RESEARCH ARTICLES
The safety of nursing worker in administration of antineoplastic drugs intravenously
Monique Haenscke SennaI; Cândida Custódio da SilvaII; Francine Lima GelbckeIII; Jane Cristina AndersIV; Maria Patrícia Locks de MesquitaV
INurse. PhD Student from Graduate Nursing Program, Federal University of Santa Catarina (UFSC). Member of the Group of Studies and Research in Administration and Management of Nursing and Health Care (GEPADES). Florianópolis, Santa Catarina, Brazil. E-mail: moniquehsenna@hotmail.com.
IINurse. Specialist in Family Health. Florianópolis, Santa Catarina, Brazil. E-mail: candycustodio@yahoo.com.br.
IIINurse. PhD in Nursing. Professor of Department of Nursing, the Graduate Nursing Program and the Professional Master in Nursing Care Management at UFSC. Member of the Group of Studies on Labour, Citizenship, Health and Nursing (PRAXIS). Florianópolis, Santa Catarina, Brazil. E-mail: francine.lima@ufsc.br.
IVNurse. PhD in Nursing. Professor of Department of Nursing, the Graduate Nursing Program and the Professional Master in Nursing Care Management at UFSC. Group Leader for Teaching and Research in Child and Adolescent Health (GEPESCA). Florianópolis, Santa Catarina, Brazil. E-mail: jane.anders@ufsc.br.
VNurse at University Hospital. PhD Student from Graduate Nursing Program, UFSC. Member of the PRAXIS Group. Florianópolis, Santa Catarina, Brazil. E-mail: pattylocks@yahoo.com.br.
DOI: http://dx.doi.org/10.12957/reuerj.2014.15513
ABSTRACT: Occupational exposure of workers handling antineoplastic chemotherapy drugs may occur during preparation, administration and disposal, being essential to proper use of personal protective equipment (PPE). This is a qualitative and quantitative study, conducted in southern Brazil. The objective was to identify the knowledge of workers on the proper use of PPE, and to analyze the process of administration of chemical agents by nursing staff in a medical unit and chemotherapy ambulatory at a university hospital. In data collection, in 2010, questionnaire and field observations were used. It was identified that workers know the care of protection, but do not perform it effectively in the medical unit, different from that observed in the ambulatory, which can be related to the fact that they act in their daily lives with such drugs, generating a greater commitment to their security. The results revealed the need for continuing education to raise awareness of the risk of exposure to antineoplastic drugs.
Keywords: Occupational Health; occupational hazards; chemotherapy; protective equipment.
INTRODUCTION
Occupational health reflects an institutional response to social movements that between the mid-70s and 90s claimed that the health issues related to work were part of the universal right to health, being included in the scope of public health1. Worker’s health in Brazil arises during the period of democratic transition, when the questions about the interference of work in the health-disease process begin. This moment is characterized by the existence of epidemics, classic occupational diseases and the emergence of new illnesses caused in the workplace, due to globalization and changes in work practices2-5. Their physical, mental and social well-being is closely related to social, economic, organizational, and technological factors.
Workers are constantly exposed to damage when exposed to different occupational hazards: physical, ergonomic, chemical, biological and psychosocial, whose importance is related to the professional category and area of operation3. The recognition of the risk that the worker is exposed involves predicting events or situations in the workplace that may cause bodily injury or functional disorder, based on prior or estimated knowledge, in order to adopt patterns of behaviors and precautions to minimize the risks4. For worker protection during handling of chemotherapy, it is essential to use personal protective equipment (PPE), such as powder-free gloves, disposable gowns with elastic wrist and masks with activated carbon filter3-5.
Accordingly, with this study we seek to answer the following guiding question: how are standards of worker safety implemented in the administration of intravenous antineoplastic drugs (Qt-An) in a university hospital?
The following objectives were established: to identify the knowledge workers on the proper use of PPE and to analyze the process of administration of chemicals cited by the nursing staff, in a medical unit and chemotherapy ambulatory at a university hospital.
