RESEARCH ARTICLES
Palliative care and Alzheimer: neurologists’ conceptions
Ronaldo Bezerra de QueirozI; Ana Aline Lacet ZaccaraII; Márcia Adriana Dias Meirelles MoreiraIII; Luípa Michele SilvaIV; Solange Fátima Geraldo da CostaV; Antonia Oliveira SilvaVI
IMedical doctor. PhD Student of the Graduate Program in Nursing, Federal University of Paraíba. Researcher of the International Group for Study and Research on Aging and Social Representations. João Pessoa, Paraíba, Brazil. Email: qronaldo@ig.com.br.
IINurse. Master and Researcher at the Center for Studies and Research in Bioethics, Graduate Program in Nursing, Federal University of Paraíba. João Pessoa, Paraíba, Brazil. E-mail: anazaccara@hotmail.com.
IIIMedical doctor. Professor of Anesthesiology and Researcher at the Center for Studies and Research in Bioethics at the Federal University of Paraíba. João Pessoa, Paraíba, Brazil. E-mail: marciadmoreira@gmail.com.
IVNurse. PhD Student of Graduate Program in Nursing, Federal University of Paraíba. João Pessoa, Paraíba, Brazil. Email: luipams@gmail.com.
VNurse. PhD in Nursing. Professor of the Graduate Program in Nursing, Federal University of Paraíba. João Pessoa, Paraíba, Brazil. E-mail: solangefgc@gmail.com.
VINurse. PhD in Nursing. Professor of the Graduate Program in Nursing, Federal University of Paraíba. João Pessoa, Paraíba, Brazil. E-mail: alfaleda@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2014.15549
ABSTRACT: This study aimed to understand conceptions of neurologists about the practice of palliative care directed to the Alzheimer's patient. This is an exploratory qualitative study, conducted in clinics and hospitals located in a capital city of northeastern Brazil with 10 neurologists who work with individuals with Alzheimer's disease. Data collection was conducted from April to May 2012. For the acquisition of empirical material, we used a form with interviews. The material was treated by the technique of content thematic analysis. Qualitative analysis revealed three categories: purposes of palliative care; types of palliative care; and ways of coping. The testimony of medical research participants presented emphatically the importance of palliative care for the Alzheimer's patient and his family. Based on the foregoing, it is intended that this study can support further research in that area.
Keywords: Palliative care; Alzheimer’s disease; medicine; aging.
INTRODUCTION
Palliative care comprise a therapeutic approach through the prevention and relief of suffering by early identification, proper assessment and treatment of pain and other physical, psychosocial and spiritual problems to improve the quality of life of patients facing a life threatening disease, which affects the entire family dynamics1,2.
Diseases that tend to suggest that life will end generate many thoughts and emotionally affect both those who have a diagnosis of terminal illness and how those who are around him, and may lead the individual to the social and spatial isolation, and the consequence generally is depression and loneliness3 This detachment from loved ones creates a hardship on a delicate and individual time.
Regarding patients with Alzheimer's disease (AD), care involves ethical issues, with which the neurologist often face, including the time of diagnosis, how and when to communicate it, the consequences of disease progression and the their management, family involvement, the impact of the diagnosis on it and patient care4.
The diversity of needs of patients with AD and his family, in the final stage of life, related to the complexity of this suffering, and the specific approaches for each patient makes interdisciplinary work in palliative care necessary, whose elements are the doctor, nurse, psychologist, social worker, nutritionist and spiritual assistant5-7.
Accordingly, what motivated this study, from the point of view of the medical professional, was the recognition of the importance of AD on the world stage, particularly in Brazil, the difficulty of providing and receiving the diagnosis according to the need to promote a better quality of life for patients, associated with the implementation of palliative care through the professionals who care for patients affected by this pathology, which certainly will contribute to the provision of services for this purpose.
Given the above considerations, this study aims to present conceptions of neurologists about the practice of palliative care directed to the Alzheimer's patient.
