ORIGINAL RESEARCH
Health personnel's perceptions of factors influencing hemodialysis treatment adherence
Rafaela Novaes FerrazI; Camilla de Godoy MacielII; Anna Karla de Oliveira Tito BorbaIII; Iracema da Silva FrazãoIV; Vanessa Vieira FrançaV
I
Nurse. Specialist in Nephrology by the Health Department of the State of
Pernambuco. Recife, Pernambuco, Brazil. E-mail: rafaelanf@hotmail.com
II
Nurse. Specialist in Nephrology by the Health Department of the State of
Pernambuco. Recife, Pernambuco, Brazil. E-mail:
camilladegodoymaciel@ig.com.br
III
Nurse. Master in nursing. Assistant Professor, Department of Nursing,
Federal University of Pernambuco. Recife, Brazil. E-mail: anninhatito@gmail.com
IV
Nurse. PhD in Social Work. Adjunct Professor, Department of Nursing,
Federal University of Pernambuco. Recife, Brazil. E-mail: isfrazao@gmail.com
V
Nurse. Master student in Nursing by the Graduate Program in Nursing,
Federal University of Pernambuco. Recife, Brazil. E-mail:
vanessafranca__@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2017.15504
ABSTRACT
Objective: to investigate health personnel's perceptions of factors influencing hemodialysis treatment adherence. Method: in this qualitative, descriptive study of 41 personnel in a hemodialysis service in northeastern Brazil, data were collected in 2014 by semi-structured interview and analyzed using Alceste software. The study was approved by the ethics committee (CAEE: 28265814.5.0000.5197). Results: 173 units of elementary contexts we classified and divided into four discursive classes: the patient-personnel bond as support in initial treatment difficulties; the renal patient's knowledge about the disease and its treatment as a strategy for adherence; depersonalization of the subject, allied to knowledge deficit and fear at catheter implantation; and patient, family and health personnel as an alliance in promoting self-care. Conclusion: communication, guidance, "embracement" and family are key to adherence to therapy.
Keywords: Renal Insufficiency; chronic; renal dialysis; health personnel; patient compliance.
INTRODUCTION
Chronic Kidney Disease (CKD) is a disease of multiple etiologies, characterized by injury and reduction of renal function for a period equal to or greater than three months. Due to its high prevalence, it is a public health problem, being more frequent among adults. It has occureed with an alarming incidence in contemporary society, with high morbidity and mortality rates. Chronic kidney disease has repercussions on daily life and socioeconomic life of the patient, as it entails frequent hospitalizations and increases hospital costs1,2.
It is a progressive and irreversible clinical syndrome that occurs when there is impairment of kidney function, which may lead the patient to a complex therapeutic regimen, consisting of dietary and liquid restriction and medication administration, in addition to Renal Replacement Therapy (RRT), which includes hemodialysis (HD) and peritoneal dialysis (PD), with hemodialysis being the most commonly used method. The hemodialysis treatment aims to replace the filter function of the kidneys, to remove nitrogenous excreta from the blood and the excess of liquids through a semipermeable membrane. The sessions last between two to four hours, performed about three to four times a week, and adherence to these variables directly reflect the quality of life of the patient1,3 .
To adhere is to follow the prescriptions and recommendations corresponding to the guidelines of the health professionals, being of paramount importance to reduce to the complications of the CKD4. Adherence to therapy, among other factors, depends on the efficient performance of the professional who has the responsibility to guide and solve the patients' doubts, and to clearly and objectively explain the recommended prescriptions in order to cope with the disease. This professional-patient bond has a positive effect on adherence3,5.
Following treatment regularly is not na easy behavior and there are a number of factors contributing to non-adherence, such as financial problems, the large number of drugs prescribed, adverse effects, the treatment regimen, the conditions of accessibility to the health service and the inadequacy of the professional-patient relationship6.
Patients with terminal CKD on hemodialysis often experience loss of autonomy due to dependence on the treatment for life support. Faced with this problem, the multidisciplinary team has the role of providing humanized assistance to patients and their families, focusing on active listening and psychological support aimed at identifying difficulties with treatment, as well as at explaining the importance of following the recommendations provided7. Thus, it is essential that the multidisciplinary team works in an integrated manner, since professionals have a shared responsibility towards the chronic renal patient3.
