Result expressed in mean and ± sd(*)
ORIGINAL RESEARCH
Profile and factors associated with successful treatment of smokers in a specialized public service
Sandro Rogério dos SantosI; Ana Rita de Cassia BitencourtII; Rosana HuppesEngelIII; Maria Helena de Castro SilvaIV; Thais Santos Guerra StacciariniV; AldenoraLaísa Paiva de Carvalho CordeiroVI
I
Nurse. Graduated in Nursing. Pulmonary Function Nurse at the Federal
University of Triângulo Mineiro. Uberaba, Minas Gerais, Brazil. Email: sanroger21@gmail.com
II
Nurse. PhD in Pneumological Sciences. Professor, Federal University of São
Paulo. Brazil. E-mail: arcbettencourt@unifesp.br
III
Nurse. Graduated in Nursing. Nurse, Federal University of Triângulo
Mineiro. Uberaba, Minas Gerais, Brazil. E-mail: manaengel@gmail.com
IV
Physician. PhD in Pathology. Professor at the Federal University of
Triângulo Mineiro. Uberaba, Minas Gerais, Brazil. E-mail: mariahcs@terra.com.br
V
Nurse. PhD in Nursing. Nurse at the Federal University of Triângulo
Mineiro. Uberaba, Minas Gerais, Brazil. E-mail:
thais.stacciarini@terra.com.br
VI
Nurse. MS in Health Care. Nurse at the Federal University of Triângulo
Mineiro. Uberaba, Minas Gerais, Brazil. E-mail: alaisapc@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2018.17381
ABSTRACT
Objectives: to profile smokers enrolled in the smoking cessation program of the Triangulo Mineiro Federal University (UFTM) in Uberaba, Minas Gerais, and to list the factors associated with successful treatment. Method: this retrospective study conducted between February 2009 and December 2013 was approved by the UFTM research ethics committee (Protocol 2272). The medical records of 305 smokers were analyzed using a specifically constructed data collection instrument. Results: the service had no free medication for treatment and only 47 (15.4%) of the smokers were successfully treated. Multiple binomial logistic regression revealed a positive correlation and statistical significance only among individuals who used treatment support medication (p < 0.001). Conclusion: in order for measures to be more effective, strategies for approaching smokers should comprise a knowledge of patient profiles and provision of treatment medication.
Descriptors: Tobacco use disorder; tobacco use cessation; nursing; treatment.
INTRODUCTION
Smoking is still considered a serious public health problem and is the leading cause of preventable death, according to the World Health Organization (WHO), which kills about 6 million people a year worldwide approximately. By 2030, if the current trend in cigarette consumption continues, 8 million annual deaths are estimated1. There are approximately 1 billion smokers in the world, and 80% of them live in underdeveloped and low-income countries, which make tobacco-related deaths more frequent and common in these populations.
Factors such as schooling, socioeconomic conditions and degree of nicotine dependence are circumstances associated with the prevalence of smoking and the difficulty of cessation of smoking; thus, smoking affects more the populations with low socioeconomic levels not only in Brazil, but also in other countries.
The smoke produced by the cigarette contains about 4,720 substances in 15 chemical functions, of which 60 are carcinogenic and others are known to be toxic; but nicotine has been the cause of tobacco dependence. Policies for smoke-free environments should be encouraged to avoid smoking in all the enclosed environments, such as households, work, leisure, schools, health services, businesses, and public places, creating 100% smoke-free environments4-6
Considering all these issues, the Ministry of Health, together with the National Cancer Institute (INCA) developed in 1989 the National Tobacco Control Program (PNCT) to reduce the prevalence of smokers and morbidity and mortality from diseases related to tobacco. In this scenario, to achieve part of the goals sought, and in view of the size of the Brazilian territory, the PNCT began to decentralize its actions and establish partnerships with the state and municipal health secretaries.
After evaluating the effectiveness of the methodology used in the approach and treatment of smokers, INCA, in conjunction with the Ministry of Health and in compliance with the Framework Convention on Tobacco Control (FCTC), established the theoretical bases and guidelines for the treatment of smokers in the groups of support to the smokers, namely: cognitive-behavioral approach that combines cognitive interventions and behavioral skills training aiming at the detection of situations of risk, of relapse and the development of coping strategies; and the use of pharmacotherapy that can be used as a support measure for the cognitive-behavioral approach where drugs are offered3.