LITERATURE REVIEW
For older adults with chronic illness such as AD, progression to death occurs when the patient is in a fragile condition, with the decline of biological functions and quality of life. Thus, it is necessary to promote an integral care to patient that also covers their families because the approaching death of their loved one in the family awakens physical and emotional wear5. This requires a holistic and humane approach that promotes comfort and relieves symptoms.
Thus, palliative care are presented as an important tool in healthcare practice for the physician, member of the multidisciplinary team, to provide quality care in treating the chronic patients affected by AD with dignity and respect, increasing the comprehensiveness of care6.
In this context, it is the neurologist’s responsibility to conclude diagnosis, understand the wishes of the family, take into account the position and circumstance of this family, the support the carrier will need regarding the therapy and nursing care, as well as a holistic, humane and singular care to a with patient terminal AD7.
METODHOLOGY
This is an exploratory qualitative study, conducted in clinics and hospitals located in a capital city of the Brazilian Northeast, with 10 neurologists who work with patients with AD and who agreed to participate voluntarily.
Data were collected through interviewers from April to May 2012. For the acquisition of empirical material, we used a form with subjective questions, in order to meet the goal, with subsidized questions in reference to palliative care and professional practice with patients affected by AD. The second part included the variables gender, age, years of academic training.
It is noteworthy that the collection was made after approval of the project by the Federal University of Paraíba Research Ethics Committee of the University Hospital Lauro Wanderley, under the protocol number 184/10. It was performed after doctors participating in the study signed an informed consent form, as provided in Resolution No. 196/1996 of the National Health Council, which establishes the standards and regulatory guidelines for human research in force on our country8.
The collected data were treated by means of thematic content analysis technique, which is used in field surveys of health, since it covers a set of techniques that favor treatement of the meanings of discourses9. The procedure included the following steps: Pre-analysis, which included the skimming reading of answered forms, which constituted the corpus; after preparation of the material it was held the technique of content analysis and, subsequently, there was a selection of units of analysis. The paragraph was considered as context units, and the phrase as log units. For cutting, classification and categorization, we opted for inductive categorical process, i.e., the categories were defined a posteriori.
In a second step, after the exploration of the material, when it was applied to the corpus the selected technique, it was performed treatment of the data; validation of the data obtained; inferences and interpretation of results, with the support of the theoretical framework1-7,10-27.
RESULTS
As categorization of 10 neurologists participants, it was found that the age ranged between 42 and 74 years old, six women and four men, nine of them possessed more than 20 years of academic training. It is noteworthy that only two participants attended a strictu sensu graduation.
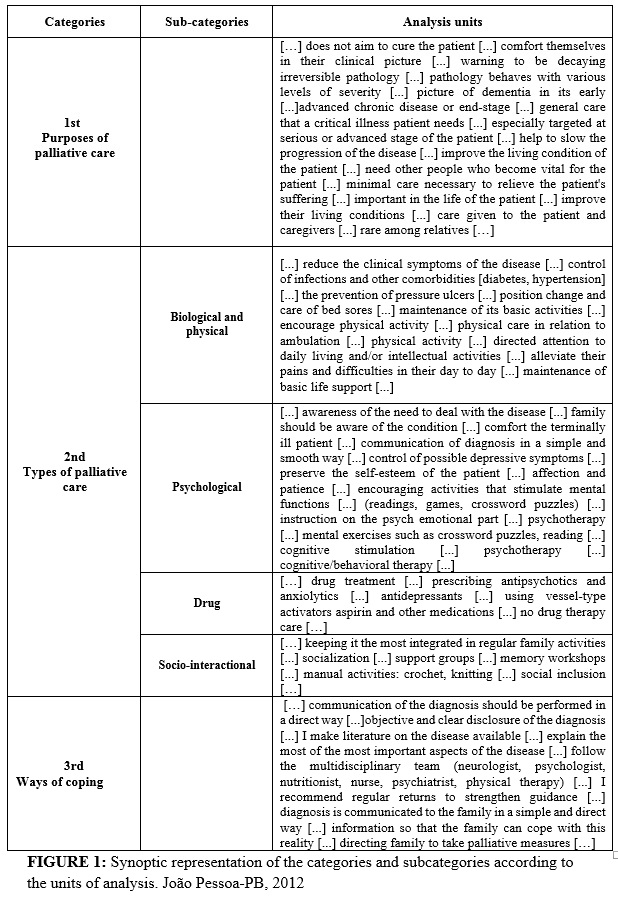
By analyzing the testimonies of doctors, three categories emerged: 1st Category - Purposes of palliative care; 2nd Category - Types of care and their respective sub-categories: biological/physical, psychological, drug and socio-interactional; 3rd Category - Ways of coping. The units of analysis, which correspond to the phrases collected, are explained in Figure 1.