LITERATURE REVIEW
The incidence of cancer grows in Brazil and throughout the world, a pace that accompanies population aging due to increased life expectancy. It is the direct result of the large global transformations of recent decades, which changed the health status of the people by rapid urbanization, new lifestyles and new consumption patterns.
Occupational cancer is caused by exposure during working life, to carcinogens present in the workplace. Risk factors can be environmental or hereditary, both of which can be related. These factors interact in various ways to initiate the cellular changes involved in cancer etiology. According to some studies, on average, 2% to 4% of all cancers may be associated with exposures occurring in the workplace6-8.
Hospitals have a variety of risks, among which the chemicals appear to be related more strongly with antineoplastic drugs, anesthetic gases and sterilizing agents. It is well known that exposure to Qt-An brings benefit to patients, but the risk to professionals, who are continually exposed to these agents, should be evaluated. These chemicals can cause acute poisoning in workers, chronic and pre-pathological states of various occupational diseases7.
Occupational exposure to health care workers that handle the drugs used in cancer chemotherapy can occur in any of the three phases of contact with these substances: preparation, administration and disposal of antineoplastic drugs. During preparation, the risks of exposure can occur during the opening of ampoules, the reconstitution of drugs, the withdrawal of solution from the vial and the removal of air from the syringe containing anticancer drugs. Regarding disposal, the risk is present when workers do not adopt biosecurity measures when handling body fluids, disposing materials that come into contact with bodily fluids and manipulating clothes contaminated by these fluids, as well as by the incorrect packaging of contaminated materials. That is, the contamination by antineoplastic drugs is directly or indirectly related to exposure to these substances8.
To protect workers during handling of chemotherapy drugs and excreta of patients undergoing chemotherapy, it is essential to adopt measures such as the use of vertical laminar flow cabinets for the preparation of antineoplastics and correct use of PPE in the various activities involving the manipulation of chemotherapy.
METHODOLOGY
This is a quantitative study. Data were obtained through a structured questionnaire with questions of multiple character, open and closed questions and a tool for focal observation, not participatory. The provisions of Resolution No. 196 of 1996 of the National Health Council, with regard to the ethical aspects of human research were obeyed, under the approval of the Ethics Committee on Research with Human Beings (CEPSH), Certification No. 918. Nursing professionals who participated in this study signed an informed consent form.
The study was conducted at a teaching hospital in southern Brazil. It was chosen to develop the study the medical unit II, where patients are admitted to the hematology to make use of chemotherapy, and the chemotherapy ambulatory.
The subjects participating in the study were the professionals that make up the nursing staff (nurses, nursing technician and nursing assistant) of both sectors in the period from August to November 2010. To ensure confidentiality and anonymity of participants, workers identified by the letters N to nurse, T for nurse technician and A for nursing assistant, followed by growing numbers.
Twenty nursing professionals responded to the survey questionnaire: six nurses, one of chemotherapy ambulatory and five of medical hospitalization unit; ten nursing technicians, two of chemotherapy ambulatory and eight of medical hospitalization unit; four nursing assistants, one of the chemotherapy ambulatory unit and three of medical hospitalization.
In field observations, ten nursing workers were followed during the administration of chemotherapy: one nurse from the chemotherapy ambulatory; seven nurse technicians, two of chemotherapy ambulatory and five of medical hospitalization unit; and two nursing assistants, one of the chemotherapy ambulatory and the other of medical admission unit, enabling thus the second instrument of research, the observation.
The qualitative data analysis enabled grouping by similarity, allowing its interpretation. Related to the quantitative approach, statistical analysis was performed with calculations of absolute and relative frequency.
RESULTS AND DISCUSSION
Depending on the turnover of patients and the specific chemotherapy treatment, it was not possible to concurrently hold the questionnaires and complete the instrument of observation. So, first we applied the questionnaire and after, we were able to observe them in the field.