But treating the smokers is a challenge for the healthcare professionals, especially in places where the financial resources are scarce. Moreover, the knowledge of the target audience is extremely necessary for an adequate structuring of the programs, which allows the specific needs of each population to be met.
Therefore, the present study aimed to identify the profile of patients enrolled in the Smoking Cessation Program of the Federal University of Triângulo Mineiro (UFTM) and to relate the factors associated with the therapeutic success.
LITERATURE REVIEW
The cultivation of the tobacco plant probably began with the indigenous migration, when the Portuguese discovered Brazil; in the sixteenth century they learned about the plant and helped to spread tobacco through Europe and later to the whole world.
Since the 1960s, cigarette smoking has been linked to illness and impairment of the health of the smokers, and several surveys worldwide have been published proving the harm caused by smoking. In that first moment, the great concern with the damages that the cigarette could cause to these people arose. In a second moment, other questions emerged, such as the environmental tobacco smoke pollution and the problems arising from the cigarette smoke to the general population1,2.
In 1989, according to a study carried out by the Ministry of Health, 33% of the Brazilian population aged 15 years old or over used tobacco products, but there was a significant decline in the prevalence of smokers over the years to 17.2% in 20084.
For a long time, Brazil has been considered the world's largest exporter of tobacco and the second largest producer of the drug, being placed it in the spotlight in the Brazilian economy. But it is expected that, with the decrease of the consumption of the cigarette by the population in the country, the production of Brazilian smoke will gradually decrease 4.
Estimated data, recently released by the Vigilance of Risk Factors and Protection of Chronic Diseases by Telephone Inquiry (VIGITEL), revealed that in 2011, 14.8% of the adult population smoked, being 18.1% men and 12% women. However, smoking still affects several countries with high prevalence rates of the drug use, such as in China where the prevalence of male smokers is 52.9%. In Argentina, Bolivia, Paraguay, and Uruguay there is a prevalence of 21.6% to 30.7% of male smokers while the prevalence in females reaches 22%5.
The reduction in the prevalence of tobacco smokers in Brazil was due to anti-smoking campaigns and the adoption of measures taken by the government to create laws, together with INCA; and after the implementation in 2005 of the FCTC created by the WHO in 20036.
Although the Brazilian tobacco control legislation is one of the strongest in the world, it is constantly challenged, since it has contributed to advances such as the significant reduction in the national consumption over the last decades. However, there are still difficulties in combating smoking due to easy access to the drugs by the general population, the smuggling of cigarettes from Mercosur countries, the low cost of the product on the market and the lack of adequate treatment for the population in some regions of the country and at different socioeconomic levels6.
METHODOLOGY
This is a retrospective study, with a quantitative data approach that was carried out in the UFTM Smoking Cessation Program. For the accomplishment of the research, all the records of smokers who sought care in the period from February 1, 2009 to December 31, 2013 were analyzed. All patients who had sufficient data to perform the research were included in the study.
Patients were treated according to the format and guidelines proposed by the INCA3. Thus, ambulatory care was structured with weekly frequency in the first month, biweekly until completing the intensive approach (three months) and finally monthly up to one year. The visits were performed individually, and each patient underwent an initial medical care for clinical assessment and then a session with the psychologist. At that time, the smoker's profile, their degree of nicotine dependence through the Fagerström's7 scale and their motivation to quit smoking according to the Transchatic Model of Prochaska and Diclemente, which consists of an interview to evaluate the motivational stage in which the smoker finds themselves to quit smoking was valued8.
The motivational stages are described as pre-contemplation, in which the person does not yet see a need to change their behavior; contemplation, the individual perceives their problem but still does not mobilize to take an attitude of change; preparation, the person already has a clearer and more precise view of their problem and begins to think about actions that can help them recover and overcome limitations; ready for action, the client begins to put into practice their efforts to chance; and, lastly, maintenance that is the most complex and challenging stage, since the individual must make every effort to avoid relapses8.
During the treatment, the pharmacological therapy was not provided by the service and was prescribed by the team physician for the patient to purchase with their own financial resources. Nicotine replacement therapy was used through transdermal patches, with the dosage determined according to the Fagerström's Test, which may or may not be associated with bupropion.
