(*) Test calculated without taking into account Gynaecology and Mastology;
(**)Mann-Whitney test;
(***) Chi-square;
(****) Fisher-Freeman-Halton.
ORIGINAL RESEARCH
Nursing diagnoses of impaired urinary elimination in hospitalized, post-operative elderly: a cross-sectional study
Graziele Ribeiro BitencourtI; Nathalia Henrique Martins Dessimone FelippeII; Rosimere Ferreira SantanaIII
I
Nurse. Master. Member of the Study Group on Standardization of Nursing
Care, Fluminense Federal University. Niterói, State of Rio de Janeiro,
Brazil. Email: gra_uff@yahoo.com.br
II
Nurse. Member of the Study and Research Center on Systematization of
Nursing Care. Fluminense Federal University. Niterói, State of Rio de
Janeiro, Brazil. Email: nathaliamartins@id.uff.br
III
Nurse. PhD in Nursing. Associate Professor of the Fluminense Federal
University. Niterói, State of Rio de Janeiro, Brazil. Email: rosifesa@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.16629
ABSTRACT
Introduction: with the aging process, anatomical and physiological changes are observed in the urinary system, which can be potentiated by surgical procedures and identified by nursing diagnosis. Objective: to examine the nursing diagnosis "impaired urinary elimination" in the elderly postoperative. Method: participants in this quantitative, observational, cross-sectional study were 103 elderly inpatients at Rio de Janeiro University Hospital on the first day after surgery. Data were described as the presence of the firm diagnosis by two experts in gerontological and medical-surgical nursing and analyzed by simple descriptive statistics. Results: most had dysuria (93), nocturia (58) and urinary urgency (34) as the main defining characteristics. Related factors were identified as multiple causes (78) and urinary tract infection (14). Conclusion: the identification of the diagnosis of impaired urinary elimination is necessary in postoperative elderly in order to facilitate early intervention in related factors so as to avoid possible urinary complications.
Keywords: Nursing diagnoses; urinary tract; perioperative nursing; aged.
INTRODUCTION
The aging process may bring physical modifications that increase the risk for clinical complications, morbidity and mortality among the elderly. The urinary system, for example, may show changes such as loss of collagen and damage to bladder contractility, urethral resistance, changes in urinary flow, reduced glomerular filtration rates, differentiated excretion of creatinine, water and salt. As a consequence, increased emergence of genitourinary diseases such as renal failure, infection and urinary incontinence is observed1.
These clinical cases are the leading causes of hospitalization in elderly patients. Urinary infections (28%) are the second leading cause of hospital admissions, behind complications in the respiratory tract (58%)2 . Furthermore, urinary incontinence accounts for the fifth nursing diagnosis in hospitalized elderly patients (6.9%)3.In this context, tools to assist in the investigation of urinary disorders in the elderly become necessary. One of the alternatives is to identify the nursing diagnosis of impaired urinary elimination, defined as dysfunction of urine elimination. Defining characteristics, that is, signs and symptoms for this clinical diagnosis: dysuria, frequency, hesitancy, incontinence, nocturia, urinary retention and urgency. In turn, as possible causes, that is, factors associated with the diagnosis: sensorimotor damage, urinary tract infection, multiple causes, anatomical obstruction 4. There is, therefore, a need for early identification of these defining characteristics and intervention on associated factors in order to decrease the risk of urinary complications in the elderly in the postoperative period. Furthermore, although the literature indicate urinary complications as frequent in postoperative moments, the studies found addressing diagnosis of urinary elimination were carried out in the following areas: hemodialysis5; in the presence of diabetes mellitus6, at risk of pressure ulcers7; and urinary incontinence8. However, what is the specific presentation of this nursing diagnosis in the elderly in the postoperative period? Thus, the present study has the following objective: to analyze the nursing diagnosis of impaired urinary elimination in elderly in postoperative period.
LITERATURE REVIEW
The nursing diagnosis is defined as "a clinical evaluation of experiences/responses of an individual, family, group or community towards health problems/real or potential life processes ... [and] provides the basis for the choice of nursing interventions in order to achieve the results that are the responsibility of the nurse"4:1.
