 Source: Science Direct, Lilacs and Medline
Source: Science Direct, Lilacs and Medline FIGURE 1: Identification of articles selected for the study.
REVIEW ARTICLES
HIV testing in the context of public policy: proposal and reality
Elis Oliveira ArantesI; Rosângela da Silva SantosII
I
Masters student in Nursing from the State University of Rio de Janeiro. School of Nursing, Rio de Janeiro, Brazil. Email: elisarantes@outlook.com
II
Adjunct professor at the State University of Rio de Janeiro. School of nursing, Maternal and child health Department. Rio de Janeiro, Brazil,
Representative of the area of nursing in the Nursing Advisory Council of the National Research Council. Email: rosangelaufrj@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.16366
ABSTRACT
This integrative review study, conducted in Rio de Janeiro, examined the healthcare-related scientific production regarding implementation of Human Immunodeficiency Virus (HIV) testing in the context of public health policies. Of the four articles selected in this study, only one discussed HIV testing from the public policy perspective. The remaining articles addressed HIV testing in primary care without, however, mentioning policy guidelines. This shows that, although there are public policies providing for health care actions in relation to HIV testing, not only are they not being discussed, they are not implemented in health services.
Keywords: HIV; women; nursing care; primary health care.
INTRODUCTION
Acquired immunodeficiency syndrome (AIDS) is configured as one of the major public health problems in Brazil and in the world due to its chronic and evolving pandemic character, which affects over 35 million people worldwide, of which 2.1 million were infected in 20131. Of this total, 17.6 million are women of reproductive age, representing more than 50% of all the adults infected1,2. Only in Latin America are there 550 thousand women infected with the human immunodeficiency virus (HIV), being Brazil responsible for 230,161 thousand of these HIV-positive women1.
The Ministry of health in 2004, adopted as a prevention and control strategy of the HIV infection, early access to HIV testing in addition to the Anonymous Testing centers (ATC), including basic health units (BHU), and should be offered to the whole population which is vulnerable to infection, for example, cases of sexually transmitted Infections (STI)3-9. Such a measure is justified by the fact that the transmission rate be 3.5 times higher in the Group of people who are unaware of their HIV serology7.
For the population, early diagnosis makes it possible to break the chain of HIV transmission and promotes the institution of early treatment which enables higher quality of life for people with HIV and, consequently, lower morbidity and mortality caused by AIDS. For public healthcare, timely diagnosis reduces the cost related to the co-morbidities of HIV infection and prevents the transmission of this virus to seronegative people2,9,10,11.
However, despite the decentralization of HIV testing and the incentive for testing in the general population, women who do not experience the obstetrical period are still on the fringe of early diagnosis, even with the doubling of the number of HIV tests and distributed paid by SUS, which went from 3.3 million to 6.3 million units2.
Therefore, reflect on the policy of expansion and decentralization of access to HIV testing it is necessary, since the women sexually active and outside the gestational period, still has a reduced access to counseling and diagnostic actions for HIV infection in the BHU. This l low coverage increases vulnerability and injuries related to infection, since, late diagnosis, postpones the educational and treatment actions aimed at providing quality of life for people with HIV and consequently reduce morbidity and mortality9,12,13.
The professional nursing has legal and ethical support for that, when properly trained and qualified in accordance with the rules of the Ministry of health, collecting, reading and recording the outcome of the qick HIV test14. Moreover, inserted in the family health program (FHP), these professionals create links with the population, which favors the realization of pre-and post-test counseling, as well as greater opportunity to Institute sex education, family planning and comprehensive assistance to all of the women's life cycles3.
This research will provide subsidies for new studies and interventions in the field of women's health, specifically with respect to nursing care, to care related to women's health are legitimate in all life cycles and thus be possible to give visibility to women who did not experience the time of pregnancy.
To this end, this study used the method of integrative review in order to identify whether the scientific production follows the recommendations provided for HIV testing. To guide the integrative review, the following guiding question was formulated: Is the HIV test made available for women outside of pregnancy during the gynecological examination at the BHU? The objective was to analyze the scientific production of the health area in relation to the HIV test, in the perspective of public health policies.
METHODOLOGY
This study used the integrative review method, including in-depth analysis of relevant research, systematic synthesize, and ordered the results of several studies about a particular subject15. It used a data collection form as a research technique designed by the authors containing closed ended questions.