The data collection took place in the same service that aided the smokers. An instrument composed of closed questions was elaborated in two parts, that is, one for the identification of socioeconomic and demographic profiles and the other involving specific questions on the theme of the research - smoking, such as the presence of comorbidities, the smoking profile and the degree of motivation for cessation of smoking. Thus, the following variables guided the study: age, gender, marital status, schooling, income, time of cigarette use, number of cigarettes smoked per day, previous attempts to quit smoking with or without specialized help, service demand, clinical comorbidities, use of support medication for treatment, treatment withdrawal, the Fagerström's test, the Transchatic Model of Prochaska and Diclemente and the therapeutic success of smokers enrolled in the service.
The data obtained were categorized into a database in the Excel Software ( Microsoft Corp. United States), carried and processed in the statistical software Statistical Package for the Social Sciences (SPSS) version 20.0, where the mean and standard deviation of the numerical variables and of the categorical variables and the percentage values were determined. To reach the proposed goal, multiple binomial logistic regression was used, with the therapeutic success as a predictor and as predictors the degree of nicotine dependence, the degree of motivation for the treatment and the use of medication of the smokers during the treatment, the significance level α=5 (p<0.05) was adopted.
This study followed the ethical principles and this project was developed after approval by the Ethics and Research Committee of the Federal University of Triângulo Mineiro and the University of São Paulo under protocol number 2272.
RESULTS AND DISCUSSION
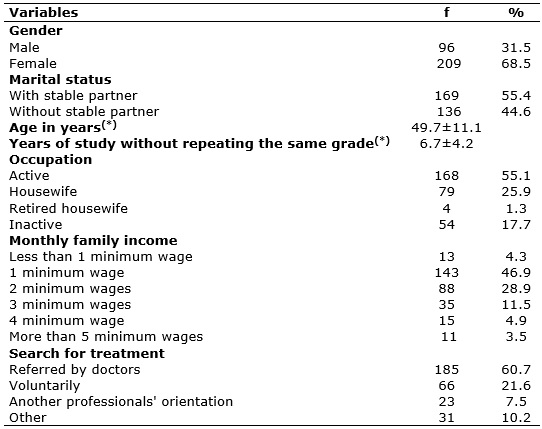
The medical records of 340 smokers were evaluated, of which 35 were excluded because they were filled out incorrectly. Of the 305 smokers assessed, 68.5% were female, with a mean age of 49 ± 11.1sd. More than half (55.4%) reported having a stable marital relationship and when analyzing their monthly family income, it was observed that the majority (80.1%) received up to 2 minimum wages, with an average of 6.7 ± 4.2sd years of study, as shown in Table 1.
TABLE 1:
Distribution of the tobacco smokers according to demographic
characteristics. Uberaba-MG, 2014
Result expressed in mean and ± sd(*)
The predominance of the demand for treatment for smoking cessation by women can be attributed to the concern of these patients with their health since the majority were referred by health professionals and possibly had already had some type of previous advice. The greater number of women in treatment also reinforces the idea that the male population needs health promotion strategies and incentives so that the demand for men's smoking cessation treatment increases among the groups that provide this type of care9-11. Regarding the age, the data found suggest that people seek treatment after a certain maturity, usually when there was the awareness that smoking can cause damage to health, and especially when clinical manifestations appear that harm people in their daily life. Similar results in relation to gender and age are described in other studies12-14.
The association between smoking, low education and low income is described in national and international studies15-17. Higher education promotes greater awareness of people about the cigarette damage and benefits when a person decides not to continue using tobacco, which contributes to lower the cigarette use in the populations with higher education, whereas the maintenance of smoking habits has had a strong relation in the population with a low level of education. The association of these two factors, low income and low level of education, further increases the prevalence of smoking. But there are other factors such as low price and easy access to tobacco that have contributed to the spread of the drug use by populations with these characteristics18.
Currently, in addition to anti-smoking awareness campaigns, and to comply with the measures proposed by the WHO through the FCTC, Brazil has invested in raising taxes on tobacco products to restrict their commercialization and to create laws that prohibit the use of the product indoors, creating environments free from tobacco and from the smoke of tobacco products6,19,20.
