ORIGINAL RESEARCH
In-person and telephone monitoring of symptoms in women with breast cancer undergoing chemotherapy
Danielle Copello Vaz I; Carlos Roberto Lyra da Silva II; Roberto Carlos Lyra da Silva III
I
Nurse. Master. Technologist of the palliative care unit. José de Alencar
National Cancer Institute. Brazil. E-mail: dani_copello@hotmail.com
II
Nurse. Post-Doctor. Associate Professor. Federal University of the State of
Rio de Janeiro. Fundamental Nursing Department. Rio de Janeiro, Brazil.
E-mail: profunirio@gmail.com
III
Nurse. PhD. Associate Professor. Federal University of the State of Rio de
Janeiro. Coordinator of the Graduate Program. Rio de Janeiro, Brazil.
E-mail: proflyra@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.15577
ABSTRACT
Objective: to identify the most prevalent symptoms during chemotherapy treatment of women with breast cancer. Method: this quantitative, descriptive, prospective study evaluated 15 women on day of infusion, and then weekly by telephone, between March and December 2014, at a chemotherapy center in Rio de Janeiro. The project was approved by the research ethics committee (opinion number: 544,459 and Certificate of Presentation for Ethical Evaluation: 26054613.5.0000.5285). Result: the most frequent symptoms were altered taste, anxiety, arthralgia, fatigue, inappetence, myalgia and nausea. Conclusion: identification of the symptoms most prevalent at certain times of chemotherapy treatment allows nurses to optimize guidelines on adverse effects. More precise care interventions, considering the various drugs employed and the multiple symptoms, favor adherence to treatment in that they contribute to maintenance of patient wellbeing.
Keywords : Breast neoplasms; drug therapy; drug-related side effects and adverse reactions; nursing.
INTRODUCTION
Adverse reactions associated with chemotherapeutic treatment are related to non-specific cell destruction; the drugs eliminate other fast-growing cells than tumor cells. This action is responsible for the appearance of adverse effects, especially in hematopoietic tissue, germinative tissue, hair follicle and lining epithelium of the gastrointestinal tract 1.
When the symptoms of the adverse reactions to such non-specific drug effect are not properly controlled, they can have an extremely negative impact on the quality of life and daily activities of patients and may interfere with adherence to treatment, consequently affecting compliance with the proposed therapeutic regimen.
Thus, continuous evaluation of the treatment is necessary and extremely important to adopt the best therapeutic conduct. The follow-up and assessment of complications help identifying problems, monitoring the progress of the symptoms, selecting the relevant interventions and analyzing whether prevention and treatment strategies are effective in fact.
Thus, the particularities of the chemotherapeutic treatment that take place with drug administration and the variable time of onset and duration of side effects are usually identified during the routine medical visit or on the day of the infusion of the next chemotherapeutic cycle by the nursing team. Consequently, the patient does not have routine professional guidance during the intervals between applications, when unwanted effects of drugs reach their apex.
Considering the above, this study aimed to identify the most prevalent symptoms in women with breast cancer undergoing chemotherapy with doxorubicin + cyclophosphamide protocol followed by docetaxel, through face-to-face evaluation on the day of infusion of medications, and weekly evaluation by telephone calls.
LITERATURE REVIEW
The nurse can be an active and transformer agent in the follow-up of breast cancer patients as their didactic role may minimize the stigma that this disease represents. Thus, the nursing team actions should not be restricted to technical skills. The ability to interact and relate with patients combined with professional knowledge allows for a more effective and individualized follow-up and promotes the well-being of both women and their families 2.
Thus, the consequences of treatment and the progression of the disease, such as motor and image changes, reduction or loss of labor activity, changes in family dynamics and, especially, change in lifestyle during treatment, will only be thought when experienced. Unless they are previously anticipated by professionals, they will be unknown to the patients. Poor guidance limits the patients' experience only to their momentary reality. Informing and educating women and society on cancer care are necessary to the quality of treatment 3.