Faced with this problem, the present study aimed to investigate the perception of health professionals about the factors that interfere in adherence to hemodialysis treatment.
LITERATURE REVIEW
Adherence to hemodialytic treatment requires that the individual accepts the CKD and then understands the importance of maintaining the therapeutic regimen for health, quality of life and survival8. Several factors, such as age, low education, income, marital status, smoking, duration of the hemodialysis (HD) session, comorbidities, absence of caregivers and relatives, time of the restricted-diet-based regimen, reduced water intake and use of several medications, in addition to the confusion of the guidelines, lead to the refusal of the patient to carry out the therapy in the long term9.
Other barriers to adherence include discomfort of arteriovenous fistula puncture, limitation of leisure time, lack of transport, suffering of losses, alteration of image and of organ function, and consequently periods of anguish, anxiety and depression5.
In addition, the evolving chronic disease is accompanied by various feelings and involves several factors which, often, the individual is not able to face, initially. At the beginning of the hemodialysis treatment, the renal individuals experience a rupture of their life habits when adapting to a new reality that sometimes prevents them from carrying out previously achieved activities, besides the difficulties associated with the communication process and the lack of knowledge of specific aspects of treatment. However, the relationship with the family, with other service users, and with health team members is an important point in their recovery and adaptation amid the adversities imposed by the disease and the treatment10.
Commonly, psychological and social difficulties arising from renal failure and treatment decrease when service providers stimulate individuals to be independent. This action requires a lot of sensitivity and empathy from the team to recognize the real needs of the clients and to promote acceptance throughout the hemodialysis treatment5.
The dietary and behavioral limitations imposed by the disease and the multiplicity of the therapeutic measures associated to the lack of knowledge of patients and their relatives contribute to poor adherence to the treatment. Thus, it is the responsibility of the multidisciplinary team to guide the patient and his/her relatives about the disease and the treatment using a language that is clear and adequate to the understanding and educational level of those involved11.
In this scenario, the health professional is a key player in promoting adherence to therapy, since each patient requires an individualized evaluation. Patient-professional dialogue is considered the best approach to assess adherence and to provide care. However, strategies such as hosting and group formation are still a gap in the assistance environments 12.
These actions could be implemented in order to encourage adherence in face of the difficulties encountered in daily care, since the groups allow the identification and solving of doubts and fears from the design of strategies to support the problems in the therapeutic scope9 starting from the reality and the difficulties found in the assistance to these patients, reflected on the professional practice in the sector in order to facilitate the care and guarantee the appropriate assistance to the user12.
METHODOLOGY
This is a descriptive research with a qualitative approach. Participants were 41 workers from the hemodialysis service, located in the city of Recife, which is areference in nephrology in the state of Pernambuco. Sampling was of intentional, in which all health workers in the hemodialysis sector of the referred service were included, excluding non-permanent staff members and those removed from the service for personal or professional reasons.
The data collection took place from May to July 2014, in a place reserved at the institution itself, with the guarantee of confidentiality and the privacy of the information given. Participation was conditioned to acceptance of the terms of the research and to signing of the Informed Consent Form (ICF). The interviews were recorded using a digital recorder and a semi-structured script was used, composed of objective questions to delineate the socioeconomic profile of the worker, addressing the variables age, sex, professional category, length of work in the service, specializations studied, number of employment ties and workload, in addition to three guiding questions: in your opinion, which factors interfere, positively and negatively, in the patient's adherence to hemodialysis? What do you do to facilitate patient adherence to hemodialysis? How does the lack of adherence to this therapy interfere with your professional performance?
The interviews were transcribed in a text editor and read in full for initial comprehension of the content. Subsequently, the interviews were formatted according to the requirements of the Analyse Lexicale par Contexte d'um Ensemble de Segments de Texte (ALCESTE), version 2010.