The construction of this integrative review contemplated the six phases: selection method proposed in the guiding question, selection of research constitute the sample of the study, representation of the characteristics of the research reviewed; analysis of the findings according to the inclusion and exclusion criteria established, interpretation and dissemination of the results16,17.
The criteria for inclusion of articles selected were addressing the HIV test; full text available in the Virtual Health Library (VHL) and Science Direct and year of publication from 2004 to 2013, during which shall enter into force the policy of expansion and decentralization of HIV testing in the BHU. The exclusion criterion was addressed in the gestational period.
The articles search occurred in the months of November and December 2014 in the VHL using the keywords: HIV, women and nursing. At first, each descriptor was used individually, without adopting filter and subsequently with the filters: full text available and year of publication-2004 to 2013. Then, we used the same descriptors, however, combined, first without use of filters and then, with them.
In the Science Direct survey, the same keywords were adopted, however, in the English language: HIV; women e nursing and with the same filters: full text available and year of publication from 2004 to 2013. Each descriptor was used individually, without adopting a filter and subsequently with filter. Then, we used the same descriptors, however, combined, first without use of filters and then, with them.
By combining the descriptors and use filters, referred to the following amount: 90 articles in Science Direct; 46 articles in Lilacs; 24 articles in Medline and 11 articles in Scielo. When performing the reading in full of these texts, only four defined the final sample of this review: two in Science Direct, one in Medline and a in the Lilacs.
For critical evaluation the reading in full of these studies and the results, in order to identify relevant aspects that were repeated or stood out. Afterwards, the articles were identified by numbers, according to location order and were cataloged and the data adapted and organized as follows: title, authors, formation, year, country, language, and periodical, level of evidence, objectives, participants, results and conclusions.
The results were discussed in the light of the relevant literature on the theme 3-5,9-14,18-30.
RESULTS AND DISCUSSION
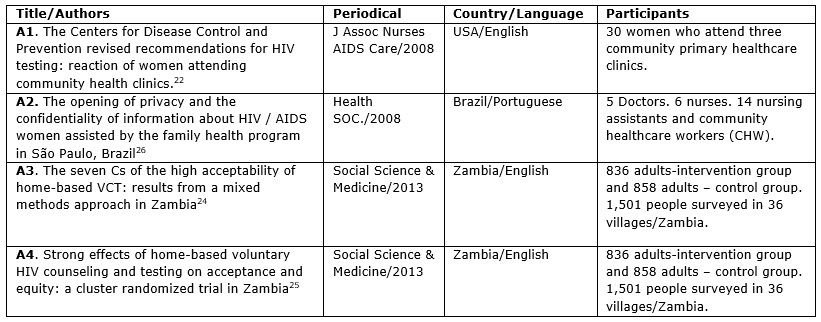
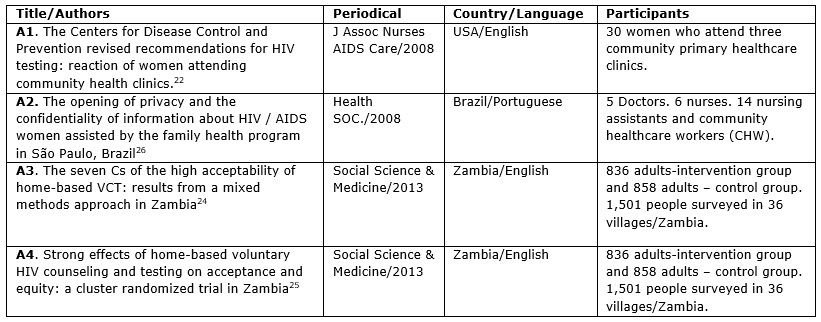
In relation to the characterization of the four selected, two articles were published in 2008 (A1 and A2)22,26and the other two (A3 and A4) 24,25in 2013. Only one was from Brazilian research (A2)26, two from the African continent (A3 and A4)24,25 and an American (A1)22. The schooling of the authors, one of the articles (A1)22had the nursing professionals and researchers from medicine, other (A2)26nursing professionals and only two articles (A3 and A4)24,25were medical professional researchers. See Figure 1.
 Source: Science Direct, Lilacs and Medline
Source: Science Direct, Lilacs and Medline
FIGURE 1: Identification of articles selected for the study.