In this sense, telephone contact represents a mean of strengthening the bond between the team and the patient. The contact made over the intervals between the dates of infusions and/or routine consultations allows the follow-up to reach another dimension, because the patients can be monitored when symptoms are more intense. Nursing care and follow-up are even more essential when the chemotherapeutic treatment is more difficult. Thus, telephone contact arises as a potential tool for comprehensive care, an effective tool for the restoring of the client's health.
This intervention is useful both to ratify the most important guidelines and to monitor adverse effects of the treatment. Oncology patients weekly followed by telephone unanimously agreed with this practice. One of the reasons for such satisfaction was the direct contact with nurses, which generates greater confidence and control of treatment 4.
The authors of an integrative review concluded that telephone follow-up is effective as strategy for more effective control of blood glucose in diabetic patients, optimizing even the self-control and, therefore, decreasing the chances of complications of the disease 5.
In another study, patients undergoing percutaneous coronary intervention were followed by telephone after hospital discharge. The objectives were to ratify the guidance received during the period of hospitalization, answer questions, encourage self-care and propose changes in the lifestyle of patients, during recovery and also in following moments. As a result, improvements were observed in the maintenance of bond and emotional and social support to patients and their families. As a result, patients themselves felt motivated to perform self-care, reducing the chances of developing coronary artery disease 6.
METHODOLOGY
This is a descriptive and prospective study with quantitative approach. Fifteen women aged over 18 years and with breast cancer, regardless of the disease stage, starting chemotherapy with doxorubicin + cyclophosphamide followed by docetaxel, neoadjuvant or adjuvant, were included in the study. Study participants were randomly selected, respecting the order of arrival in the service with the respective protocol. The survey took place from March to December 2014 at a particular chemotherapy center located in the city of Rio de Janeiro. The project was approved by the Research Ethics Committee of the Federal University of the State of Rio de Janeiro, Opinion number: 544,459 and Certificate of Presentation for Ethical Appreciation: 26054613.5.0000.5285.
The selected participants had adequate communication and understanding skills and a telephone at home or mobile to keep contact with the researchers in order to follow-up the symptoms at home. Patients with low communication and understanding skills, who did not have a telephone at home or mobile, who needed to change the therapeutic regimen due to resistance to antineoplastics, during treatment, or who had some serious drug toxicity and death before the end of treatment were excluded from the study.
The chemotherapy protocol consists of two stages: four applications of doxorubicin + cyclophosphamide followed by four applications of docetaxel, with intervals of 21 days between applications and average length of 5 months, totaling eight cycles of drug administration in an outpatient setting, as each application represents one cycle.
To establish the bond between professional and patient, the researcher conducted the first nursing consultation of all patients. After the clarification of doubts about the treatment, each patient was invited to participate and, when they agreed, they signed two copies of the Informed Consent (IC) form.
In order to better identify the most prevalent symptoms during chemotherapy treatment, the researcher was responsible for the follow-up of the patients in all outpatient chemotherapy cycles and made telephone contact in two moments - on the eighth and fifteenth day after each intravenous application of chemotherapy. Therefore, each patient was evaluated in eight face-to-face consultations and 16 telephone calls, totaling 24 evaluations. Numbers from 1 to 15 were assigned to distinguish each participant preceded by the letter P. Thus, each patient was evaluated in person on the day of the outpatient intravenous application of chemotherapy (D1) and on the eighth day (D8) and eleventh fifth day (D15) after application through a telephone call.
The data obtained were tabulated and analyzed using the software Microsoft Excel Office, 2010 version, calculating absolute frequencies and percentages. The findings were discussed according to the current literature.
RESULTS AND DISCUSSION
Characterization of patients
Fifteen women with breast cancer, submitted to chemotherapy with doxorubicin + cyclophosphamide followed by docetaxel, composed the study sample. One patient was excluded due to toxicity caused by the treatment after the second application of docetaxel, with consequent change of therapeutic protocol.