The next step in the formatting of the text was the identification of the corpus (formatted text) until its processing that culminated in the division of the elementary context units (ECU), which composed a reduced dictionary. After separation in thematic blocks, they went through continuous divisions until they did not result in new classes.
The ready classes are composed of radical forms of the words of the text, associated with their respective incidence and frequency values (Q2) in addition to the semantic context of each class13. Thus, ALCESTE performed the statistical analysis of the data and allowed extracting structures with representative meanings through the relationship with the léxicon, and the researcher was able to make available the real meaning of the information in the context and to name the classes presented in the analysis. Grouped according to the content revealed by the four classes, they were entitled: Professional-patient bond as support in the initial difficulties of the treatment; Knowledge of the renal patient about the disease and its treatment as a strategy for adherence; Depersonification of the subject associated with the deficit of knowledge and fear in the implantation of the catheter; Patient, family and professionals as an alliance in the promotion of self-care. In addition, each subject was assigned a pseudonym (P01, P02, P03) as a way to protect the identity of the professional when they are cited in speech extracts.
The present study respects the basic references of bioethics: autonomy, non-maleficence, beneficence and justice, being in line with resolution 466/12 and approved by the Ethics Committee of the institution, under the number of the Certificate of Presentation for Ethical Appreciation (CAAE): 28265814.5.0000.5197 and protocol no. 634,593 of May 5, 2014.
RESULTS AND DISCUSSION
Characterization of the sample
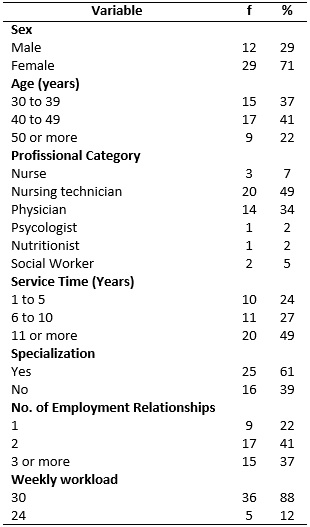
Of the total number of professionals in the study (n = 41) at the time of collection, 29 (71%) were female, 17 (41%) were in the age group 40-49, 20 (49%) had been working in the service for eleven years or more and 25 (61%) had a specialization in nephrology or in the hospital area. These data corroborate with another study, where the predominance of the female gender also occurred, the mean age was close to 40 years old and the mean working time in the hemodialytic unit was 10 years14.
Professional training is still a gap between the interviewees, since 16 (39%) do not have any specialization in the area. As for the quantity of employment relationships, 17 (41%) work in two institutions and 15 (37%) have three or more jobs. Regarding the weekly workload, 36 (88%) work 30 hours and 5 (12%) work 24 hours (Table 1).
TABLE 1:
Profile of health professionals working in a public hemodialysis service.
Recife, Brazil, 2014.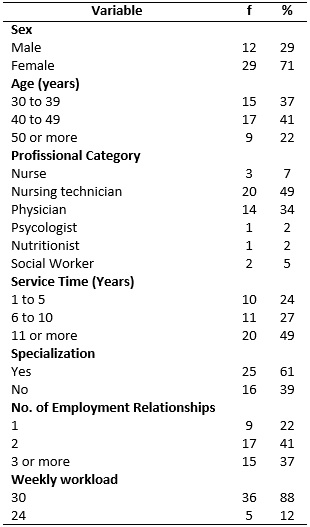
The analysis of the Alceste report identified 173 ECUs that made possible the formation of four classes, in which class 1 with the highest amount of ECU, as shown in Figure 1.

FIGURE 1:
Division of ECUs per speech classes of health professionals working in a
public hemodialysis service. Recife, Pernambuco,Brasil, 2014.
The classes presented in Figure 1 show the reduced forms and their frequencies (Q2). These nuclei, read within the context of the lines and grouped according to the content they reveal, allowed the construction of four thematic axes, listed and distributed below.
Professional-patient bond as support in the initial difficulties of the treatment
In the view of professionals, patients, at the beginning of hemodialysis, undergo obstacles imposed by CKD, such as the need to change habits, continuous use of various medications, coexistence with other people, routine and dependence on the hemodialysis machine. There is also the fear of the new, anxiety and uncertainty about the disease15.