In the field survey, data related to gender, occupational category, working unit, length of training and on the job, work shift, i.e., data that could draw a profile of the sample was collected; and data relating to the object of study - knowledge and use of PPE in Qt-In; such as purpose of chemotherapy; importance of using PPE in the administration of chemotherapy and PPE used; risks they face when applying Qt-In; symptoms subsequent to the application; and whether they had suffered an accident related to the administration of Qt-An. If they had ever had an accident with Qt-An, it was also questioned: how the accident occurred, what symptoms they presented and which were perceived, what steps were taken and whether they had knowledge of the side effects of the current accident. We sought to thereby compare the data from the questionnaires to the observation in the field, because many times the worker knows the necessary care, but does not use them in everyday practice.
In field observation seven nursing technicians, two nursing assistants and one nurse were followed. These numbers are related to the composition of the workforce, in which there is a significant number of not graduated nursing professionals, and activities defined by the law of professional practice, which states that the nurses are responsible for the supervision of services and assistance directly, especially to critically ill patients. Regarding the workforce, the statistics of registered professionals for the State of Santa Catarina, in 2010, 33,700 (80%) of the nursing professionals are not graduated, with 23,784 (56%) nursing technicians and 9,916 (24%) nursing assistants, 8,422 (20%) are graduated professionals (nurses) 9. This smaller quantity of nurses in health care facilities may be influencing the activities performed by these professionals with regard to direct assistance. It should be noted that we only observed the nurse administering such drugs in chemotherapy ambulatory and in the medical unit this care has not been performed by the nurse. One can assume that this care provided on an ambulatory basis is because there is a smaller quantity of professionals in this service, coupled with increased demand of Qt-An management.
Data from general knowledge about chemotherapy such as purpose, risk of exposure, which PPE are required in Qt-An administration, among others were raised. On participants' responses, 16 (80%) workers indicated that the purpose of chemotherapy is the treatment of cancer, 15 (75%) indicated the destruction of cancer cells, 13 (65%) to prevent, control or reduce tumor growth, 11 (55%) to avoid the appearance of metastasis and 6 (30%) nodes reduction. In general, workers know the goal of chemotherapy, however in a superficial and limited manner, suggesting a deficit in continuing education and deepening the theme.
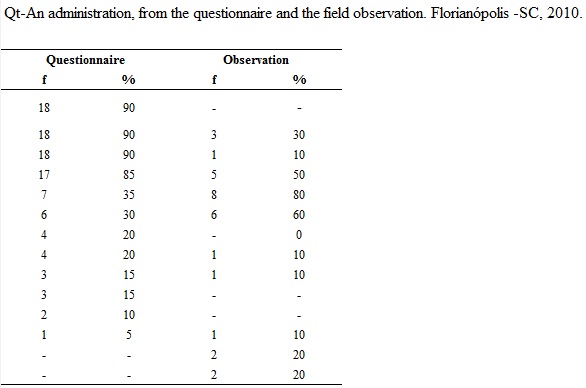
Regarding the use of PPE, the data presented refer to what was raised in the questionnaires and field observation, as shown in Table 1.
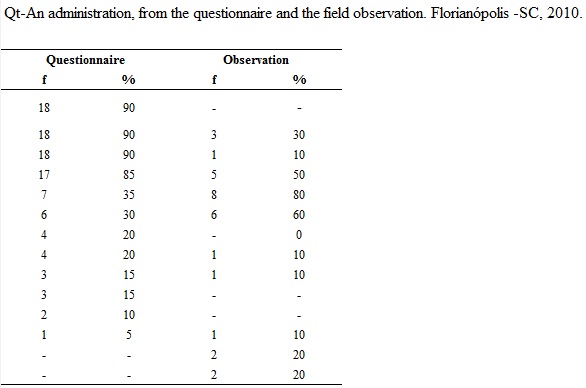
By analyzing the data of observation and confronting them with the questionnaires, we noted a significant discrepancy between the observed reality and the described reality, especially in the use of PPE, fundamental element to individual, collective and environmental biosafety. Most participants described making use of equipment beyond the recommended (according to Table 1, referring to the questionnaire), to greater protection coverage, but it was observed a neglect of these professionals to protect themselves against the exposure to antineoplastic substances, according to Table 1, referring to the observation.