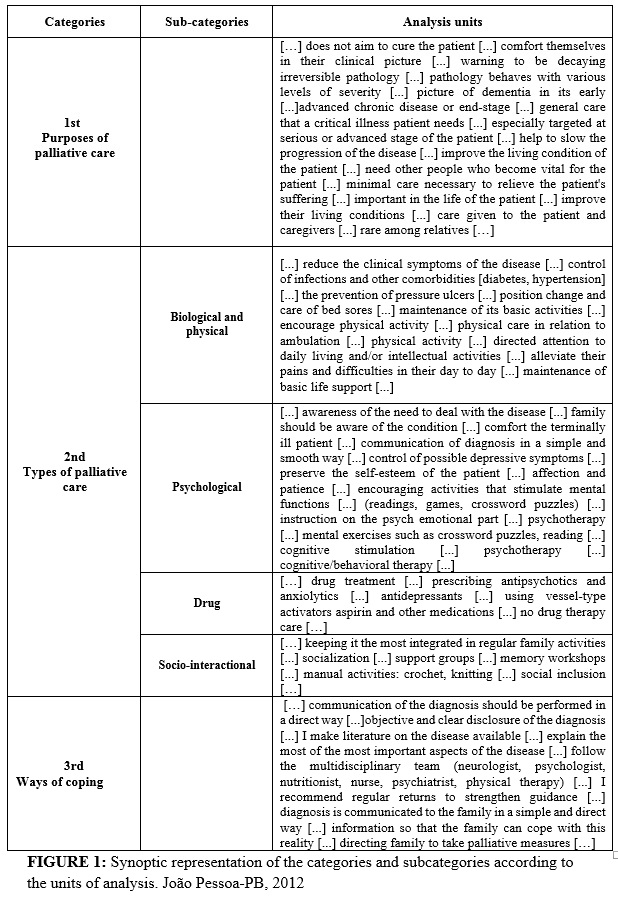
In the 1st category, the speech analyzes demonstrated the purposes of palliative care, as the following report:
[…] it does not aim to heal the patient [...] comfort themselves in their clinical picture [...] warning to be decaying irreversible pathology [...] pathology behaves with various levels of severity […]
The 2nd category arouses four sub-categories, which determine characteristic speeches of the types of care:
[...] control of infections and other co-morbidities (diabetes, hypertension) [...] comfort terminally ill patient [...] antidepressants [...] social inclusion […]
Thus, the 3rd category emerged from speeches such as:
[…] explain the most of the most important aspects of the disease [...] follow the multidisciplinary team (neurologist, psychologist, nutritionist, nurse, psychiatrist, physical therapy) […]
DISCUSSION
The analysis procedure adopted in this study enabled the construction of three categories: purposes of palliative care; types of palliative care; and ways of coping.
1st Category - Purposes of palliative care
The neurologists understand palliative care as a tool to alleviate the suffering of patients with Alzheimer's disease, to provide comfort and improve their living conditions and their families. From this perspective, its focus is not the cure, i.e., in palliative care, health professionals seek care and recognize the limits of the treatments and medicine, as well as value comfort, well-being, zeal, dedication, empathy and attention to terminally ill being1,2,4,5.