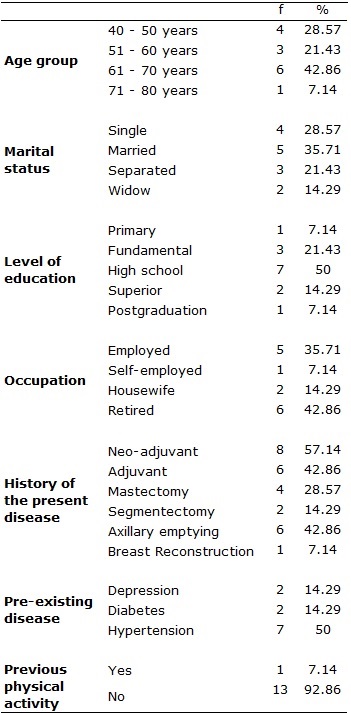
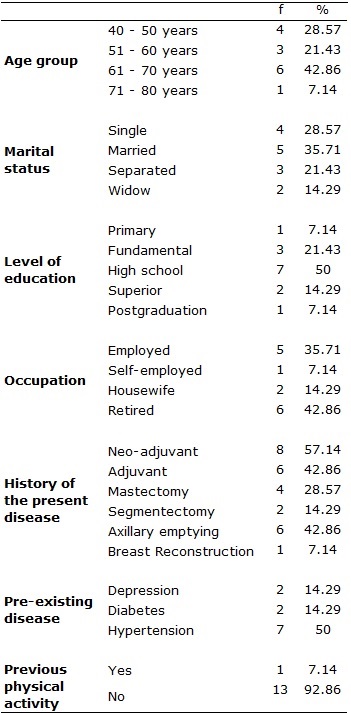
The sample (N = 14) has a mean age of 57.3 years. The analysis of data from the study participants led to the following percentages: married, 5 (35.71%); with complete high school, 7 (50%); retired, 6 (42.86%); with neoadjuvant therapy proposal, 8 (57.14%); with comorbid hypertension, 7 (50%), diabetes, 2 (14.29%), and depression, 2 (14.29%); and without routine practice of physical exercise, 13 (92.86%). Sociodemographic characteristics of participants are presented in Table 1.
TABLE 1
: Sociodemographic and clinical characteristics. Rio de Janeiro,
2014.(N=14)
For better identification of the most prevalent symptoms, each patient was weekly assessed: on the day of outpatient application of chemotherapy (D1); on the eighth day (D8) or one week after intravenous application; and on the fifteenth day (D15) or the second week after application. Therefore, face-to-face evaluations (D1) were carried out with all patients, resulting in a total of 56 evaluations (14 individuals x 4 cycles = 56 evaluations), as the presence of these patients for outpatient application of chemotherapy was mandatory. However, D8 and D15 evaluations did not occur in all times because they were conducted through phone calls and sometimes the patients were not found in their homes or would not answer the phone. Therefore, in the first stage, that is, the administration of doxorubicin + cyclophosphamide, the total number of evaluations on the eighth day (D8) was 51 and on the fifteenth day (D15) was reduced to 47. This means that five patients were not evaluated in D8, and nine patients in D15. Regarding the application of docetaxel, corresponding to the second stage of treatment, 49 evaluations on D8 and 42 evaluations on D15 were conducted. Thus, the symptoms of seven patients were not evaluated in D8, and of 14 patients in D15. Thus, from a total of 336 evaluations (14 women x 24 possible evaluations) to be performed if all telephone contacts were successful, 301 (89.58%) were accomplished and 35 (10.42%) were not. In each stage, the presented percentages were considered as totals (100%) and related to the number of evaluations accomplished, which varied with the difficulties already mentioned.