The usefulness of the application of nursing diagnosis is the possibility to determine the clarity and assertiveness in the conduct of care outlined by the nursing staff, as well as communication with other team members on its multi and interdisciplinary approach9. For this, its development requires data collection, physical examination and clinical reasoning with technical and scientific basis of anatomy, physiology, pathophysiology and a diagnostic classification system.
In this context, this analysis in the elderly require special attention due to changes resulting from the aging process and the presence of associated diseases that can compromise the functional balance and change the physiological functioning10. This aspect associated with increased vulnerability caused by surgical conditions make the analysis of nursing diagnoses in this clientele even more specific in order to reduce postoperative complications.
Urinary changes, in this sense, may be related to changes that are typical of the aging process such as weakening of bladder muscles, changes in prostate and kidney function. They may be also related to the conditions of the postoperative period which involve urinary catheterization, urologic surgical approach, fluid restriction and anesthesia11.
METHODOLOGY
The study presents a quantitative, cross-sectional and observational approach. Data collection occurred in the period of September through October 2013, in the wards of male and female surgical clinics of a university hospital located in Niterói, Rio de Janeiro.
The sampling was by convenience and non-probabilistic, and gathered 103 subjects, that is, individuals over 65 years old, of both sexes, on the first day after surgery.
Sampling was stratified according to the eight types of surgeries most commonly performed in the institution surgery: General (35%), Urological (18%), Orthopedic (15%), Mastology (10%), Gynecologic (9%), Vascular (7% ), Thoracic (3%) and Neurosurgery (3%). A subsample was calculated for each stratum considering a confidence level of 90%, absolute sampling error of 5% and the correction for finite populations. The sample was initially calculated in 291 patients. However, due to limitations of time for data collection, that were two months, the final sample consisted of a total of 103 patients stratified as follows: General (21), Urologic (24) Orthopedic (18), Mastology (12 ) Vascular (9), Gynecological (7), Thoracic (7) and Neurosurgery (5). For a punctual sample, the average sampling error would increase to 0.43. However, since each subject was evaluated by two experts in medical-surgical nursing and gerontology to increase the reliability of the data, a total of 206 observations were realized.
In order to increase reliability and parity in the data analysis, experts were trained in the following steps:
After the data collection phase, the defining characteristics and the related factors were transcribed in a table and sent to a statistician. Data were subjected to statistical treatment using absolute and percentage distribution of the frequency and the findings were discussed.
It is noteworthy that the study is in accordance with Resolution nº 466/12, Research Ethics of the Faculty of Medicine/University Hospital Antônio Pedro nº 304/11 and that participation depended on participants , or their legal representatives, signing the Informed Consent (IC ).
RESULTS
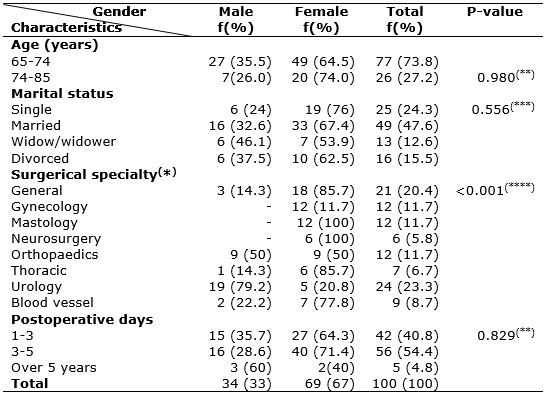
In order to characterize the subjects investigated in the present study, the following variables are presented: age, gender (male and female), surgical specialty and presence of nursing diagnosis of preoperative impaired urinary elimination , presented in Table 1.
TABLE 1: Distribution of elderly subjects in postoperative impaired urinary
elimination. Niterói, RJ, 2013. (N = 103).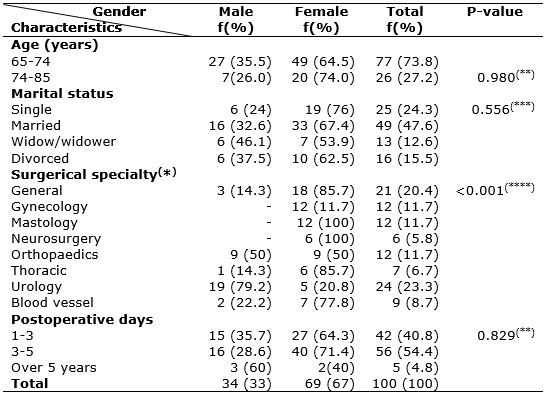
(*)
Test calculated without taking into account Gynaecology and Mastology;
(**)Mann-Whitney test;
(***)
Chi-square;
(****)
Fisher-Freeman-Halton.