In this sense, the concept of World Health Organization deserves to be highlighted, which considers palliative care as an approach that improves the quality of life of patients and their families, in the presence of problems associated with life-threatening illnesses, through the prevention and relief suffering with early detection and treatment of pain and other physical, psychosocial and spiritual problems10,11.
Palliative care aims to improve the quality of life of patients and their families through appropriate assessment and treatment to relieve pain and symptoms, and provide psychosocial and spiritual support11-15. For this it is necessary to promote an integral care to patients, including their family, since the approaching death of their loved one cause in the family physical and emotional exhaustion4. For this, the connecting thread is a holistic and humane approach that promotes comfort and relief of symptoms. In another approach, the speeches of the physicians participating in the study show sensitivity to others, searching for their comfort, which culminates with a deep respect for the patient and his family and promote the dignity of both parts.
Study showed that caring for each other and respecting the experience of the moment of pain and difficulty enables to build a relationship of trust between caregivers and patients and their families12.
2nd Category - Types of palliative care
It presents four subcategories seized from neurologists’ speeches in the study: biological/physical; psychological; drug and socio-interactional care.
Subcategory - Biological/physical care
It is related to continued care and symptom management, control, prevention and maintenance of basic daily activities and the increasing dependence generated during the process of evolution of the patient with AD.
Palliative care advocate that care to patients without therapeutic possibility of cure must be based on listening, perception, understanding and identifying the needs for only then planning actions. It is noteworthy that such care emerges as a strategy through which care is provided, taking into account the appreciation of the uniqueness of the patient. Therefore, the team needs to be available and receptive to care for the Alzheimer's patient in its entirety6.
Studies show that when practitioners report a concern with feeding, including the possibility of indicating enteral feeding, they suggest more than one type of palliative care5-7,10-19. According to the American Dietetic Association, in this type of care, feeding should provide pleasure, emotional comfort, decreased anxiety and increased self-esteem and enable greater integration and communication with their families13.
Palliative care aim at avoiding or minimizing clinical symptoms of the disease and controlling infections and other comorbidities such as diabetes, hypertension, prevention of pressure ulcers and decubitus change and care of pressure sores, pain relief, etc.5-7,10,27.
Subcategory - Psychological Care
It highlights neurologists’ concern with integrity, for as long as possible, of the psychological structure of the patient with AD and those involved in their care. Thus, humanizing care to the needs of all who deal with the disease with no possibility of cure and improving the quality of life is only possible with palliative care in its first sense of ease the disorder of the process since the time of diagnosis14.
From a psychological standpoint, offering palliative care involves assisting patients with Alzheimer's, their family caregivers and professionals, from the perspective of five main dimensions: physical, psychological itself, social, spiritual and ethical, since the moment of diagnosis, aiming maintain or improve the quality of life for all involved15. To do so, it is not enough to control and relieve symptoms, but also support to maintain the family structure and promote communication among members of the unit of care, emotional and social support.
In face of a diagnosis of a disease that is inexorably threatening and has no possibility of cure, everybody becomes vulnerable and is affected in some way. Therefore, it is up to the psychologist to act as a link between the family and the palliative care team, aiming to seek answers to face the final stage of life, and contribute so as to strengthen the family, to communicate well with staff, to develop their sense of control over what is known or is not known, to understand the process of death and identify symptoms that require immediate attention, to be an effective agent in this process15.
The behavioral and psychological symptoms of dementia can be treated with behavioral therapy, multisensory stimulation, cognitive stimulation, physical exercise, music therapy, recreation, art therapy, creative expression encouragement and storytelling programs that stimulate imagination16. Such activities may have mood-related benefits, stimulate memory and lead patients to share their experiences and values.
Subcategory - drug care
In the professionals’ descriptions, there is a clear concern with palliative care on the knowledge about the medications that should be used in patients with no chance of cure disease, such as AD.