First stage of chemotherapy treatment
In the first stage of treatment, corresponding to infusion of the drugs doxorubicin + cyclophosphamide, the dominant symptoms on the application of chemotherapy in the clinic (D1) were fatigue, 31 (55.36%), anxiety, 20 (35.71%), taste alteration, 16 (28.57%), and with the same percentage, inappetence and insomnia, 8 (14.28%). Regarding the evaluation of the first week after application of drugs in the clinic (D8), the main symptoms were fatigue, 36 (70.59%); nausea, 30 (58.82%); altered sense of taste, 25 (49.02%); constipation, 21 (41.18%); anxiety, 19 (37.25%); and inappetence and insomnia, 12 (23.53%) each. On the fifteenth day (D15), the most common were fatigue, 28 (59.57%); altered sense of taste, 25 (53.20%); anxiety, 16 (34.04%); inappetence and nausea, 12 (25.53%) each; and insomnia, 11 (23.40%). Table 2 shows the main symptoms reported during all applications of doxorubicin + cyclophosphamide medications.
TABLE 2
: Follow-up of the main symptoms resulting from the infusion of doxorubicin
+ cyclophosphamide in women at three evaluative moments. Rio de Janeiro,
2014
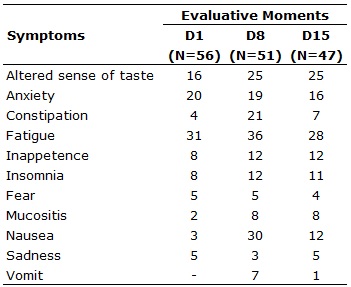
Caption: D1: infusion day; D8: Eighth day after infusion; D15: 15th day
after infusion.
Second stage of chemotherapy treatment
In the second stage, corresponding to the administration of docetaxel, the prevalent symptoms reported on the outpatient application of chemotherapy (D1) were fatigue, 47 (83.93%); altered sense of taste, 34 (60.71%); anxiety, 25 (44.64%); myalgia, 22 (39.28%); inappetence, 21 (37.50%); and arthralgia, 18 (32.14%). On the eighth day (D8), fatigue prevailed, 49 (100%); followed by altered sense of taste, 41 (83.64%); arthralgia, 38 (77.55%); myalgia, 38 (77.55%); anxiety, 32 (65.31%); and inappetence, 31 (63.26%). The evaluations on the fifteenth day (D15) revealed the following symptoms: fatigue, palate alteration, myalgia, arthralgia, inappetence, and anxiety, 21 (50%). Table 3 shows the list of main symptoms reported throughout the administration of docetaxel.
Table 3
: Follow-up of the main symptoms resulting from the infusion of docetaxel
in women at three evaluative moments. Rio de Janeiro, 2014
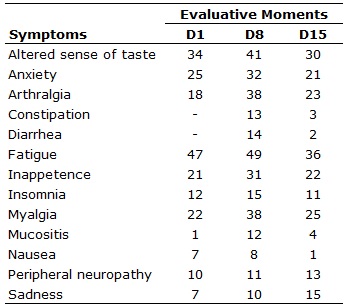
Caption: D1: infusion day; D8: Eighth day after infusion; D15: 15th day
after infusion.
Symptoms during treatment
Among the symptoms presented, fatigue was the most prevalent in both phases of treatment. In the first stage, the symptom occurred with less severity and the patients were able to recover until the next infusion of chemotherapy. In the second stage of the protocol, this symptom was stronger and more persisting throughout the treatment, with lower rates of recovery for the day of application of the next chemotherapeutic cycle. Higher incidence of the symptom was clear in the D8 evaluation. This result is in agreement with some studies that have pointed out that breast cancer patients undergoing chemotherapy present roller coaster oscillations of fatigue. Fatigue levels are higher during the first week after infusion and then show a reduction before the next application 7,8.