Among the 103 elderly, it is observed that the majority - 69 (67%) - are female; 77 (73.8%) were aged between 65 and 74 years; 49 (47.6%) were married; and 24 (23.3%) were undergoing treatment for urological surgery. It is noteworthy that 56 (54.4%) subjects were in the third to fifth day of the postoperative period.
Regarding the differences in percentage identified between the sexes, the significant surgical specialty (p <0.0013) with women in general surgery - 18 (85.7%), and men of urologic surgery - 19 (79.2%), stood out.
All 103 patients in the study retained or developed the nursing diagnosis of postoperative impaired urinary elimination, whose defining characteristics and related factors are detailed in Table 2.
TABLE 2:
Distribution of the nursing diagnosis of Postoperative Impaired Urinary
Elimination/IUE in elderly . Niterói, RJ, 2013. (N = 103)
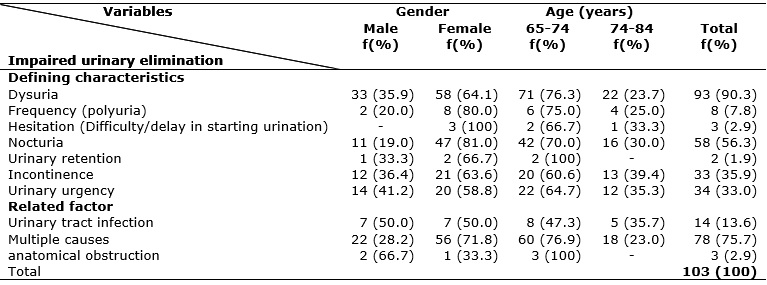
Dysuria was the most obvious defining characteristic, in 93 (90.3%) of the elderly patients that shared in the study, in both sexes and age groups. As a related factor, most participants - 78 (75.7%) - had multiple causes associated with the use of anesthetics and/or conditions after surgery such as immobility and fluid restriction.
DISCUSSION
The changes brought about by the aging process and the surgical procedure interfered both in the characterization of the subjects and in the nursing diagnosis of impaired urinary elimination investigated in the study.
The profile of the elderly was predominated by women, which corroborates the feminization of the aging process. The increasing proportion of women in the old age stands out as a typical characteristics in the Brazilian population. In 2000, for a group of 100 women, there were about 80 men; by 2050, there will be approximately 76.3 men. This phenomenon is accentuated among the elderly over 80 years, reaching 61 men for every 100 women and reaching the proportion of nearly two women for every man13.
The predominance of the age group between 65 and 74 years confirms the findings of previous studies14. The same is not true as to marital status. Married was the most common status in this study and this may not reflect the demographic findings in Brazil, in which aging is linked to widowhood, especially among women13.
Regarding the predominance of urological surgical specialty, recent studies on this subject were absent, despite its importance. However, it can be inferred that, because this is about urinary elimination analysis, it was expected that the presence of this nursing diagnosis were common in urological surgery , since the urinary system is directly affected by this type of surgery.
Aging can modify the ability of storage, increase vesical irritability and may cause contractions during filling and emptying of the bladder. These changes can lead to problems such as variation in the frequency of urination, urinary retention and urinary urgency, besides nocturia, defining characteristics of the diagnosis under study6.
Concerning changes in urinary frequency, polyuria can be seen in diabetes Insipidus and mellitus, which is aggravated by the use of anesthetics in the intraoperative moment. Increased production of vasopressin observed in some people over 65 years of age may also increase the production of urine, as well as the loss of muscle tone and storage capacity observed in cases of diabetes Insipidus 15.