Adhering is related to this process of discovery and acceptance of treatment; it is at this point that the multidisciplinary team with a good relationship with the patient are pointed as support for adherence16. This can be explained through testimonials:
It is not common, at the very beginning, that they know about the disease, because they come feeling very bad, but then they get better [...]. (P03)
We have a very good relationship, I think this also contributes a lot. Love in the relationship between the professional and the patient, makes them accept the conviviality here. (P04)
We have a nurse, a team of nursing technicians, a social worker and a nutritionist, that somehow makes them believe, they see that the service is commited. (P05)
The patient arrives at the dialysis center and discovers that he will have a social life, it starts to be easier. The difficulty is in the first moment, but they end up adapting to the new structure of life and I try to see what I can do when they arrive, to welcome them. (P12)
Multiprofessional presence and support comfort the patient and is a coping strategy, being a stimulating factor in adherence to treatment in the view of the service workers17. Therefore, welcoming the patient is essential at all times, especially in the first hemodialysis sessions.
Knowledge of the renal patient about the disease and its treatment as a strategy for adherence
The hemodialysis procedure demands increasing attention from the health professional throughout the session. Nursing works focused on patient care, an activity that has a high level of requirement, as well as technical ability of the dialysis procedure and specific knowledge regarding the functioning of the machine and immediate action in case of intercurrences and problem-solving18.
This specific knowledge should be used in the monitoring and especially in the guidelines to the patient and the family about the whole treatment process. However, the lack of knowledge and guidance to these patients is pointed out as one of the main points of non-adherence of the chronic renal disease in the service, according to the testimony of some professionals:
The negative point is the lack of information; many enter without knowing what it is, how it happens [...] The positive aspect is when they have knowledge on the need for treatment, knowledge of improvement of the quality of life. (P01)
A factor that interferes positively is to clarify the patient regarding the treatment so that he can be well aware of his illness. (P32)
The patient adheres better when he is aware of the treatment, knows data on the treatment, helps, participates in his treatment, is more active, has greater knowledge. (P18)
To do so, it is necessary to implement and structure an educational process, in addition to attention to approach in order to avoid misunderstandings and using strategies to obtain the expected behavior and adequacy of the information to the comprehension capacity of the subject.
In this way, it is the responsibility of each team member of the team to develop their specific duties, to better manage their professional interventions through dialogue and health education, to plan educational actions with a focus on particularity and to stimulate the autonomy of each individual assisted in the search for ideal health conditions19.
Depersonification of the subject associated with the deficit of knowledge and fear in the implantation of the catheter
Communication has a crucial role in the adaptive process and in the adequacy of the patient throughout the therapeutic development. Sensitivity to subjective perceptions in the professional approach in the first contact with patients is an important aspect to be considered. It is the responsibility of all team members, but this responsibility constantly relies on the doctor or nurse10 as shown in the testimonials:
Clarification is a negative point; they throw the patient in a room and pass the catheter, explain nothing, nor say what will happen, as if it were an object. First, if we correct the negative point, it can lead to greater adherence, the patient may understand what is happening because they get a little crazy, do not understand what is going on. (P21)
I know that when we enter the room for catheter implants we see the fear on their faces; many are in the first hemodialysis. The doctor does not guide what is going to happen at that moment. Sometimes, before the doctor arrives I have already guided them, because the doctor arrives and does not guide. (P04)
I see that most of them give explainations, but sometimes the patient does not even know the reason for the catheter, what will be done there, how his routine will be like. They arrive frightened, as if they could not do anything and life would end there. (P37)
The catheter implant is a shock to the patient by the fear of the procedure itself or for understanding the functional incapacity of their body or the rupture of the self-image. Altering the self-image, and the care associated with the use of the catheter create an unfavorable feeling for the patient, which leads to fear, feeling of anguish and consequent isolation16.
The interviews showed that the team is not ready to deal with the moment of catheter implantation and, therefore, there is a need to elaborate, structure and standardize an approach to this procedure, and to organize and delegate to each employee his/her responsibility in the welcome in order to help the patient to reduce the anguish, aiming to make them understand and deal with the renal problem20.