A study in Switzerland evaluated 175 newly diagnosed breast cancer patients and identified fatigue, body tension, impaired work or daily living activities and problems with leisure activities as the most recurrent symptoms. Psychological disorders such as anxiety, anxiety and depression were mentioned to some extent. The domains of pain, well-being and gastrointestinal symptoms were less frequent 9. Thus, these symptoms require supportive care at a higher or lower level depending on the reaction of each patient.
The underdiagnosis of psychic suffering, either in newly diagnosed patients or in the course of chemotherapeutic treatment, is a common mistake. This happens due to factors such as hectic schedule of professionals and the patients' resistance to exposing their anguish10. It was evident that lack of guidance from the nursing staff had a negative effect, contributing to the increase of anxiety and emotional fragility, which may compromise even the postoperative recovery11.
One of the factors that can affect the quality of life of patients is the time between diagnosis and start of treatment. One study found that this time is considerably longer in public than in private institutions, what aggravates recurrent symptoms such as fear and anxiety and negatively impacts the quality of life of patients 12. The present study was conducted in a private clinic; Fear was only eventually reported, probably due to the shorter time to start treatment and due to he established trust between patients and the team. Anxiety, though, proved to be recurrent, as in the above mentioned study.
Besides impacting on physical aspects, chemotherapy also has negative repercussions on cognitive functions. Study with 30 breast cancer patients assessed the cognitive function before, during and after a four-step treatment with doxorubicin and cyclophosphamide, relating it to psychological changes, hemoglobin level, menopause stage and perception of cognitive function. Before starting the treatment, the patients had anxiety, but they were usually not depressed or tired and had high levels of cognitive function. After the end of the four chemotherapy cycles, fatigue and depression levels increased and cognitive function decreased 13.
The same paper reports that difficulties in processing and interpreting visual information and decreased ability to perform manual tasks were experienced after treatment. Even after the control of other effects such as anxiety, depression, fatigue, hemoglobin level and state of menopause, such deficits in cognition remained. Besides the overall negative impact of the treatment on cognitive functions, it was evident that women in premenopausal or transition (perimenopause) stages experienced more dramatic worsening of cognition compared to postmenopausal women 13.
In this study, the most prevalent symptom among patients after fatigue was altered sense of taste, resulting in inappetence. Patients undergoing chemotherapy very often report altered taste. The causes of this symptom are not yet completely understood and its prevalence may vary depending on the type of tumor and chemotherapy regimens. One hypothesis is that drugs have direct effects on the taste buds, destroying them or interfering with their renewal. Another common condition is chemotherapy-induced mucositis. Some cytostatics cross the blood-brain barrier and this may alter the recognition of tastes by the central nervous system. Other justifications could be the oxidative stress and metabolic alteration caused by the antineoplastic drugs 14.
A longitudinal study with 109 patients (67.9% with breast cancer) undergoing chemotherapy assessed the taste alterations before and during treatment and after three months of its completion. The majority of the sample (76.1%) reported the symptom during the study. Furthermore, 26.4% rated it as moderate or severe at least once. The symptom was more acute in older patients and became worse in the course of treatment. Patients treated with the epirubicin, docetaxel and capecitabine suffered higher levels of toxicity regarding the change in the sense of taste. The highly significant association between taste changes with inappetence and fatigue enhances the problem. All these symptoms can lead to cachexia, as well as decreased therapeutic response, increased morbidity, mortality, side effects and length of hospital stay, thus compromising the quality of life 15.
Another study showed that patients undergoing chemotherapy presented decreased olfactory and gustatory sensations throughout the treatment. However, three months after discontinuation of treatment, the total olfactory function was practically restored, while changes in the taste completely disappeared. Among the factors that cause greater or less predominance of symptoms, the main one identified by the study was the chemotherapeutic agent employed. Drugs belonging to the taxane group (e.g., docetaxel) proved to be the most impactful on taste, while olfaction changes did not show significant changes according to the drug administered, but were stronger in older patients. Disorders of the palate were mainly related to savory flavors, while sweet, sour and bitter flavors were less affected, and did not have any relation with age of the patients 16.