Article A122 checked the perceptions of women attending basic health units in relation to new recommendations for HIV testing in the United States. Article A226 emphasized the issues of confidentiality of diagnosis in the FHP assistance; A3 check the reasons why the high acceptance of the HIV test when performed at home and25A4, which consisted of an offshoot article A324, sought to assess the question of access and the negative effects of HIV test at home.
The evaluation of the quality of scientific evidence on the issue in studies aimed to determine the reliability of the studies using the results and strengthen the conclusions that will generate the state of current knowledge about the research theme. Thus, an article was classified as level of evidence I (A4)25, randomized clinical trial and the other three (A122, A226 e A324), were classified as evidence level IV, for using the qualitative descriptive method17.
Article A425addresses the achievement of HIV counseling and testing in women together with their partners and point for acceptance of the testing. According to the women in the study, the partner's involvement in testing the free responsibility to reveal the diagnosis and recruit their husbands to do so, as indicated by the healthcare provider.
It is worth revisiting the stigma and prejudice are related to infection from the beginning of the epidemic that spread rapidly around the world and knew little about it. Until 1984, four years after the first case of HIV infection in the world, AIDS became known as Gay Plague and linked to so-called risk groups such as homosexuals, hemophiliacs, sex workers and intravenous drug users18. The urgency of response to the epidemic, the little knowledge related to it and the concentration of cases transgressors of the morality of society generated moralistic policies that spread and perpetuated the prejudice and stigma to HIV19,20.
The HIV infection in Brazil and in the world showed social, economic and cultural contradictions, which challenged the search for answers and for the establishment of health policies to control the epidemic21,22. The lack of knowledge about this new epidemic that affected the world in 1980 brought as consequences prejudice and stigma that still perpetuate about HIV and constitute in important barriers to the implementation of public policies for the infection19.
Despite these Brazilian policies represent a level of excellence and have, many of them international recognition, still present major challenges in its execution19.22. That's what happens with policies and programs about the HIV test that are quite limited, due to the various factors that influence the decision to accept or not the test, by suffering still influences biased and exclusionary measures adopted at the beginning of the epidemic.
Moreover, when these policies are aimed at women the challenges are even greater for decades since women were only seen to have children without the right to experiencing sexuality the way they wished, as they fell upon gender issues21. Even with government programs ensuring sexual and reproductive rights of women and the National Policy for Integral Attention to Women's Health in 2004, the remaining public policies prioritize the female population only during pregnancy, especially with regard to HIV3.
In early 2000, the Brazilian public policies began the process of expansion of HIV testing in addition to the Testing and Counseling Centers (TCC) by introducing them in BHU, regardless of pre-natal consultations. The measure gained momentum with the AIDS III Project and the Campaign Knowing that, among other objectives, noted the increase in access to early diagnosis of HIV and improve the quality of attention to STD/AIDS19,22.
In 2004, the Brazilian Government made the offer of quick test for HIV, the BHU, for the population in General, in order to expand and decentralize HIV test, which were concentrated in the TCC and from that, only for pregnant women21. As well as Brazil, the United States also proposed the expansion of HIV testing for the general population, but only from 200622. The proposal brought the end of the pre-and post-test counseling service, the end of the written consent for HIV testing, and the test for the population between the ages of 13 to 69 years23.24.
However, many times, that the HIV test is being performed only during pregnancy and without compulsory pre-and post-test counseling, without that the women know that the exam is for HIV serology25-27. The frivolity of the HIV testing, prenatal consultations, demonstrates that health professionals are more concerned to comply with protocols and targets than to ensure the health and life of mother and child24-26.
The concern to know the opinion of women about how and when it should be carried out HIV testing is notorious in scientific production. However, professional practice this concern, autonomy and evidence are not given to women so that they make informed choices relative to accept or not to perform the anti-HIV test in any of their life cycle22-26. Health professionals still work with the concept of risk groups and, in particular, incorporate gender issues, distancing the women who fall outside these groups of educational and preventive health actions28-30.
The scientific literature examined showed that the HIV test, when done at home, provides women greater reliability on professional secrecy in relation to diagnosis. The fact that one goes to the BHU to be tested for HIV, regardless of the diagnosis, already predisposes themselves to the stigma and discrimination, as a woman in the study people's eyes can kill you25. Furthermore, the test offered at home has the potential to reduce social differences and gender inequalities in access to HIV testing that arose due to the increase of pregnant women tested for HIV22,.25.