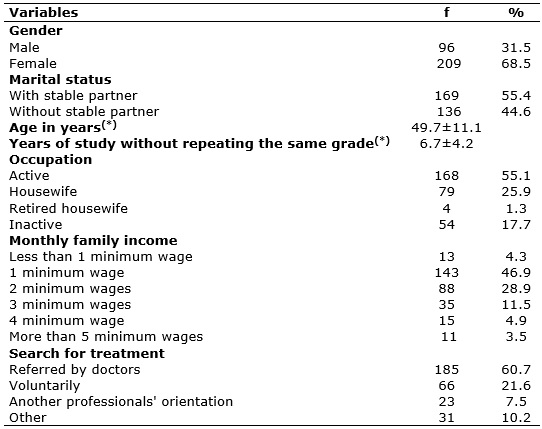
The majority had a high (46.9%) and very high (23%) degree of nicotine dependence, with a mean of 43.0 ± 28.3 years/package. A large part of the population (69.8%) had already made at least one attempt to quit smoking, either alone or with specialized help, and in assessing the motivation of these individuals, 91.1% were in the phase - ready for action to quit smoking, as described in Table 2.
TABLE 2:
General characteristics of the tobacco smokers. Uberaba-MG, 2014.
(*)
Results expressed as mean and ± sd (**)Fagerström Test (***)Some patients had more than one co-morbidity
For a long time, tobacco smoking has been a risk factor for the health, considered the leading cause of death that is preventable and responsible for some diseases such as malignant, cardiovascular and respiratory system neoplasms1. In the study population, most smokers presented comorbidities, and the systemic arterial hypertension was the one that excelled the most, which corroborates the relation between cigarette smoking and cardiovascular diseases1,21. A similar outcome was reported in another smoking cessation program22. However, in other studies involving smokers, the (COPD) and other respiratory manifestations were evidenced as the main comorbidities associated with cigarette smoking23,24.
In this study, those manifestations are shown in second place in the list of comorbidities presented by the tobacco smokers. As most adults in this study were in a stable relationship, the likelihood of their partners or children developing the same diseases increases further. Therefore, it should be considered that the non-smokers, known as passive smokers, who cohabit with smokers indoors are also exposed to the products derived from the smoke released by the cigarette and may become ill and have their health impaired25.26.
Regarding the time of exposure of cigarette smokers, an average of 33.4 years was observed, more than half of the patients that sought care had a high and very high degree of nicotine dependence (69.9%), which is consistent with data found in other studies21,27. The high level of nicotine dependence of the tobacco smokers found through the Fagerström's Test may reflect, over time, a greater number of diseases associated with smoking.
This result is important and should be considered when planning the therapeutic actions and strategies to be established since nicotine addiction has been the greatest difficulty during the treatment of these patients and the withdrawal syndrome is directly related to this addiction 28. Thus, such knowledge becomes extremely important to the therapeutic success. The manual on the addressing and treatment of smokers, prepared by the INCA, recommends that, in patients with these characteristics, it is necessary to make the option for the use of support medication to aid the treatment3.
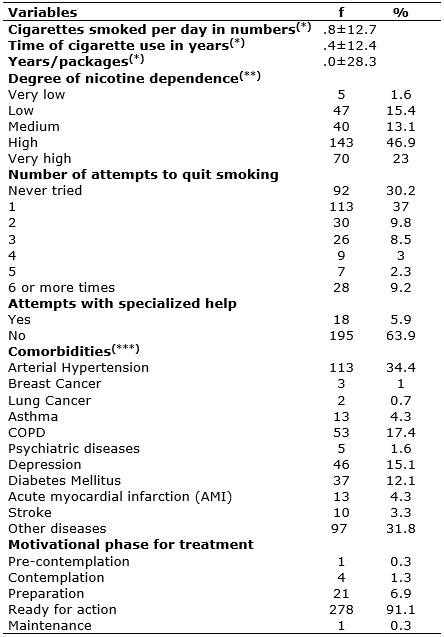
The medicine forms used for the treatment of patients in this study were Nicotinic Replacement Therapy (NRT) through the transdermal patch and, when necessary, Bupropion was used. Only 52.1% of the tobacco smokers made use of the medicine. This result may be related to the fact that the service did not provide free medication support. The medication was prescribed in medical prescription so that the patient acquired it with proper resources. Nevertheless, it was observed that the medication support contributed significantly (p<0.05) in the therapeutic success of the tobacco smokers that had used it, as described in Table 3.