In this research, during the first stage of treatment, a few patients claimed to have experienced nausea and vomiting, although in less extent. In the second stage, only nausea was reported but, in any case, with little evidence compared to the other symptoms. Perhaps the reduction of these symptoms is related to the routine use of antiemetics protocoled by the service.
This result differs from a study with 79 women that showed that, despite the fact that patients presented nausea and vomiting at least once during treatment, there was no significant decrease in quality of life. Of the 79 women, 48 received the EC-T (epirubicin, cyclophosphamide and docetaxel) or EC-TH (epirubicin, cyclophosphamide, docetaxel and trastuzumab) protocol and throughout the treatment 349 events were reported, of which 231were nausea and 118, vomiting. Vomiting was predominant in the first five cycles and nausea, until the fourth. Likewise, the 31 patients submitted to the FEC scheme (fluouracil, epirubicin and cyclophosphamide) presented 225 events, 94 of which were vomiting and 131 were nausea with little or no variation throughout the treatment 17.
Another study carried out with 172 cancer patients (gastrointestinal, lung and breast cancer) in the emergency of a public hospital showed pain - 143 (83.1%), nausea and vomiting - 116 (67.4%) and fever - 45 (26.1%) as the main complaint in the admission, and more than one symptom was eventually present in the same patient 18.
Therefore, chemotherapy treatment is experience by patients with emotions and doubts, besides, of course, the various symptoms caused by toxicity. These symptoms allied with concerns brought about by the physic-chemical and biological consequences of the disease, and the reflections due to the social and emotional aspects arising from this new condition generate much preoccupation and anxiety. In this context, the follow-up, which goes beyond the nursing consultation, enables the nurse to be present in the patients' homes. The technological resource increases the frequency of contact between patients and nursing professionals, in comparison with the follow-up consisting only in consultations on the day of infusion. For patients, this support that increases the time of the professional available to the patient allows clarifying doubts and promotes greater safety of the treatment and conveys confidence to patients, their relatives and caregivers 4.
CONCLUSION
The most prevalent symptoms during the first stage of treatment, that is, the application of doxorubicin + cyclophosphamide, were fatigue, altered taste, anxiety and nausea. In turn, the main symptoms reported in the second stage of treatment, with the isolated infusion of docetaxel, were fatigue, altered sense of taste, myalgia, anxiety, arthralgia and inappetence. It is important to note that the symptoms varied in intensity during the evaluated week. Thus, it is of paramount importance for the nurse to be aware of the adverse effects of each medication to optimize the guidelines and, if possible, to prevent or minimize the damages.
Given the complexity of the chemotherapy treatment and the necessary care to the patients, nurses assume a strategic role as members of a multidisciplinary team, with the responsibility of identifying, evaluating and proposing care interventions. In this sense, one of the major objectives of nursing care is to control the signs and symptoms resulting from this therapeutic modality, which occasionally become troublesome due to their multiplicity.
The telephone contact has proven to be an effective means to follow up patients and meet their needs throughout the chemotherapy treatment. Such monitoring increased the link between professionals and patients, and represents an important tool to the identification and evaluation of adverse effects of treatment and, when possible, their control.
However, difficulties in making contact and, therefore, following the patients was a limiting factor of the study. Thus, it was not possible to complete all the follow-ups in D8 and D15, making it impossible to more accurately measure the real impact of symptoms during treatment. Future studies may compare patients who receive assistance through weekly telephone contacts, and who are consequently followed up more frequently, with those who only receive the guidelines during face-to-face medical and nursing consultations.
REFERENCES
1.Bonassa EMA, Gato MIR. Oncology therapy for nurses and pharmacists. São Paulo: Atheneu Publisher; 2012.
