculosis patients in north of Iran. Biomed Res Int. 2015; 2015(1):1-5.
21. Pereira EP. Análise epidemiológica da tuberculose em indivíduos com HIV/aids em Goiás. [Master's dissertation]. Goiânia (GO): Federal University of Goiás; 2012.
22. Cheade MFM, Ivo ML, Siqueira PHGS, Sá RG, Honer MR. Caracterização da tuberculose em portadores de HIV/aids em um serviço de referência de Mato Grosso do Sul. Rev Soc Bras Med Trop. 2009; 42(2):119-25.
23. Prado TN, Miranda AE, Souza FM, Dias ES, Sousa LKF, Arakaki-Sanchez D. Factors associated with tuberculosis by HIV status in the Brazilian national surveillance system: a cross sectional study. BMC Infectious Diseases. 2014; 14(1):415-22.
24. Magno ES, Saraceni V, Souza AB, Magno RS, Saraiva MGG, Buhrer-Sékula S. Factors associated with TB/HIV coinfection: evidence from notification data in the State of Amazonas, Brazil, 2001-2012.Cad Saúde Pública. [Scielo-Scientific Eletronic Library Online] 2016 [cited on Aug 17, 2016]; 33(5):e00019315. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2017000505006&lng=en. Epub June 12, 2016. http://dx.doi.org/10.1590/0102-311x00019315 .
25. Neves LAS, Canini SRM, Reis RK, Santos CB, Gir E. Aids and tuberculosis: coinfection from the perspective of the quality of life of patients. 2012. 46(3):704-10.
26. Barbosa IR, Costa ICC. Estudo epidemiológico da coinfecção tuberculose-HIV no nordeste do Brasil. Rev Patol Trop Vol. 2014; 43(1):27-38.
27. Agbor AA, Bigna JJ, Plottel CS, Billong SC, Tejiojem MC, Ekali GL, et al. Characteristics of patients co-infected with HIV at the time of inpatient tuberculosis treatment initiation in Yaoundé, Cameroon: a tertiary care hospital-based cross-sectional study. Arch Public Health. 2015; 73(1):1-10.
28. Pinto Neto LFS, Vieira NFS, Cott FS, Oliveira FMA. Prevalência da tuberculose em pacientes infectados pelo vírus da imunodeficiência humana. Rev Bras Clin Med. 2013; 11(2):118-22.
29. Gaspar RS, Nunes N, Nunes M, Rodrigues VP. Temporal analysis of reported cases of tuberculosis and of tuberculosis-HIV co-infection in Brazil between 2002 and 2012. J Bras Pneumol. 2016; 42(6):416-22.
30. Santos MLSG, Ponce MAZ, Vendramini SHF, Villa TCS, Santos NSGM, et al. The epidemiological dimension of TB/HIV co-infection. Rev Latino-Am Enfermagem. 2009; 14(5):683-8.
31. Santos JS, Beck ST. A coinfecção tuberculose e HIV: um importante desafio – Artigo de revisão. Rev Bras Anal Clin. 2009; 41(3):209-15.
32. World Health Organization. Monitoring and valuation system, and impact measurement 2013. [cited on Nov 20, 2016]. Available from: http://www.who.int/tb/dots/monitoring_evaluation/en/index.html .
33. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Manual de recomendações para o controle da tuberculose no Brasil. Brasília (DF): Ministério da Saúde; 2011.
34. Souza KMJ, Sá LD, Assolini FEP, Queiroga RPF, Surniche CA, Palha PF. Discourses on tuberculosis: stigma ande consequences for the subject ill. Rev enferm UERJ. 2015; 23(4):475-80.
35. Cecilio HPM, Marcon SS. Health personnel's views of directly observed treatment of tuberculosis. Rev enferm UERJ. 2016; 24(1):1-6.