TABLE 3:
Results of multiple binomial logistic regression analysis, with success as
a therapeutic outcome. Uberaba-MG, 2014.
A study conducted to evaluate the use of the NRT concluded that all available forms of this type of therapy can increase therapeutic success rates by 50% to 70%29. Another commonly used drug in combination with NRT is Bupropion, which is generally recommended for the treatment of severe withdrawal symptoms and in patients with high levels of anxiety and/or depression.
In addition to pharmacological resources, the non-pharmacological approach, such as behavioral interventions, is also an excellent tool in the treatment of smokers; and the association of these two measures significantly increases the chances of therapeutic success, especially with clients that are considered heavy tobacco smokers. The approach, even if simple and with an emphasis on motivation for smoking cessation, has yielded excellent results. But it is worth emphasizing that because it is a multifactorial problem, smoking cessation does not depend exclusively on medical guidelines and/or drug use, the therapeutic success goes beyond the smoking cessation treatment groups31,32.
It is known that most tobacco smokers make several attempts to quit smoking before achieving full therapeutic success, and the clear majority choose not to seek help from qualified professionals. In more than half of the patients of this study there was at least one unsuccessful attempt, either with help or without specialized help, which is described in other studies33,34.
The frustrated attempts, the abandonment, the failure, and the difficulty to follow the therapeutic regimen proposed during treatment have been related to nicotine dependence and to the motivational state in which the smoker is to receive and carry out the treatment35.
In the present study, most tobacco smokers were in the motivational phase ready for action and no statistical significance was observed in the association of the degree of motivation (p<.994) with nicotine dependence (p<0.628) among those who reached therapeutic success, as shown in Table 3. A different result was found in a study conducted to assess the motivational level associated with failure to quit during smoking cessation treatment, where the low motivational level, the high degree of nicotine dependence, higher smoking charge, and high levels of anxiety were associated with the therapeutic failure35.
The motivational state of the smoker is an important factor and it also directs the approach and the need to cultivate the behavior presented by the smoker who often seeks help but is not yet prepared to quit smoking 22. Thus, it is fundamental that the health professionals are receptive and open to those patients who are at a low motivational level and who are resistant to the proposed treatment in the groups of treatments for smokers. Then, the monitoring of the motivational state of the tobacco smokers during treatment becomes essential to also implement the approach and define strategies for a treatment as effective as possible35 .There was no statistically significant difference between the gender (p=0.267), the income (p=0.717) and the educational level (p=0.363) of the smokers to therapeutic success in this study, according to the data presented in Table 3.
A high abandonment rate was observed - 258 (84.6%) and only 47 (15.4%) smokers achieved therapeutic success. Regarding the treatment withdrawal, this study is in accordance with other studies conducted in Brazil, involving tobacco smokers21,22,35. Regarding the therapeutic success, there is a great variability of the results described in the literature. A similar result was found in a survey carried out by the National Agency of Sanitary Vigilance, through the Brazilian Bulletin of Health Technology Assessment (BRATS), which revealed smoking cessation rates, generally below 30%, in agreement with another study, conducted in Vitória-ES, in which smoking cessation rates of 28.7% was observed 32.
However, other studies that evaluate the effectiveness of treatment for smokers found smoking cessation rates above 60%36-38. The fact that the service does not provide free drug therapy, as well as low income, low educational level and the high degree of nicotine, are factors that may have contributed to the high number of treatment withdrawal.
Therefore, when performing the multiple binomial logistic regression analysis, with the therapeutic success, as a result, it was observed that only the use of the medication was statistically significant (CR (CI) = 5.64 / 2.40-12.70), that is, the tobacco smokers who used the medication had 5.64 times more chances of achieving therapeutic success than those who did not use the medication.
This study was observational, and its results cannot be extrapolated to other populations. Although other supplemental health services have not been evaluated, this research provides useful data for other public services that assist tobacco smokers, emphasizing the importance of the free distribution of support medication for treatment.
CONCLUSION
The study described that the patients who sought tobacco smoking cessation care had a low educational level, low economic status, high and very high levels of nicotine dependence, were mostly in the motivational phase ready for action and the pharmacotherapy was not provided for free during treatment.
Since the supportive medication was statistically significant, these data reinforce the idea that in the tobacco smoking cessation programs, the evaluation of the profile of the patients served, the supply of the medication for the treatment, associated with behavioral measures, should be part of the smoker's approach and treatment strategies so that the actions are more effective.