2.Costa WB, Vieira MRM, Nascimento WDM, Pereira LB, Leite MTS. Women with breast cancer: interactions and perceptions about nursing care. Rev Min Enferm. 2012; 16(1): 31-7.
3.RosaI LM, RadünzII V. Meaning of breast cancer in women's perception: from symptom to treatment. Rev enferm UERJ. 2012; 20(4): 445-50.
4.Cruz FOAM, Ferreira EB, Reis PED. Nursing consultation by telephone: reports of patients submitted to antineoplastic chemotherapy. Rev. Enferm. Cent O Min. 2014; 4(2): 1090-99.
5.Vasconcelos HCA, Freitas RWJF, Marinho NBP, Damasceno MMC, Araújo TL, Teixeira FE. Efficacy of interventions using the telephone as a strategy for glycemic control: Integrative literature review. Texto contexto-enferm. 2013; 22(1): 239-46.
6.Furuya RK. Educational program with telephone follow-up for patients undergoing percutaneous coronary intervention: randomized controlled clinical trial [doctoral thesis]. Ribeirão Preto (SP): University of São Paulo; 2013.
7.Jong N, Kester AD, Schouten HC, Abu-Saad HH, Courtens AM. Course of fatigue between two cycles of adjuvant chemotherapy in breast cancer patients. Cancer Nurs. 2006; 29(6): 467-77.
8.Berger AM, Higginbotham P. Correlates of fatigue during and following adjuvant breast cancer chemotherapy: A pilot study. Oncol Nurs Forum. 2000; 27(9): 1443-8.
9.Schmid-Büchi S, Halfens RJ, Müller M, Dassen T, van den Borne B. Factors associated with supportive care of patients undergoing breast cancer treatment. Eur J Oncol Nurs. 2013; 17(1): 22-9.
10.Cheung YT, Lee HH, Chan A. Exploring clinical determinants and anxiety symptom domains among Asian breast cancer patients. Support Care Cancer. 2013; 21(8): 2185-94.
11.Costa TMN, Sampaio CEP. Nursing guidelines and their influence on anxiety levels of hospital surgical patients. Rev enferm UERJ. 2015; 23(2): 260-5.
12.Garcia SN, Jacowski M, Castro GC, Galdino C, Guimarães PRB, Kalinke LP. The domains affected in the quality of life of women with breast neoplasia. Rev Gaúcha Enferm. 2015; 36(2): 89-96.
13.Jansen CE, Dodd MJ, Miaskowski CA, Dowling GA, Kramer J. Preliminary results of a longitudinal study on changes in cognitive function in breast cancer patients undergoing chemotherapy with doxorubicin and cyclophosphamide. Psychooncology. 2008; 17(12): 1189-95.
14.Hong JH, Omur-Ozbek P, Stanek BT, Dietrich AM, Duncan SE, Lee YW, et al. Taste and odor abnormalities in cancer patients. J Support Oncol. 2009; 7(2): 58-65.
15.Gamper EM, Giesinger JM, Oberguggenberger A, Kemmler G, Wintner LM, Gattringer K, et al. Taste alterations in breast and gynaecological cancer patients receiving chemotherapy: prevalence, course of severity, and quality of life correlates. Acta Oncol. 2012; 51(4): 490-6.
16.Steinbach S, Hummel T, Böhner C, Berktold S, Hundt W, Kriner M, et al. Qualitative and quantitative assessment of taste and smell changes in patients undergoing chemotherapy for breast cancer or gynecologic malignancies. J Clin Oncol. 2009; 27(11): 1899-905.
17.Gozzo TO, Moyses AM, Silva PR, Almeida AM. Nausea, vomiting and quality of life of women with breast cancer undergoing chemotherapy. Rev Gaúcha Enferm. 2013; 34(3): 110-6.
18.Boaventura AP, Vedovato CA, Santos FF. Profile of cancer patients treated at an emergency unit. Ciencia y enfermería. 2015; 21(2): 51-62.