ORIGINAL RESEARCH
Characterizing women in the pregnancy-puerperal cycle and encouraging early breastfeeding
Andréa Cristina de Morais Chaves ThulerI; Marilene Loewen WallII; Marli Aparecida Rocha de SouzaIII
I
Nursing PhD Student in the Postgraduation Program of the Federal University
of Paraná. Brazil. E-mail: andrea.chaves@ufpr.br
II
PhD. Professor at the Federal University of Paraná. Brazil. E-mail: wall@ufpr.br
III
Nursing PhD Student in the Postgraduation Program of the Federal University
of Paraná. Brazil. E-mail: marlirochasouza2@gmail.com
DOI: https://doi.org/10.12957/reuerj.2018.16936
ABSTRACT
Objective: to develop socioeconomic, gynecological and obstetric profiles of the women, and to identify their early contact with their newborns. Methods: in this quantitative, descriptive, longitudinal study, 51 women were interviewed between November 2013 and June 2014 at a public maternity hospital in southern Brazil. The study was approved by the research ethics committee. Results: mean age 26.2 years, married/stable union (80.39%), over 8 years' schooling (60.78%), family income 1 to 3 minimum wages (66.67%), exclusively housewives (80.39%), primigravidas (52.94%), no prior abortion (92.15%), had attended more than 6 appointments (100%), and received no guidance on breastfeeding (54.90%). Conclusion: most of the puerperas who underwent cesarean section had no skin-to-skin contact in the delivery room, with the opposite occurring in cases of normal birth
Descriptors: Breastfeeding; maternal and child health; nursing; health education.
INTRODUCTION
The pregnancy-puerperal cycle is a physiological process that generates physical, psychological, and social changes and is influenced by several factors such as biological changes and socioeconomic characteristics, in addition to cultural aspects, in which she is inserted.1
Therefore, it is essential to know these women and to recognize early on the part of pregnant women who may present risks during pregnancy and the follow-up should aim to clarify doubts and demystify the beliefs of this period, especially regarding breastfeeding.
The Ministry of Health (MH) stresses the importance of this follow-up in the basic health units (BHU) and, therefore, recommends that the prenatal care should have at least six visits, the first being performed as early as possible and the other interspersed between the nurse and the doctor.
These consultations carried out with quality promote the health of newborns, better intrauterine growth, greater birth weight, less occurrence of prematurity and neonatal mortality. For the mother, the benefits are significant - lower gestational intercurrent rate and complications at the time of delivery, as well as stimulation and support for breastfeeding.1,4
The strategies to support, promote and encourage breastfeeding should be present throughout the pregnancy cycle, including clarifying the benefits of breastfeeding to the mother/child binomial. This practice is considered a universal strategy for the reduction of morbidity and mortality rates in childhood and adulthood.1,5-7 However, for the prevention of mortality and morbidity, it is necessary for the pregnant women to be guided on the benefits of breastfeeding and skin-to-skin contact with the newborn, strategies that promote the increase of exclusive breastfeeding babies, a greater bond between the binomial and, consequently, the reduction of early weaning.8,9
In view of the above, this study aimed to characterize the socioeconomic, gynecological and obstetric profiles of women and to identify their early contact with the newborns.
LITERATURE REVIEW
The health professional who knows the socioeconomic and cultural characteristics of the family in which the newborn will be inserted can guide the family members and the pregnant woman, regarding the beliefs related to breastfeeding, to strengthen the self-efficacy of the nursing mothers. Studies report that common sense, inadequate supply, grandparents' influence and use of pacifiers and bottles are the main factors of the early weaning.10
Thus, the act of breastfeeding remains the focus of discussion and challenges the health services, because despite the advantages and strategies developed for support, promotion, and protection of breastfeeding since the 1980s, such practice is still far from that proposed by the World Health Organization (WHO), which recommends exclusive breastfeeding until the child's sixth month of life and, in a complementary way, until two years of age or over.7 it is believed that although health professionals present attitudes and speeches favorable to breastfeeding, they are often not close and do not experience the moments of the women's (un)success in the lactation process.