On the other hand, oliguria can be observed due to potential medical complications of the surgical procedure, such as urinary retention, which is one defining characteristic of the diagnostic under study16 In the present study, possibly because patients were already on wards and with decreased anesthetic effects, urinary retention was not numerically significant.
This is a frequent condition in the post-anesthetic recovery room defined as incomplete emptying of the bladder, inability or failure to complete bladder emptying16. It is characterized by bladder volume equal to or greater than 600 mL associated with inability to perform spontaneous urination to 30 minutes17.
Modifications of the aging process, as well as the residual action of anesthetic medications, can cause urinary retention. Decreased fluid intake, use of multiple drugs in these patients, weakening of the pelvic floor, reduced bladder capacity, failure of the detrusor muscle and urinary tract infection, were also observed8.
Urinary urgency, that is, sudden and compelling desire to urinate that is difficult to inhibit18 can be identified as one of the main defining characteristics, and classified as a type of urinary incontinence. This can be defined as involuntary urine loss, related to bladder emptying19. This consists of specific attributes, including place, time, location and style of urination, influenced by the physical and social environments. Because it is one geriatric syndrome, that is, a group of clinical cases of greater attention in elderly patients20, this stresses the need for research in the postoperative period.
Studies also point nocturia as a type of urinary incontinence. This is defined as nocturnal awakenings after beginning resting21, represented by decreased bladder capacity and/or increased urine production at night. This can be associated with common chronic diseases in the elderly such as diabetes, hypertension, sleep apnea and chronic kidney disease22 .
Benign prostatic hyperplasia, vaginal trophism and the presence of distopias can lead to changes in the lower urinary tract such as detrusor instability and shortening of the passage of urine through the urethra. Involuntary contractions of the bladder muscle and post-urination residual volume can also increase with age and affect these characteristics23.Dysuria may also occur in other post-operative complications such as urinary retention, infection and urinary incontinence24. Surgical conditions, particularly gynecological and urological conditions due to edema or local inflammatory process, may lead to incomplete emptying of the bladder and urinary retention. Furthermore, in the first days of catheter removal, which is used in the postoperative period, trauma or excessive enlargement of the urethra may happen25.
In the case of urinary hesitancy, considered as difficulty to expel the first jet of urine, this can be analyzed with base in the delay to start urination due to obstruction or problems on peristalsis. Prostate problems (prostate cancer and benign prostatic hyperplasia) in men and the weakening of the pelvic floor muscles in women typical of the elderly can lead to increased urinary output delay26. This can also be caused by certain conditions related to the hospitalization process in the postoperative period such as removal of indwelling catheters.
Factors related to development of impaired urinary elimination can also be associated with the aging process and the surgical procedure. Multiple causes can be inferred, as they are one of the main factors identified. Age, birth numbers, decreased estrogen levels in menopause, and prostate cancer treatment can interfere with urinary elimination27.Furthermore, in the postoperative period, conditions such as the restriction in the bed, pain and reduction of tonicity of the bladder, fear, shame to use containers for disposal of urine different from what is found in the household, are all factors that may impair the spontaneous elimination of urine in the elderly and may reflect the related factor under discussion. If maneuvers of spontaneous stimulation are not successful, intermittent or indwelling catheterization can be used. However, this can lead to other complications such as infection or urinary retention after its removal. Some variables can also aggravate the situation. These include gender, physical condition, part of the body affected by the surgery, type of anesthesia, surgical and anesthetic times, use or not of opioids, volume of fluids administered, previous history of urinary symptoms, and conditions that suggest systematic evaluation of the urinary volume in the postoperative period17.
In hospitalized elderly, the use of diapers and the lack of stimulus to use the toilet as part of sphincter control therapy are aggravating factors. We recommend the use of diapers for elderly with difficulty to eliminate urine, such as incontinence or severe mobility restrictions that prevent the aid of utensils as "bedpan" and/or "duckling". However, indiscriminate use of diapers occurs even in patients who do not need, which can lead to other complications such as urinary tract infection28,29.