According to studies on conceptions of palliative care, pain occurs in individuals who experience a lot of discomforts of physical, psychological, social and spiritual character, such as skin lesions, unpleasant odors, anorexia, cachexia, insomnia, fatigue, anticipatory grief, economic difficulties, depression, etc1-3,7,10-27.
It is known that in practice, poorly controlled pain has an impact beyond the physical realm, both for the individual patient and for the family and health professionals. Hence the term total pain was born, since pain in humans, is a frame that, in addition to nociception (number of damaged tissue), involves physical, emotional, social and spiritual factors that influence the experience and expression of complaint of pain. Thus, the control and the relief of pain and other symptoms is an individual right and a duty of professionals, who must develop strategies to reduce the suffering caused by this situation17.
It is noteworthy that studies suggest that antipsychotics such as risperidone (1mg/day) and olanzapine (5-10 mg/day) are effective as drug therapy in patients with AD. However, in recent years, regulatory authorities, including the National Health Surveillance Agency (ANVISA), reported that both drugs increase the risk of cerebrovascular events18.
Subcategory – socio-interactional care
It is identified the need to maintain the socialization of the patient and their engagement in productive activities in an attempt to preserve and enjoy their cognitive reserves to improve their quality of life and their families.
Given the testimony of physicians participating in the study, in terms of attention to the social aspect of the patient, it is highlighted the inclusion of the family throughout the treatment process. This attitude is fundamental to the care required by the patient, and this confirms the need to listen to their suffering and willingness to learn to deal with the difficulties that arise in the course of the disease. Thus, the stimulus to family life and strengthen family ties are mainly intended to reduce anxiety and suffering19.
Authors have shown improvement in the cognitive and functional performance in patients at early stages of AD, with the use of psychosocial interventions, particularly when associated with envisaged drug treatment. However, few studies have set out to elucidate the efficacy of non-pharmacological treatment of subjects at more advanced stages of the disease20.
The earlier the diagnosis of AD and starting treatment, including socio-interactive measures - neuropsychological rehabilitation – the better results will be obtained because the patient can remain at a higher cognitive and functional level. This makes it possible, even, that he remains independent longer and avoid burdens for their families. Small cognitive changes or even stabilization of some cognitive functions already show large gains in the case of patients with neurodegenerative disease.
3rd Category - Ways of coping
It underscores the ways of dealing with the disease, which ranges from family members when they are communicated, so that they have the necessary information, as well as the patients themselves who shall be an interdisciplinary monitoring in which there is an interaction between: doctor, nurse, psychologist, nutritionist, patients and families. These features are evident in the testimonies of professionals surveyed on the exchange of information between doctor and family members of patients with AD who value this relationship.
The speeches of the participants expressed that they understand the importance of diagnostic information to be given to the family. From this perspective, the family members play an important role and should be seen as responsible for their health. Is the reason why they should be heard, valued and encouraged to participate in all phases of the disease, from diagnosis and throughout the care process. This is relevant because AD, for its characteristics, is undoubtedly a nightmare in the life of its carrier and his family21.
Regarding the disclosure of the diagnosis to the family of a patient with a chronic, progressive degenerative disease such as Alzheimer's, it is possible to point out that it is intrinsically linked to prior personal and professional experience of the informants. Also, one must wonder if the news should be given to the family or to the patient himself22. Regarding this pathology, except in exceptional cases, the exchange of information is usually kept with the family because the individual is unable to receive his diagnosis due to neurological impairment that can be installed in varying degrees.
As well as the diagnosis, guideline on the care that must be provided to the patient is referred to the family. We understand the sheer importance of the family in the context under discussion. One study found that 70% of doctors surveyed claim to support and establish a trusting relationship with the family of the patient, showing the consideration given to the patient’s family by professionals23. However, to cope with the disease, it is necessary to speak the truth, because it is vital, and there are proper ways to communicate it. The way a doctor interacts with patients and family is extremely important, because it might be the beginning of a painful, sustained and difficult process for everyone involved. Probably, this moment will be decisive for driving the storm of feelings that will surface and will drive the health-disease binomial that will involve the patient and their family24.