In 1992, the MH, supported by WHO and the United Nations Children's Fund (UNICEF), adopted the Baby-friendly Hospital Initiative (BFHI) based on the Ten Steps to Successful Breastfeeding, which summarize the practices needed to be developed in maternity hospitals to support breastfeeding.9 Among them, the 4th step is to: put the newborn in direct contact with the mother immediately after childbirth for at least one hour and encourage the mother to identify if the baby is ready to be breastfed, offering help if necessary.9
In 2015, WHO and UNICEF initiated a process to re-evaluate and reinvigorate the BFHI program; thus in 2018, the new version for the implementation of the BFHI was launched, that reinforces that contact between mothers and babies, which should be facilitated and encouraged as soon as possible after birth, so that it must be uninterrupted for at least 60 minutes. This recommendation is also possible after a cesarean section with epidural anesthesia since even if mothers and infants are unable to initiate breastfeeding in the first hour, this approach provides skin-to-skin contact and this is the beginning of the family bond.11
Every pregnant woman needs to be informed about the importance of her right to early contact with the newborn in the delivery room. Because in addition to stimulating and intensifying this bond, this early contact provides calmness between these two, helps stabilize the blood, heart rate and breathing of the child, reducing the baby's stress and heat loss.7,12
METHODOLOGY
A quantitative, descriptive, longitudinal study conducted between November 2013 and June 2014, in a maternity hospital in the Metropolitan Region of Curitiba/PR that provides care to pregnant women at normal risk.
Two structured instruments were developed with open and closed questions, developed by the researchers and based on obstetrical literature. The instruments were applied in different periods with the same participants: during pregnancy (1st moment) and during the immediate puerperium (2nd moment).
During the first moment, the instrument was applied to the pregnant participants in order to verify the socioeconomic and gynecological characteristics. After the delivery, characterized in this research as the 2nd moment, the questions were related to the type of delivery, breastfeeding, and skin-to-skin contact with the newborn.
The data collection was performed between November 2013 and May 2014 due to the need to wait for the delivery date. The sampling was for convenience, that is, all the pregnant women that met the inclusion criteria in the research, which were: pregnant women over 18 years old, from the third trimester of pregnancy, who participated in the maternity visit. And as exclusion criteria, the presence of physical and/or mental restrictions that made it impossible to understand the instrument.
The participants signed the Free and Informed Consent Term (FICT), and to ensure their anonymity, the form of identification was with the letter G followed by the sequence number of the application of the instrument.
After the data collection, the data were stored in the Microsoft Excel® 2007 software and later submitted to descriptive statistics, the results were presented through tables with absolute frequency, percentage, mean and standard deviation of the variables. The study was approved by the Research Ethics Committee of the Health Sciences Sector of the Federal University of Paraná with the Certificate of Presentation for Ethical Consideration CAAE 19619213.0.0000.01102.
RESULTS AND DISCUSSION
Among the 51 pregnant women who participated in the study, the ages presented were between 19 and 42 years old (mean of 26.2; SD=5.8), of these 23 (45.10%) with higher prevalence in the age group of 19-24 years old and who began their participation in the research around the 33rd gestational week.
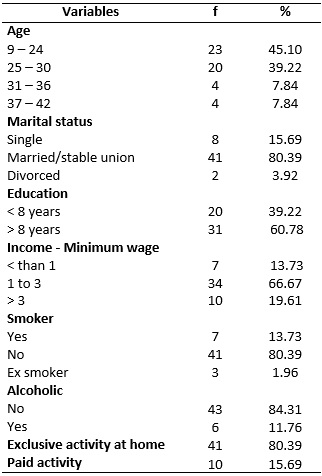
The data on the marital status showed that 41 (80.39%) were married or in a consensual union, 31 (60.78%) reported that they had more than 8 years of study, 41 (80.39%) had no history of smoking, 43 (84.31%) without the use of alcoholic beverages, 41 (80.39%) only exerted activities at home, 31 (66.67%) pregnant women had a family income of between 1 and 3 minimum wages, with a per capita income of a minimum wage, due to the average of 3 people living in the same household, as explained in Table 1.
TABLE 1:
Sociodemographic and behavioral characteristics of the pregnant women.
Metropolitan Region of Curitiba/PR, 2013/2014. N(51)
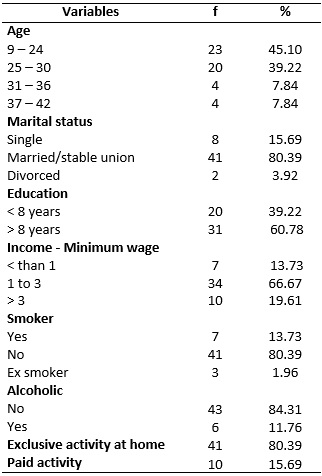
This study identified a group of pregnant women with a predominance of young adults, married, with a good level of schooling, family income of up to 3 minimum wages and absence of addictions, such as alcoholism and smoking. These data are close to the results of the report of the National Survey of Demography and Child and Women's Health (PNDS),14 in which the average age found in the South Region was over 31 years old. In the report on the satisfaction of puerperal women treated in the Unified Health System (SUS), the age of 53.10% of the postpartum women ranged from 20-29 years old13, corroborating the present study, which demonstrated the prevalence of the age range of the younger women - 19-24 years old.