In addition, tobacco smoking cessation programs should offer alternative approaches and treatment with a view to a greater adherence to the treatment of males. This article also opens margins so that further studies can be carried out to identify other factors of failure in the treatment of these patients, which will make it possible to improve the approach and follow-up of these tobacco smokers to increase the success of the tobacco smoking cessation.
REFERENCES
1.World Health Organization. Enforcing bans on tobacco advertising, promotion and sponsorship. Genebra (Swi): WHO; 2013:11-201.
2.World Health Organization. Strong monitoring keeps countries on track to combat the tobacco epidemic. Genebra (Swi): WHO; 2017.
3.Ministério da Saúde (Br). Instituto Nacional de Câncer. Abordagem e tratamento do fumante: consenso 2002. Rio de Janeiro: Instituto Nacional de Câncer; 2002.
4.Szklo AS, Levy D, Souza MC, Szklo M, Fiqueiredo VC, Perez C et al. Changes in cigarette consumptiom patterns among Brazilian smokers between 1989 and 2008. Cad. Saúde Pública (Online). 2012; 28(11): 2211-5.
5.Ministério da Saúde (Br). Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: VIGITEL 2011. Brasília (DF): Secretaria de Vigilância em Saúde; 2012.
6.Silva ST, Martins MC, Faria FR, Cotta RMM. Combate ao tabagismo no Brasil: a importância estratégica das ações governamentais. Ciênc. saúdecoletiva (Online). 2014; 19(2): 539-52.
7.Fagerström KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict. behav. 1978;3(3-4):235-41.
8.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J. Consult. Clin. Psychol. 1983;51(3):390-5.
9.Correa ACP, Mozer IT. Gestão do processo de implementação da política de saúde do homem. Rev. enferm. UERJ. 2016; 24(1):e9483.
10.Piovesan LR, Schimith MD, Simon BS, Budó MLD, Weiller TH, Brêtas ACP. Promoção da saúde na perspectiva de enfermeiros de atenção básica. Rev. enferm. UERJ. 2016; 24(3):1-11;e5816.
11.Costa ECV, Trovisqueira AM. Perfil sociodemográfico e clínico de uma amostra de fumantes portugueses: implicações do sexo para a intervenção na cessação tabágica. Psic. teor. Pesquisa. 2016; 32(2);e322221.
12.Marino MG, Fusconi E, Magnata R, Panà A, Maurici M. Epidemiologicdeterminantsaffectingcigarettedmokingcessation: a retrospectivestudy in a nationalhealth system (SSN) treatmentservice in Rome (Italy). Journal of Environmental and Public Health. 2010:1-9.
13.Castro MRP, Matsuo T, Nunes SOV. Caracteristicasclínincas e qualidade de vida de fumantes em um centro de referência de abordagem e tratamento do tabagismo. J. bras. pneumol. 2010; 36(1):67-74.
14.Echer IC, Corrêa APA, Lucena AF, Ferreira SAL, Knorst MM. Prevalence of smoking among employees of a university hospital. Revista latino-am.enferm. (Impresso). 2011; 19(1):1-8.
15.Barros AJD, Cascaes AM, Wehrmeister FC, Mesa JM, Menezes AM. Tabagismo no Brasil: desigualdades regionais e prevalência segundo características ocupacionais. Ciênc. saúdecoletiva (Online). 2011; 16(9):3707-16.
16.Palipudi AM, Gupta PC, Sinha DN, Andes LJ, Asma S, McafeeT.Social Determinants of Health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. 2012; 7(3):1- 9.
17.Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M. Socioeconomic status and smoking: a review. Ann. N. Y. Acad. sci. 2012;1248(1):107-23.
18.Fagundes LG, Martins MG, Magalhães EMS, PalmiériPCR,Silva Júnior SI.Políticas de saúde para o controle do tabagismo na América Latina e Caribe: uma revisão integrativa. Ciênc. saúde coletiva (Online). 2014; 19(2):499-510.
19.Silva ST, Martins MC, Faria FR, Cotta RMM. Combate ao tabagismo no Brasil: a importância estratégica das ações governamentais. Ciênc. saúdecoletiva (Online). 2014; 19(2):539-52.