The study warns, however, that the attitude of professionals can both tranquilize the individual to face the changes in his life, and worse the emotional health state. Therefore, how to deal with the diagnosis should be well crafted, since the way this task is accomplished will guide the feelings and attitudes that lead patients and families to cope with the disease23.
In this light, it is approached the difficulty of communicating the diagnosis of a terminal illness, given that this task must be accomplished in procedural and cautious manner, from the moment it raises a number of fantasies, culminating with the fear of death13.
In this sense, the study highlights the strategies used to promote good communication, namely: the use of verbal and non-verbal communication to support the humane care to the patient, to provide support, safety, trust, convey strength and hope, which is paramount in the context of palliative care25.
Besides the communication strategies, assessment and management of behavioral and psychological symptoms of AD are a challenge, and ethical dilemmas often arise. Research indicates that physicians often do not perceive a disconnection between evidence-based guidelines and the challenges of treating AD. Given the fact that it is a progressive disease, the study proposes an approach to palliative care that prioritizes the recognition of personhood and the preservation of dignity26.
Especially, when patients with AD reach the final stage of the disease their ability to provide subjective complaints pertaining to pain and discomfort gets reduced. Thus, exploring the disease process, ethical issues and important clinical considerations are necessary to improve the quality of care for patients with end-stage AD27.
CONCLUSION
In this research, it was evident the importance of this type of care, offering support to meet the biological, psychological and social needs of the patient and giving more attention to drug therapy and the ways to tackle the disease, according to the conceptions of neurologists on palliative care, on professional practice, when dealing with the Alzheimer's patient.
There was unanimous position on the AD - the family is of crucial importance, since it is the one who receives the diagnosis, therefore, it is responsible for the patient throughout the process of illness. Professionals have also highlighted the importance of communication as a fundamental strategy in the practice of palliative care.
The testimony of medical doctors participating on research shows, emphatically, the importance of palliative care for the Alzheimer's patient and their family. Based on the foregoing, it is intended that this research will support further research in this area.
The limitation found in this study was the lack of a dedicated unit for this type of therapeutic approach; it is perceived, in the addressed literature, this Brazilian problematic. Therefore it requires dedication of professionals and investment in professional training in the area of palliative care and terminal patients.
REFERENCES
1.Rodrigues IG, Zago MMF. A morte e o morrer: maior desafio de uma equipe de cuidados paliativos. Cienc Cuid Saude. 2012; 11: 31-8.
2.Rodrigues IG, Zago MMF. Cuidados paliativos: realidade ou utopia? Cienc Cuid Saude. 2009; 8: 136-41.
3.Vasques TCS, Lunardi VL, Silveira RS, Gomes GC, Lunardi Filho WD, Pintanel AC. Percepção dos trabalhadores de enfermagem acerca da implementação dos cuidados paliativos. Rev enferm UERJ. 2013; 21: 16-22.
4.Paula JJ, Bertola L, Nicolato R, Moraes EN, Malloy-Diniz LF. Evaluating language comprehension in Alzheimer's disease: the use of the Token Test. Arq Neuro-Psiquiatr. 2012; 70: 435-40.
5.Bifulco VA, Iochida LC. A formação na graduação dos profissionais de saúde e a educação para o cuidado de pacientes fora de recursos terapêuticos de cura. Rev bras educ med. 2009; 33(1): 92-100.
6.Machado J, Caram CLB, Frank AA, Soares EA, Laks J. Estado nutricional na doença de Alzheimer. Rev Assoc Med Bras. 2009; 55: 188-91.
7.Blasco PG. O médico perante a morte. Rev Bras de Cuidados Paliativos. 2009; 2(4): 7-13.