The youngest maternal age is related as an unfavorable factor to breastfeeding, in all Regions of Brazil14. A fact that directs the professional to motivate these women, when they encounter some difficulty (insecurity, lack of confidence in themselves and lack of support from family members), as a means of avoiding the early weaning.9 Therefore, to support the breastfeeding process, it is necessary to exchange experiences, backgrounds, and knowledge to strengthen the family support, considering the characteristics of each family.15
Most of the women (80.39%) declared themselves married or on a stable union, corroborating the satisfaction report in which 57.40% of women were married and/or on a stable union. This factor is favorable since women who have partners tend to receive more support during pregnancy and breastfeeding.16 They feel more capable in relation to breastfeeding when they perceive that their partners act in an active way and, therefore, strategies to reinforce this support must be implemented for both the woman and her partner and initiated in the prenatal phase with postpartum continuity.16,17
The paternal participation in the breastfeeding process was evaluated in a survey conducted in the Central-West Region of Brazil and found that 58.93% of the fathers did not receive any guidance on breastfeeding.18
The parental inclusion in maternal and child health and health education are increasingly present, but health professionals are not able to receive them in prenatal consultations or even in obstetric centers, because during the undergraduate program, the topics covered are mainly about milk technique, management, and composition, excluding the psychological aspects and the father's inclusion during the pregnancy-puerperal cycle.15 Thus, the importance of the approximation between the academic education and the health service is emphasized, in order to contribute to the improvement of the training process and the development of the competencies necessary for the professional practice.19
Regarding the prevalence of breastfeeding, low-income countries had an advantage, however, when compared with rates of early onset and exclusive breastfeeding, the data were unsatisfactory.20
It is possible to observe the predominance of primigravidae - 27 (52.94%) - without a history of miscarriage - 47 (92.15%) and although 100% of the pregnant women performed more than 6 prenatal consultations, only 19 (37,25%) performed between 1-2 consultations with nurses (mean of 1.08, SD=0.87); and 28 (54.90%), that is, more than half of the participants did not receive orientation about breastfeeding in the prenatal period, according to Table 2.
TABLE 2:
Gynecological characteristics and prenatal follow-up of pregnant women.
Metropolitan Region of Curitiba/PR, 2013/2014. N(51)
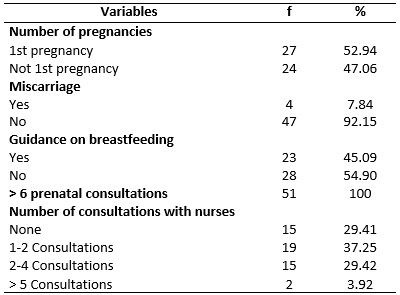
According to the MH, for a minimally adequate prenatal care, in addition to the six consultations, it is recommended that care be provided with educational and preventive actions, without unnecessary interventions with the early detection of pathologies and risk situations, as well as establishing the client/health team link and knowledge of the place of birth.
The support for breastfeeding should start during the prenatal care so that the difficulties are recognized and overcome. According to the MH, the guidelines during the consultations should inform the advantages of breastfeeding, promote self-confidence and ability, through teaching positioning techniques and correct holding.21
There was a predominance of primigravidae with no history of miscarriage, with children who were born through natural birth and who had contact with the baby in the first hour in the delivery room; also prevailed the feeding of the newborn in the maternity, through the breastfeeding.
Regarding the delivery route, it was observed the predominance of vaginal delivery - 31 (60.79%), of the contact with the newborn in the first hour in 28 (54.90%); the delivery room was the place where the baby suckled for the first time - 28 (54.90%), the feeding of the newborn in the maternity ward was exclusive breastfeeding - 43 (84.31%), according to the Table 3.