The rules of the US Agency Safety and Occupational Health Administration (OSHA) set as obligatory the use of PPE for handling and administration of antineoplastics and specify the use of aprons long sleeves, elastic cuffs, with closed and disposable front; glasses full protection; protective masks with activated carbon and; thick polypropylene or latex gloves, disposable and powder-free5. Recommendations of the standard precautions are being used by health professionals for over 15 years, especially after the accession of universal precautions for protection. This primary prevention continues to be effective and efficient in protecting workers against occupational hazards10. The recommended is that the professional is always protected during patient care, making constant use of PPE. The major causes of accidents among employees of the nursing staff occur during handling of sharps due to the lack of adherence to use of PPE8.
It is noteworthy that the institution, in general, offers such protection equipment for workers’ use, which does not therefore justify not using them. An action that could change this lack of adherence to PPE would be continuing education of these professionals, conducting educational workshops and providing informational materials in order to arouse their attention to the risks they face when coming into direct contact with the antineoplastic substances. For this to happen, there must be a reorganization of the service process, which there is already in discussion in the institution.
As for the other measures necessary, the institution seeks to follow the recommendations of the National Health Surveillance Agency (ANVISA) and other specific organs, ensuring the provision of individual and collective protective equipment, use of vertical laminar flow chapel for handling and specific boxes for disposal of toxic material11, but there is some resistance to the full and correct use of this material, highlighting the need for continuing education.
In the survey of the importance of using PPE, it was observed limited knowledge about the real value of this material, not only as individual protection but also as collective protection, since it aims safety to oneself and others in ethical context. The responses of the survey are highlighted:
It is vital that the professional has awareness regarding the use of PPE as well as in relation to the existing safety culture within the institution. It is the professional’s responsibility the proper use of PPE for each situation and responsibility of the institution to offer this equipment. (N16)
To reduce to the maximum the possibilities of contamination accidents with medicines used both EV as VO. (T17)
In relation to the risks they are exposed to contact with the chemotherapy, the presented data refer to what was raised in the questionnaires, as ordered in Table 2.
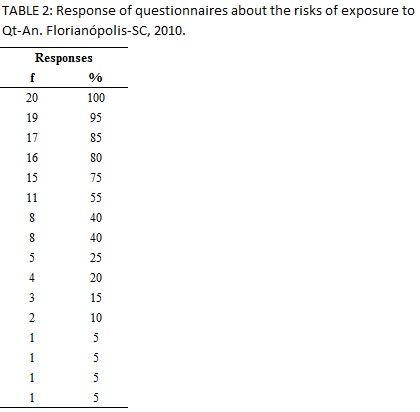
It was observed that the nursing staff know the risks of exposure to Qt-An in the short term, i.e. to come into direct contact with the drug or the occurrence of work accidents, but most are unaware of the long-term effects, as shown in Table 2. However, scientific data arise that there are several symptoms that occur with workers handling Qt-An, among which stand out the more immediate effects, such as dizziness, headache, nausea, changes in mucous membranes and allergic reactions among others12.
In this sense, care related to professionals who handle antineoplastic is needed due to the mutagenic potential of the medications, requiring the following technical and safety standards for handling these agentes6. Supervising the nursing staff constitutes fundamental role of the nurse, warning them of serious risks they are exposed when not adequately protected when handling chemotherapy drugs.
About adverse effects from chemotherapy, 9 (45%) respondents did not feel anything, 8 (40%) reported headaches and 4 (20%) nausea, 3 (15%), throat irritation, and 1 (5%) in heat face, these effects identified in the literature12. Of the 20 participants who answered the questionnaire, 05 reported having had accidents with the administration of chemotherapy.