20.Hughes JR, Solomon LJ, Naud S, Fingar JR, Helzer JE, Callas PW.Natural history of attempts to stop smoking. Nicotine&TobaccoResearch. 2014: 1-9.
21.Dias CRK, Hertel KS, Gregórios F, ViguerasESR,Goldmeier S. Programa de cessação do tabagismo: resultados em pacientes cardiopatas. Rev. bras. ciênc. saúde. 2014; 12(39):21-27.
22.Manso MEG, Silveira RS, Godoy MC, Lima M. Programa para cessação de tabagismo em uma operadora de planos de saúde: relato de experiência. Rev. bras. med. 2013:1-8.
23.Carvalho AA, Gomes L, Loureiro L, Bezerra AJ.Controle do tabagismo em instituição de longa permanência. Ciênc. saúdecoletiva (Online). 2013; 18(4):1119-30.
24.Silva ERP, Fonseca FLA, Pinto JL, Oliveira LC, Fonseca ALA, Gehrke FS. As principais doenças associadas ao tabagismo e o tratamento medicamentoso no combate à dependência pelo Sistema Único de Saúde. Saúde Meio Ambient. 2014; 3(1):51-8.
25.Ribeiro AG, Cotta RMM, Ribeiro SM. A promoção da saúde e a prevenção integrada dos fatores de risco para doenças cardiovasculares.Ciênc. saúdecoletiva (Online). 2012; 17(1):7-17.
26.Oliveira RS, Martins IML, Souza LPS, Souza EMO, Teles JT, Santana JMFetal.Fatores de risco associados às doenças cardiovasculares na população carcerária. Gestão & Saúde. 2014; 5(1):263-75.
27.Meier DAP, Vannuchi MTO e Secco IAO. Abandono do tratamento do tabagismo em programa de município do norte do Paraná. Espaç. saúde (online). 2012; 13(1):35-44.
28.Santos JDP, Duncan BB, Sirena AS, Vigo A, Abreu MNS. Indicadores de efetividade do programa de tratamento do tabagismo no sistema único de saúde em Minas Gerais, Brasil, 2008. Epidemiol. serv. saúde. 2012; 21(4):579-88.
29.Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K, Lancaster T. Nicotine replacement therapy for smoking cessation (Review). The Cochrane Library. 2012. p. 18-24.
30.Stapleton J, West R, Hajek P, Wheeler J, Vangeli E, Abdi Z et al. Randomized trial of nicotine replacement therapy (NRT), bupropion and NRT plus bupropion for smoking cessation: effectiveness in clinical practice. Addiction Research Report. 2013; 108(12):2193-201.
31.Roberts NJ. Kerr SM, Smith SMS.Behavioral interventions associated with smoking cessation in the treatment of tobacco use. Health Serv Insights.2013; 6: 79-85.
32.Bartlett YK, Sheeran P, Hawley MS. Effective behavior change techniques in smoking cessation interventions for people with chronic obstructive pulmonary disease: a meta-analysis. 2014; 19(1):181-203.
33.Sattler AC,Cade NV. Prevalência da abstinência ao tabaco de pacientes tratados em unidades de saúde e fatores relacionados. Ciênc. saúdecoletiva (Online). 2013; 18(1): 253-64.
34.Karen SKK, Oliveira ML, Pádua AI, Vieira F, Martinez JAB. Características clínicas de fumantes atendidos em um centro de referência na cessação do tabagismo. Medicina (Ribeirao Preto). 2012; 45(2):337-42.
35.Pawlina MMC, Rondina RC, Espinosa MM, Botelho C.Ansiedade e baixo nível motivacional associados ao fracasso na cessação do tabagismo. J. bras. psiquiatr. 2014; 63(2):113-20.
36.Mesquita AA. Avaliação de um programa de tratamento do tabagismo. Rev. bras. ter. comport. cogn. 2013; 15(2):35-44.
37.Meier DAP, VannuchiMTO,Secco IAO. Abandono do tratamento do tabagismo em programa de município do norte do Paraná. Espaç. saúde (online). 2011; 13(1):35-44.
38.Goyatá SLT, Silva MJD, Souza WA, Podestá MHMC, Beijo LA. Impacto do programa de apoio ao tabagista de um município do sul de Minas Gerais, Brasil. Cienc.enferm. 2014; 20(1):75-88.