TABLE 3:
Obstetric characteristics of pregnant women and encouragement of
breastfeeding. The metropolitan region of Curitiba/Paraná. November 2013 to
June 2014. (N=51)
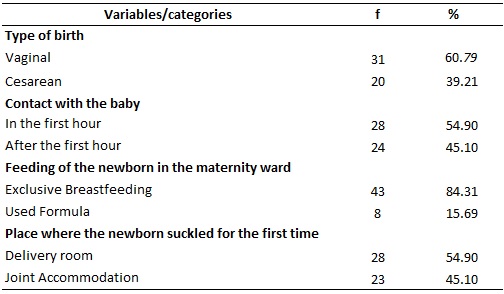
In this study, although most births occurred through vaginal deliveries, the number of cesareans reached 39.21%, higher than that recommended by the MH - 15% rate of surgical deliveries. Compared to the data found in PNDS (27.3%), it is observed that the number of cesareans in Brazil has been increasing significantly. In just 8 years (2000-2008), there was an increase from 38% to 48.8%, with 35% of births being performed by SUS and 80% by the private sector.13 According to a report by the PNDS, the cesarean section has already become more frequent than the normal birth in the Southeast and South regions, respectively, in 51.7% and 51.6% of births
The normal childbirth is safer and it must be stimulated in a humanized way, thus promoting the minimum of interventions. However, if necessary, the professional should rely on scientific evidence and clinical protocols to interrupt the physiological process of childbirth.5
According to a systematic review, the cesarean section was considered the main risk factor for not breastfeeding in the first hour of life.22 The skin-to-skin contact during the first hour of the newborn's life strengthens the binomial's bond even for mothers who cannot breastfeed. This procedure, known as alert inactivity, stimulates the recognition between mother and child, continuing the bond initiated in intrauterine life.5,9,22
In this study, 54.90% of the 60.79% who were born vaginally had skin-to-skin contact, corroborating a study carried out in Portugal, in which newborns who did not start breastfeeding in the first hours were born through cesarean section.23 The birth by surgical procedure contributed in this study to the early separation of the binomial, leading to consider that the operative procedures hamper the accomplishment of the 4th step of the BFHI.
The non-adherence to the 4th step of BFHI persists; in a study conducted in the Northeast Region of Brazil, the average length of the permanence of infants in skin-to-skin contact did not exceed 30 minutes, demonstrating the discrepancy between scientific evidence and clinical practice.24
According to WHO, breastfeeding offered in the first hour of life is considered an indicator of excellence and, therefore, rates the percentage of adherence to breastfeeding in the first hour for healthy mothers and newborns - between 0 and 29% as very poor, from 30 to 49%poor, from 50 to 89% good and from 90 to 100% very good.22
The educational workshops carried out during the prenatal care are considered strategies for the practice of health promotion and are characterized by a group of people who interact with the objective of expanding their knowledge and abilities, propitiating the development of their autonomy.17
The nursing professional is an important agent of transformative actions aimed at the promotion, encouragement, and support of breastfeeding, besides providing care to pregnant women, the puerperium and the newborn, aiming at the behavioral change of women and support groups.6,11
CONCLUSION
The socioeconomic profile of the women surveyed was characterized, mainly, by the age group from 19 to 24 years old, married, housewife, with a good degree of education, without addictions and with a family income of up to 3 minimum wages. Regarding the gynecological-obstetric profile, primigravidae, with no history of miscarriage, who had more than six prenatal consultations, but only between 1-2 consultations with nurses and no orientation regarding breastfeeding. The predominant way of delivery was vaginal and skin-to-skin contact with the newborn in the first hour of life prevailed, and the opposite occurred with women undergoing a cesarean delivery.
Knowing the characteristics of the ascribed women is fundamental for quality care, especially as referenced in this research; breastfeeding should be stimulated from the prenatal period by the nurse practitioner and extended throughout the pregnancy-puerperal cycle.
The results attested that most of the pregnant women interviewed received no guidance during the prenatal period on breastfeeding or the benefits of skin-to-skin contact. Such findings should be considered, considering that the research was composed of young pregnant women, timely conditions for health education, lack of knowledge about this phase and insecurity regarding the experience of pregnancy.
Pregnant women who underwent a cesarean section did not have early contact with their children and were not stimulated to breastfeed in the first hour of life. Aggravated by the fact that most of these women were primigravidae, which also becomes a relevant factor for health professionals to sensitize and guide, regardless of the way of delivery.
The lack of follow-up of the duration of breastfeeding for a longer period than the immediate puerperium and the recording of the time in which the newborn remained in skin-to-skin contact is seen as a limitation of the study,
It is suggested that these findings may challenge professionals and institutions in the search for better strategies so that skin-to-skin contact and the initiation of breastfeeding are also performed to the women who undergo the cesarean section procedure.
REFERENCES
1.Ministério da Saúde (Br). Atenção ao pré-natal de baixo risco. Brasília (DF): Ministério da Saúde; 2013.