In chemotherapy sector (infusion site,) when installing in the patient there was leaking on my coat and floor. (T18)
There was disruption in rubber connection of equipment in I, causing extravasation of chemotherapy on my face. The accident occurred on a day shift in Medical Unit II/University Hospital about 1 year ago. (A13)
Workers who suffered accidents with Qt-An leaking, reported feeling symptoms similar to adverse reactions that the patient presents during and after treatment, such as:
Headache and sore throat. (N5)
Changes in oral mucosa and headache. (N16)
On the measures taken after the accident, they referred to collective protective measures, thinking and focusing more on the others; professional colleagues, patients and families/caregivers; than on himself, as later described:
Site protection, disposal of bedding, patient care. Towards me, nothing. (N5)
It is noteworthy that the institution has extravasation of chemotherapeutic protocol and the support of the Division of Health and Safety of Work with the aim of promoting health, providing suitable conditions for worker/server; possessing forms to report accidents and communication of risks at work13. The following answer demonstrates care in case of accidents, either with patients or with workers:
Using the protocol of extravasation, forwarding all the material used for the cleanup to chemical waste container. To communicate and register the accident with the safety work’s service and request new particle count in the environment. (N16)
As for side effects, both long-term - after exposure to anticancer agents and short-term, after the accident, professionals have demonstrated knowledge of the risks, however, without assigning relevance to this issue:
In long-term it may bring cellular changes, but I believe that an isolated incident will not bring consequences. (N5)
The effects of chemical exposure are cumulative and added to the lifestyle, in which environmental factors tend to potentiate the side effects and consequences to the health of the individual 14. The role of nurses in the awareness of professional becomes crucial in guiding this worker to adopt biosecurity measures that could prevent potentially irreversible damage.
The care provided in chemotherapy ambulatory is more direct and focused, since the patient stays from 1pm to 4h30min in service for treatment. It is noteworthy that the space in this sector is presented in island format, facilitating the monitoring of the patient and possible adverse reactions. Since the ambulatory is able to receive seven patients at the same time to infusions of Qt-An, we noticed a major concern of employees in relation to contamination of the environment, i.e., the use of ventilation, the meticulous care for the installation of the infusion and disposal of all materials used. It was observed that in all circumstances the professionals used at least gloves procedures.
On the other hand, the medical clinic, the patient receives Qt-An in push and infusion. As in ambulatory, the staff, besides taking care of cancer patients, cares for patients from other specialties. Since there are 29 beds in the inpatient unit, care is held in a general way, often becoming unfeasible a focal care. It was noted that care throughout the infusion (from installation, handling of excreta and disposal of the material used) is not done with due attention, suggesting thus they are manipulating a drug whatsoever, without often PPE.
It is noteworthy to highlight the importance of nurses in surveillance, health promotion and safety of health workers, especially workers who handle chemotherapy. The actions to biosecurity must be continually developed by the nursing staff, mainly because they provide direct patient care, being constantly exposed to the risks of the activity itself15. The nurse should supervise their staff and promote actions for continuing education in order to exclude possible occupational risks to workers exposed to chemotherapy drugs.
Supervising, guiding and alerting the nursing staff is a primary role of the nurse as leader of the nursing team. The health care of workers can be enhanced through continuing education, educational workshops, informational materials, and especially with the active participation of nurses in caring for cancer patients. The team needs to be aware of the possible intervention of nurse to correct professional in the case of negligence, as this measure ensures safe care for the patient and the health professional either.
CONCLUSION
A growing use of antineoplastic drugs has been happening as a form of cancer treatment. In the same proportion, the rate of occupational exposure to these drugs accompanies its use, pointing a closer look at the risks that such exposure may lead; to worker’s health, throughout his life.
There is scientific evidence that side effects experienced by patients during treatment are also reported by professionals, being described discomfort such as headaches, allergic reactions and mucositis. In more advanced stages, there is evidence of carcinogenic risk associated with poor dietary habits, inexistent physical activity, abuse of substances, genetic predisposition and family history of the disease.
Likewise, patient’s biosafety against harmful agents is unanimity. It is necessary worker safety, thus comprising the individual, collective and environmental security, respecting ethical principles and universal rights. Worldwide, there are measures that ensure worker health through the use of PPE.