Another point highlighted is that health professionals included in the FHP recognizes the important role of the community health agents inserted into the community and, therefore, recognize women in situations of risk for HIV. Therefore, discuss the importance of early diagnosis among team members is essential, so that together, would facilitate access to HIV testing and chart a plan of care for the HIV-positive26.
The realization of counseling and HIV testing in women together with its partners was a positive aspect for acceptance testing by women, according to the analyzed scientific production24,25. According to the women, be tested at home and together with its partners reduce the responsibility that they are not the only ones who know their HIV status for HIV and disclaim recruit partners to the test24.
CONCLUSION
In relation to the four articles selected in this study, only one article discusses the HIV test from the perspective of public policy. Other articles discuss the HIV test on basic care, however, not to mention the political guidelines14,15,16,18. This fact shows that although there are public policies that establish the actions of care in relation to the HIV test, these not being discussed, are not implemented in the health services.
Even with the expansion policy and decentralization of HIV testing for the general population, women who do not experience nor wish to experience pregnancy remain invisible when it comes to early diagnosis of HIV. Therefore, health professionals inserted into BHU even direct tests only towards pre-natal consultations and outdated risk groups, which perpetuates the stigma and prejudice related to HIV testing.
It is obvious that just as in practice of BHU, the scientific literature reviewed stresses the HIV tests only for prenatal appointments, without any mention of the offer of these tests in the gynecological consultation.
It is necessary to address the HIV test in gynecological consultations and highlight the national policy of expansion of the HIV test, as it is a right to citizenship, access to public health services and the early knowledge of serology for HIV. It is necessary that professional practice, concerning HIV testing in women, no matter fully and fairly, without conditioning it only to pregnancy.
REFERENCES
1.United Nations Programme On HIV/AIDS. 2014 report on the global HIV/AIDS epidemic: 4th global report. Geneva: UNAIDS, 2014. [cited in 2015 July 10] Disponível em: http://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2014/july/2010716prgapreport .
2.Ministério da Saúde (Br). Secretaria de Assistência à Saúde. Boletim Epidemiológico – Aids e DST. Guia de Vigilância Epidemiológica. Brasília (DF): Ministério da Saúde; 2013.
3.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Departamento de DST, aids e Hepatites Virais. Cadernos de boas práticas em HIV/Aids na Atenção Básica. Brasília (DF): Ministério da Saúde; 2014.
4. Denize Z. Aconselhamento pré e pós-teste anti-HIV na atenção básica: as perspectivas dos profissionais de saúde [dissertação de mestrado]. São Paulo: Universidade de São Paulo; 2012.
5.Araújo CLF, Priscila AS, Gleice KAS, Maíra GPO, Livia SC. A testagem anti-HIV nos serviços de ginecologia do município do Rio de Janeiro. Esc Anna Nery. 2014; 18: 82-9.
6.Mariângela GS, Francisco IB. HIV/aids no Brasil: provimento de prevenção em um sistema descentralizado de saúde. Questões relativas à provisão universal de saúde. GHD-018.
7.Szwarcwald CL, Castilho EA. A epidemia de HIV/AIDS no Brasil: três décadas. Cad Public Health. 2011; 27(suppl 1): 4-5.
8.Ministério da Saúde (Br). Boletim epidemiológico 2013 DST/AIDS. Brasília (DF): Ministério da Saúde; 2013.
9.Alejandra XA. Facilitadores y barreras que enfrentan las personas al tomar el test de ELISA para el diagnóstico del VIH: revisión de la literatura. Rev Chilena Infectol. 2013; 30: 638-43.
10.Pereira BS. Enfrentamento da feminização da epidemia da AIDS. FG Ciência. 2011; 1(1): 1-18.
11.Moreschi C. Mulheres e vulnerabilidade ao HIV/AIDS. Saúde Santa Maria. 2012; 38(2): 85-94.
12.Leonardo GF, Richardson ARS, Ilisdayne TSS, Karla GSS, Francisca FAS. Percepção de mulheres casadas sobre o risco de infecção pelo hiv e o comportamento preventivo. Rev enferm UERJ. 2013; 21: 805-11.