To guarantee the quality of care we need to welcome the user in matters not directly related to therapy. Comprehensiveness should be part of health care so that the professional knows the users' needs. It is necessary to understand the patient in his longings, complaints, doubts and develop skills for a humanistic atitude. Listening is the basis of good care and the professional should not be restricted to performing procedures but to welcoming, listening and respecting each subject21,22. Another indispensable aspect is the internal environment and the working conditions in which these professionals carry out their activities, which must be healthy to favor the work process and make it as ideal as possible.
Patient, family and professionals as an alliance in the promotion of self-care
The hemodialysis treatment involves the whole social and family contexto in which the individual is inserted. It also includes the contexto of the dialysis clinic where the professional team always works with the same patients who attend the service, usually every other day, for several years. An affective bond is created, which makes it possible to know the life stories, but it is capable of generating ambiguity of feelings, on the one hand recognition and affection, and on the other, the wear and tear resulting from the coexistence in situations of physical and emotional frailty23. This fact can be evidenced in the following excerpt in which the professional talks about the feelings generated about the non-adherence to the treatment:
It interferes because it generates that feeling of impotence. We guide, say, treat, prescribe, recommend medication, repeat the medication and the patient is not doing the treatment; this generates a frustration and we feel impotent (P40).
In the perception of health professionals, the active family, interested in the treatment, is another factor emphasized in speeches as relevant to adherence:
It ends up doing things because we are asking there, the patient's family is so present there that they end up being more forward, whether or not this issue of the family present in the system, encouraging. (P05)
However, The CKD imposes a substantial change in the family dynamics. It requires a decision-making and strategies to provide shelter to the patient both emotionally and financially to accompany them in their therapeutic itinerary. This partnership strengthens the connection between family/patient and health service/professionals, serving as a stimulus for therapeutic adherence20. It is possible to observe that the professional recognizes himself/herself and the family as self-care agents, according to testimony:
We keep insisting that the patient can do what we want him to do. The medical and the nursing, multidisciplinary team, is going through this to add and make it better themselves. (P40)
It is appropriate to consider that the bond with family members and professionals contributes as tools for the user to develop self-care and to make them aware of their role as a promoter of therapeutic success24,25. It is necessary to bring professionals, patients and family members closer together, to stimulate the formation of groups and to value collective, playful and multiprofessional actions to favor the creation of bonds in the elaboration of possible and satisfactory therapies26.
CONCLUSION
The chronic renal patient on hemodialysis encounters several obstacles to adherence. Investigating the factors that interfere in the adherence to this treatment, with a focus on the professional performance enabled verifying that communication, guidance, family and reception are key points to therapeutics.
The internal environment of the institution is another indispensable aspect for care. It must be healthy and working conditions should be the best possible for professionals to carry out their activities.
It is hoped that this study may subsidize professionals working in hemodialysis services to create norms and routines in the multidisciplinary approach to improve the quality of work and life of all staff.
As limitations of this study, the qualitative approach has low power of generalization of the findings, considering the sociodemographic particularities. However, studies about perceptions and in the care environment are important for the elaboration of interventions with the individuals involved and the understanding of realities similar to those described. It is also recommended to carry out further studies in this area with the cut of the professional categories in order to organize the care model according to the area of performance and the results can be used in the specific training of the professional.