2.Cruz SH, Germano JA, Tomasi E, Facchini LA, Piccini RX, Thumé E. Orientações sobre amamentação: a vantagem do Programa de Saúde da Família em municípios gaúchos com mais de 100.000 habitantes no âmbito do PROESF. Rev. bras. epidemiol. 2010; 13 (2): 259-67.
3.Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Pré-natal e puerpério: atenção qualificada e humanizada. Brasília (DF): Ministério da Saúde; 2006.
4.Gomes RMT, César JA. Perfil epidemiológico de gestantes e qualidade do pré-natal em unidade básica de saúde em Porto Alegre, Rio Grande do Sul. Rev. Bras. Med. Fam. Comunidade. 2013; 8(27): 9.
5.Ministério da Saúde (Br). Além da sobrevivência: práticas integradas de atenção ao parto, benéficas para a nutrição e a saúde de mães e crianças. Brasília (DF): Ministério da Saúde; 2011.
6.World Health Organization. Indicators for assessing infant and young child feeding practices. Washington (DC) WHO; 2008.
7.World Health Organization. Baby friendly hospital initiative, revised, updated and expanded for integrate care, Washington (DC): UNICEF and Wellstart International; 2006.
8.Barbosa V, Orlandi FS, Dupas G, Beretta MIR, Fabbro MRC. Aleitamento materno na sala de parto: a vivência da puérpera. Cienc. cuid. saude. 2010; 9 (2): 366-73.
9.Ministério da Saúde (Br). Iniciativa Hospital Amigo da Criança. Brasília (DF): Ministério da Saúde; 2010.
10.Marques ES, Cotta RMM, Priore SE. Mitos e crenças sobre aleitamento materno. Ciênc. & saúde coletiva (Online). 2011; 16 (5): 2461-8.
11.World Health Organization. Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services – the revised Baby-friendly Hospital Initiative. Geneva, (Swi): WHO; 2018.
12.Dodt RCM, Oriá MOB, Pinheiro AKB, Almeida PC, Ximenes LB. Perfil epidemiológico das puérperas assistidas em um alojamento conjunto. Rev. enferm. UERJ. 2010; 18 (3): 345-51.
13.Ministério da Saúde (Br). Pesquisa Nacional de Demografia e Saúde da Criança e da Mulher: dimensões do processo reprodutivo e da saúde da criança. Brasília (DF): Ministério da Saúde; 2009.
14.Ministério da Saúde (Br). Resultados preliminares da pesquisa de satisfação com mulheres puérperas atendidas no SUS. Brasília (DF): Ministério da Saúde; 2013.
15.Wenzel D, Souza SB. Fatores associados ao aleitamento materno nas diferentes regiões do Brasil. Rev. Bras. Saúde Matern. Infant. 2014; 14 (3): 241-9.
16.Onah S, Donatus ICO, Ebenebel J, Ezechukwu C, Ekwochi U, Ndukwu I. Infant feeding practices and maternal socio-demographic factors that influence practice of exclusive breastfeeding among mothers in Nnewi South-East Nigeria: a cross-sectional and analytical study. International Breastfeeding Journal. 2014; 9: 10.
17.Mannion CA, Hobbs AJ, McDonald SW, Tough SC. Maternal perceptions of partner support during. International Breastfeeding Journal. 2013; 8(4):1-7.
18.Lima JP, Cazola LHO, Pícoli RP. A participação do pai no processo de amamentação. CogitareEnferm. 2017; 22(1):01-7.
19.Gonçalves MD, Kowalski ISG, Sá AC. Atenção ao pré-natal de baixo risco: atitudes dos enfermeiros da estratégia saúde da família. Rev. enferm. UERJ. 2016; 24(6): e18736
20.Victora CG, Barros AJD, França GVA, Bahl R, Rollins NC, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet. 2016; 387(010017): 475-90.
21.Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Promovendo o aleitamento materno. álbum seriado. Brasília (DF): Ministério da Saúde; 2007.
22.Esteves TMB, Daumas RP, Oliveira MIC, Andrade CAF, Leite IC. Factors associated to breastfeeding in the first hour of life: systematic review. Rev Saúde Pública. 2014; 48 (4): 697-708.
23.Romão P, Durão F, Valente S, Saldanha J. Aleitamento materno: o que mudou em 12 anos. Nascer e Crescer – Birthand Growth Medical Journal 2017; 26(3): 171-7.
24.Sampaio ARR, Bousquat A, Barros C. Contato pele a pele ao nascer: um desafio para a promoção do aleitamento materno em maternidade pública no nordeste brasileiro com o título de Hospital Amigo da Criança. Epidemiol. Serv. Saude. 2016; 25(2):281-90.