The elderly are at increased risk of infection due to physiological changes caused by aging, reduced functional capacity, and chronic and debilitating conditions. It has even higher incidence in older hospitalized patients, and women over 65 years have the higher rate of hospitalizations due to pyelonephritis than men and younger women30. In these patients, previous infections, use of indwelling bladder catheters, other concomitant diseases, institutionalization and decline in cognitive status are associated with worse prognosis31.Cognitive changes may interfere with the related factor known as sensory motor damage, which refers to the importance of nurses in the early management of neurological and chronic diseases that worsen bladder dysfunction6.Mental and physical disabilities caused by diseases such as Parkinson's disease and previous stroke, in addition to surgical medications, may interfere in the decrease of pelvic muscle tone and nerve damage27. This requires from nursing commitment for its control. These aspects together increase the morbidity and costs of the treatment and early mortality, which increases the need for precision in the analysis of clinical signs and symptoms of factors that can trigger urinary problems.
Moreover, in the hospital, the nurse needs to promote urination in a private place, so as to allow adequate time and provide sensory stimulation for sphincter relaxation and the ability to urinate32. The absence of these conditions increases the risk of urinary problems caused by multiple factors in this study.
CONCLUSION
The profile of urinary elimination of elderly people surveyed showed that most elderly display dysuria and factor related to multiple causes. This data can point to aspects that are inherent of the aging and surgical processes, such as bladder weakness and use of anesthetics, respectively. With these findings, it can be inferred that the postoperative period and the age interfere with the nursing diagnosis under investigation. However, there is a gap in the present study related to the analysis of surgeries to which participants were submitted.
Thus, there is a need for new studies that may indicate the early identification of the reason of defining characteristics and intervention in related factors associated with the age and surgical conditions found, since they can facilitate the reduction of urinary complications in the elderly in post-operative moments.
Also, the importance of developing new studies focused on best practices, whose interventions produce effective results in preventing and reducing complications in elderly in postoperative moments.
REFERENCES
1. Leme LEG, Sitta MC, Toledo M, Henriques SS. orthopedic surgery in the elderly: clinical. Rev bras ortop. 2011;46(3):238-46.
2. Izaias EM, Dellaroza MSG, Rossaneis MA, Belei RA. Cost and characterization of hospital infection in elderly. Ciênc. saúde coletiva.. 2014;19(8):3395-02.
3. Sousa RM, Santana RF, Santo FHE, Almeida JG, Alves LAF. Nursing diagnoses identified in hospitalized elderly. Esc Anna Nery (impr.)2010;14 (4):732-41.
4. Nanda International. Nursing diagnoses NANDA: definitions and classification (2012-2014). Porto Alegre (RS): Artmed; 2013.
5. Biscal MM, Marques IR. Nursing diagnoses profile before starting hemodialysis treatment. Rev Bras Enferm, Brasília 2010; 63(3): 435-9.
6. Teixeira CRS, Nakanish MK, Becker TAC, Zanetti ML, Kusumota L, Landim CAP. Urinary elimination nursing diagnosis impaired in people with diabetes mellitus. Rev Bras Enferm. 2010;63(6):908-12.
7. Lucena AF, Santos CT, Pereira AGS, Almeida MA, Dias VLM, Friedrich MA. Clinical profile and nursing diagnosis of patients at risk of pressure ulcers. Rev. Latino-Am. Enfermagem. 2011;19(3):523-30.
8. Loureiro LSN, Medeiros ACT, Fernandes MGM, Nóbrega MML. Urinary incontinence in elderly women: determinants, consequences and nursing diagnoses. Rev Rene. 2011;12(2):417-23.
9. Pereira JMV, Cavalcanti ACD, Santana RF, Cassiano KM, Queluci GC, Guimarães TCF. Nursing diagnoses of patients hospitalized with cardiovascular disease. Esc Anna Nery. 2011; 15(4):737-45.
10. Bitencourt GR, Santana RF, Cavalcanti ACD, Cassiano, KM. Comparison of nursing diagnoses in adults and elderly hospitalized in the post-operative Rev Eletr Enf. 2011;13(4):604-11.
11. Bitencourt, GR, Santana, RF. Conceptual validation of the nursing outcome urinary elimination in elderly surgical. In NANDA International 2012 Conference; 2012 mai. 12-15; Texas, Estados Unidos: Nanda/USA;2012.