Data showed weakness experienced by nursing staff, since the professional thinks he knows enough to take care of himself and the others, without suffering accidents. However, we noted a greater concern with personal and collective safety, at the chemotherapy ambulatory, since it is a specialized service of management of An-Qt. In the medical unit data from this research were analyzed and discussed, and the conclusion is that an effective intervention is needed to educate its employees due to occupational risks to which they are exposed.
Results showed the knowledge of nurses regarding the meaning of the illness in question, on the occupational risks of treating the patient and the need for the use of PPE. However, the responses indicate the need for investment in professional development, continuing education, aiming to better awareness of self-care to reflect positively in the care of another. Biosecurity measures must be present at all times of the care provided by nursing staff. Therefore, it is necessary to continually educate these professionals, conducting educational workshops, lectures and discussions on the importance of this issue.
REFERENCES
1.Gomez CM, Lacaz FAC. Saúde do trabalhador: novas-velhas questões. Ciênc saúde coletiva. 2005; 10:797-807.
2.Duran ECM, Robazzi MLCC, Marziale MHP. Conhecimento de enfermagem em saúde do trabalhador oriundo de dissertações e teses. Rev Gaúcha Enferm. 2007; 28:416-23.
3.Almeida ANG, Tipple AFV, Souza ACS, Brasileiro ME. Risco biológico entre os trabalhadores de enfermagem. Rev enferm UERJ. 2009; 17:595-600.
4.Alves SSM, Passos JP, Tocantins FR. Acidentes com perfurocortantes em trabalhadores de enfermagem: uma questão de biossegurança. Rev enferm UERJ. 2009; 17:373-7.
5.Silva LF, Reis PED. Avaliação do conhecimento da equipe de enfermagem sobre riscos ocupacionais na administração de quimioterápicos. Rev Bras Cancerol. 2010; 56:311-20.
6.Instituto Nacional do Câncer (Br). Ações de enfermagem para o controle do câncer: uma proposta de integração ensino-serviço. 3ª ed. Rio de Janeiro: INCA; 2013.
7.Maia PG, Brito JC. Riscos relacionados à exposição de trabalhadores a quimioterápicos antineoplásicos: uma análise crítica da produção científica brasileira. Revista Tempus Actas de Saúde Coletiva. 2011; 5:51-65.
8.Gallas SR, Fontana RT. Biossegurança e a enfermagem nos cuidados clínicos: contribuições para a saúde do trabalhador. Rev Bras Enferm. 2010; 63:786-92.
9.Conselho Regional de Enfermagem. Estatística de profissionais cadastrados no COREn-SC. [citado em 06 nov 2013]. Disponível em http://www.coren-sc.org.br.
10.Neves HCC, Souza ACS, Barbosa JM, Ribeiro LCM, Tipple AFV, Alves SB, Suzuki K. O uso de equipamentos de proteção individual por profissionais em unidades de endoscopia. Rev enferm UERJ. 2010; 18:61-6.
11.Maia, PG. A atividade da equipe de enfermagem e os riscos relacionados à exposição a quimioterápicos antineoplásicos no setor de oncologia de um hospital público do estado do Rio de Janeiro [dissertação de mestrado]. Rio de Janeiro: Escola Nacional de Saúde Pública Sergio Arouca; 2009.
12.Xelegati R, Robazzi MLCC, Marziale MHP, Haas VJ. Riscos ocupacionais químicos identificados por enfermeiros que trabalham em ambiente hospitalar. Rev Latino-Am Enfermagem. 2006; 14:214-9.
13.Universidade Federal de Santa Catarina. Comunicação de acidente de trabalho. [citado em 11 nov 2010]. Disponível em: http://www.dsst.ufsc.br/acidentes-de-trabalho.
14.Randon FR. Avaliação dos níveis de genotoxicidade e estresse oxidativo em manipuladores de quimioterápicos em serviços de oncologia [dissertação de mestrado]. Caxias do Sul (RS): Universidade de Caxias do Sul; 2006.
15.Valle ARMC, Moura MEB, Nunes BMVT, Figueiredo MLF. A biossegurança sob o olhar de enfermeiros. Rev enferm UERJ. 2012; 20: 361-7.