8.Ministério da Saúde (BR). Conselho Nacional de Saúde, Comissão Nacional de Ética em Pesquisa. Resolução nº 196 de 10 de outubro de 1996: diretrizes e normas regulamentadoras de pesquisa envolvendo seres humanos. Brasília (DF): CNS; 1996.
9.Bardin L. Análise de conteúdo. Lisboa (Pt): Edições 70; 2012.
10.Mencarelli VL, Bastidas LS, Aiello Vaisberg TMJA. A difícil notícia da síndrome de imunodeficiência adquirida para jovens: considerações psicanalíticas com base na perspectiva winnicottiana. Psicologia: teoria e prática. 2008; 10(2): 106-20.
11.World Health Organization (WHO). Who definition of palliative care [Internet]. 2012. [cited 2014 Feb 18]. Available at: http://www.who.int/cancer/palliative/definition/en/.
12.Floriani CA, Schramm FR. Cuidados paliativos: interfaces, conflitos e necessidades. Ciênc Saude Colet. 2008; 13(2): 2123-32.
13.Benarroz MO, Faillace GBD, Barbosa LA. Bioética e nutrição em cuidados paliativos oncológicos em adultos. Cad Saude Publica. 2009; 25: 1875-82.
14.Santos FS. Cuidados Paliativos: diretrizes, humanização e alívio de sintomas. São Paulo: Editora Atheneu; 2011.
15.Melo AC, Valero FF, Menezes M. A intervenção psicológica em cuidados paliativos. Psic., Saúde & Doenças (Lisboa). 2013; 14: 452-69.
16.Phillips L, Reid-Arndt S, Pak Y. Effects of a creative expression intervention on emotions, communication, and quality of life in persons with dementia. Nurs Res. 2010; 59: 417-25.
17.Silva EP, Sudigursky D. Concepções sobre cuidados paliativos: revisão bibliográfica. Acta Paul Enferm. 2008; 21: 504-8.
18.Caixeta L. Doença de Alzheimer. Porto Alegre (RS): Artmed; 2012.
19.Nunes MGS, Rodrigues BMRD. Tratamento paliativo: perspectiva da família. Rev enferm UERJ. 2012; 20(3):338-43.
20.Cunha FCM, Cunha LCM, Silva HM, Couto EAB. Abordagem funcional e centrada no cliente na reabilitação de idoso com Demência de Alzheimer avançada: relato de caso. Rev Ter Ocup Univ São Paulo. 2011; 22: 145-52.
21.Neumann S, Dias C. Living with Alzheimer's Disease in the family. Journal of Nursing UFPE on line. 2011; 5: 967:73.
22.Oliveira FT, Aparecida D, Marengo FMO, Silva RHA. Bioética e humanização na fase final da vida: visão de médicos. Rev Bioética. 2011; 19: 247-58.
23.Peternella FMN, Marcon SS. Descobrindo a Doença de Parkinson: impacto para o parkinsoniano e seu familiar. Rev Bras Enferm. 2009; 62: 25-31.
24.Araujo MMT, Silva MJP. O conhecimento de estratégias de comunicação no atendimento à dimensão emocional em cuidados paliativos. Texto contexto - enferm. 2012; 21: 121-129.
25.Brito FM, Costa ICP, Costa SFG, Andrade CG, Santos KFO, Francisco DP. Comunicação na iminência da morte: percepções e estratégia adotada para humanizar o cuidar em enfermagem. Esc Anna Nery. 2014; 18: 317-22
26.Passmore MJ1, Ho A, Gallagher R. Behavioral and psychological symptoms in moderate to severe Alzheimer's disease: a palliative care approach emphasizing recognition of personhood and preservation of dignity. J Alzheimers Dis. 2012; 29: 1-13.
27.Yeaman PA, Ford JL, Kim KY. Providing quality palliative care in end-stage Alzheimer disease. Am J Hosp Palliat Care. 2013; 30: 499-502.