12. Carpenito-Moyet LJ. Nursing diagnosis: application to clinical practice. Porto Alegre (RS): Artmed; 2012.
13. Porciúncula RCR, CarvalhoEF, Barreto KML, Leite VMM. Socioepidemiológico profile and autonomy of the oldest in Recife, Nordeste do Brasil. Rev Bras Geriatr Gerontol. 2014; 17(2):315-325.
14. Campolina AG, Adami F, Santos JLF, Lebrão ML. The transition of health and changes in healthy life expectancy of the elderly: possible impacts of chronic disease prevention. 2013;29(6):1217-29.
15. Saletti D, Grigio TR, Tonelli D, Ribeiro OD, Marini F. Anesthesia in a patient with asphyxiating thoracic dystrophy: Jeune syndrome. Rev Bras Anestesiol. 2012;62(3):424-31.
16. Negro CL.A, Muir GH. Chronic urinary retention in men; how we define it, and how does it affect treatment outcomes. BJU Int. 2012;10(11):1590-4.
17. Mago AJD, Helayel PE, Bianchini E, Kozuki H, Oliveira Filho GR. Prevalence and predictors of urinary retention diagnosed by ultrasound in the immediate post-anesthetic. Rev Bras Anestesiol. 2010;60(4):387-90.
18. Jerez-roig J, Souza DLB, Lima KC. Urinary incontinence in institutionalized elderly in Brazil: an integrative review. Rev bras geriatr gerontol. 2013; 16(4):865-79.
19. Honório, MO, Santos SMA. Urinary incontinence and aging: impact on daily life and quality of life. Rev Bras Enferm. 2009; 62(1):51-6.
20. Liberalesso NA, Sanches YM, Araújo LF, Carmo EM, Cabral BE, Siqueira MEC. Methodology and sociodemographic profile, cognitive and fragility of community nursing seven Brazilian cities: FIBRA Study. Cad Saúde. 2013; 29(4):778-92.
21. Moccellin AS, Rett MT, Driusso P. Urinary incontinence during pregnancy: implications for quality of life. Rev. Bras. Saude Mater. Infant. 2014; 14(2): 147-54.
22. Faria CA, Menezes AMN, Rodrigues AO, Ferreira ALV, Bolsas CN. Urinary incontinence and nocturia: prevalence and impact on quality of life in elderly women in a Basic Health Unit . Rev bras geriatr gerontol. 2014; 17(1):17-25.
23. Silva VA, D'Elboux MJ. Nurses' performance in the management of urinary incontinence in the elderly: an integrative review. Rev esc enferm USP. 2012; 46(5):1221-26.
24. Poveda VB, Alves JS, Santos EF, Moreira AGE. Nursing diagnoses in patients undergoing hemodialysis. Enfermeria Global. 2014; 13(2):58-69.
25. Conterno LO, Lobo JA, Masson W. Excessive use of urinary catheters in hospitalized patients in university hospital wards. Rev esc enferm USP. 2011; 45(5):1089-96.
26. Torricelli FCM, Mazzucchi E, Danilovic A, Coelho RF, Srougi M. Surgical treatment of bladder lithiasis: literature review. Rev Col Bras Cir. 2013; 40(3): 227-33.
27. Alencar DL, Marques APO, Leal MCC, Vieira JCM. Factors that influence the sexuality of the elderly: an integrative review. Ciênc saúde coletiva. 2014; 19(8):3533-42.
28. Alves LAF, Santana RF. nursing staff perceptions about the use of adult diapers in hospital. Cienc Cuid Saude. 2013; 12(1):19-25.
29. Alves LAF, Santana RF. Nursing perceptions about the use of diapers during hospitalization. Rev enferm UERJ. 2014; 22(3):371-75.
30. Rowe TA, Mehta MJ. Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin North Am. 2014; 28(1):75-9.
31. Nogueira PSF, Moura ERF, Costa MMF, Monteiro WMS, Brondi L. Profile of nosocomial infection in a university hospital. Rev enferm UERJ. 2009; 17(1):96-101.
32. Fumincelli L, Mazzo A, Silva AAT, Pereira BJC, Mendes IAC. Scientific production on urinary elimination in Brazilian nursing journals. Acta Paul Enferm. 2011; 24(1):127-31.