13.Aboim S. Risco e prevenção do HIV/AIDS: uma perspectiva biográfica sobre os comportamentos sexuais em Portugal. Ciênc saúde coletiva. [Scielo- Scientific Electronic Library Online] 2012 [citado em 12 out 2014]. 17:99-112. Disponível em: http://www.scielosp.org/pdf/csc/v17n1/a13v17n1.pdf.
14.Conselho Federal de Enfermagem. Parecer Normativo nº 001/2013. Legislação profissional. Competência do enfermeiro para realizar teste rápido para detecção de HIV, sífilis e outros agravos. [citado em 10 jun 2015] Disponível em: http://novo.portalcofen.gov.br/parecernormativo-no-0012013_18099.html.
15.Mendes KDS, Silveira RCCP, Galvão CM. Revisão Integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto contexto – enferm. 2008; 17: 758-64.
16.Souza MT, Silva MD, Carvalho R. Revisão Integrativa: como é e como fazer. Eisnten. 2010; 8(1): 102-6.
17.Polit DF, Beck CT. Fundamentos de pesquisa em enfermagem: avaliação de evidências para a prática de enfermagem. 7ª ed. Porto Alegre (RS): Artmed; 2011.
18.Cau BM. O estigma do HIV e SIDA e a testagem de infecção pelo HIV entre adolescentes e jovens em Moçambique. Gazeta de População e Saúde. 2014; 3(4): 1-33.
19.Villarinho MV. Políticas públicas de saúde face à epidemia da AIDS e a assistência às pessoas com a doença. Rev Bras Enferm. 2013; 66: 271-7.
20.Rodrigues CS, Perreault M. A feminização do HIV/AIDS sob a perspectiva de mulheres infectadas: uma questão de gênero. In: III Seminário Internacional Enlaçando Sexualidades; 2013 mai 15-17; Salvador, Brasil. Salvador (BA): Universidade do Estado da Bahia; 2013.
21.Ministério da Saúde (Br). Secretaria de Atenção à Saúde Departamento de Ações Programáticas Estratégicas. Política Nacional de Atenção Integral à Saúde da Mulher – Princípios e Diretrizes. Brasília (DF): Editora MS; 2011.
22.Burrage JW, Zimet GD, Cox DS, Cox AD, Mays RM, Fife RS, et al. The Centers for Disease Control and Prevention revised recommendations for HIV testing: reactions of women attending community health clinics. J Assoc Nurses AIDS Care. 2008; 19: 66-74.
23.Pimenta C, Raxach JC, Terto Júnior V, organizadores. Prevenção das DST/AIDS e novos desafios. Rio de Janeiro: Abia; 2010.
24.Jürgensen M, Sandøy IF, Michelo C, Fylkesnes K, Mwangala S, Blystad A. The seven C sof the high acceptability of home-based VCT: Results from a mixed methods approach in Zambia. Social Science & Medicine. 2013; 97: 210-219.
25.Fylkesnes K, Sandøy IF, Jürgensen M, Chipimo PJ, Mwangala S, MicheloC. Strong effects of home-based voluntary HIV counseling and testing on acceptance and equity: A cluster randomized trial in Zambia. Social Science & Medicine. 2013; 86: 9-16.
26.Abdalla FTM, Nichiata LYI. A abertura da privacidade e o sigilo das informações sobre o HIV/Aids das mulheres atendidas pelo Programa Saúde da Família no Município de São Paulo, Brasil. Saúde Soc. 2008; 17(2): 140-52.
27.Feitosa JÁ, Coriolano MWL, Alencar EM, Lima LS. Aconselhamento do pré-teste anti-HIV no pré-natal: percepções da gestante. Rev enferm UERJ. 2010;18: 559-64.
28.Bastos DC, Paiva MS, Carvalho ESS, Rodrigues GRS. Representações sociais da vulnerabilidade de mulheres negras e não negras à infecção pelo HIV/AIDS. Rev enferm UERJ.
2013; 21: 330-6.
29.Galvão MTG, Gouveia AS, Carvalho CML, Costa Ê, Freitas JG, Lima ICV. Temáticas produzidas por portadores de HIV/AIDS em grupo de autoajuda. Rev enferm UERJ. 2011; 19: 299-304.
30.Branheto ACM, Carvalho AMP. Narrativa da mulher, mãe infectada pelo HIV. Saúde & Transformação Social. 2013; 4: 47-52.