REFERENCES
1.Siviero P, Machado CJ, Rodrigues NR. Chronic Renal Disease: An aggravation of increasing proportions in the Brazilian population. Belo Horizonte: UFMG/CEDEPLAR [Internet], 2013 [cited 2017 Dec 19]; 17p. Available from: http://www.cedeplar.ufmg.br/pesquisas/td/TD%20467.pdf
2.Ribeiro PRS, Batista TS. Adherence to antihypertensive drug treatment of hemodialysis patients. Rev ciênc farm básica Apl [Internet]. 2010 [cited 2017 Dec 19]; 36(2): 201-12 Available from http://seer.fcfar.unesp.br/rcfba/index.php/rcfba/article/view/233/137
3.Lins SMSB, Leite JL, Godoy S; Fuly PSC, Araújo STC; Silva IR. Validation of the adherence questionnaire of the Brazilian chronic renal patient on hemodialysis. Rev. bras. enferm. [Internet]. 2017 [cited 2017 Dec 19]; 70(3): 585-92. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&nrm=iso&lng=pt&tlng=pt&pid=S0034-71672017000300558
4.Lima-Dellamora EC, Osorio-de-Castro CG, Madruga LGSL, Azeredo TB. Use of medication dispensing records in adherence measurement: critical literature review. Cad Saúde Pública [Internet]. 2017 [cited 2017 Dec 19]; 33(3): e00136216. Available from: https://scielosp.org/scielo.php?script=sci_arttext&pid=S0102-311X2017000302001
5.Madeiro AC, Machado PDLC, Bonfim IM, Braqueais AR, Lima FET. Adherence of chronic renal failure patients to hemodialysis treatment. Acta Paul Enferm [Internet]. 2010 [cited 2017 Dec 19]; 23(4):546-51. Available from: http://dx.doi.org/10.1590/S0103-21002010000400016
6.Girotto E, Andrade SM, Cabrera MAS, Matsuo T. Adherence to pharmacological and non-pharmacological treatment and associated factors in the primary care of hypertension. Ciênc Saúde Coletiva [Internet]. 2013 [cited 2017 Dec 19]; 18(6): 1763-72. Available from: http://dx.doi.org/10.1590/S1413-81232013000600027
7.Trepichio PB, Guirardello EDB, Duran ECM, Brito AP. Profile of patients and nursing workload in the nephrology unit. Rev Gaúcha Enferm[Internet]. 2013 [cited 2017 Dec 19]; 34(2): 133-9. Available from: http://dx.doi.org/10.1590/S1983-14472013000200017
8.Fonseca PP, Oliveira MDG, Del Porto JA. A questionnaire to evaluate the impact of chronic diseases: validated translation and Illness Effects Questionnaire (IEQ) reliability study. J Bras Psiquiatr[Internet]. 2012 [cited 2017 Dec 19]; 61(11): 181-4. Available from: http://dx.doi.org/10.1590/S0047-20852012000300010
9.Sgnaolin V, Prado AE, Figueiredo L. Adherence to pharmacological treatment of hemodialysis patients. J Bras Nefrol [Internet]. 2012 [cited 2017 Dec 19]; 34(2): 109-16. Available from: http://dx.doi.org/10.1590/S0101-28002012000200002
10.Campos CJG, Turato ER. Hemodialytic treatment from the perspective of the renal patient: qualitative clinical study. Rev bras enferm [Internet]. 2010 [cited 2017 Dec 19]; 63(5): 799-805. Available from: http://www.scielo.br/pdf/reben/v63n5/17.pdf
11.Araujo LPR, Figueiredo AEPL, D' Avila DOL. Evaluation of teaching-learning program on calcium and phosphorus metabolism for hemodialysis patients. Rev esc enferm USP [Internet]. 2010 [cited 2017 Dec 19]; 44(4); 928-32. Available from: http://dx.doi.org/10.1590/S0080-62342010000400010
12.Waidman MAP, Radovanovic CAT, Estevam MC, Marcon, SS. Assistance to the person with hypertension from the perspective of the health professional. Rev bras enferm [Internet]. 2012 [cited 2017 Dec 19]; 65(3): 445-53. Available from: http://dx.doi.org/10.1590/S0034-71672012000300008
13.Nascimento ARA, Menandro PRM. Lexical analysis and content analysis: a proposal of conjugated use. Estud e Pesqui em Psicol [Internet]. 2006 [cited 2017 Dec 19]; 6(2): 72-88. Available from: http://www.revispsi.uerj.br/v6n2/artigos/pdf/v6n2a07.pdf
14.Ummann J, Guido LDA, Silva RM. Stress, coping and presenteism in nurses who attend critical and potentially critical patients. Rev esc enferm USP [Internet]. 2014 [cited 2017 Dec 19]; 48(5):891-8. Available from: http://dx.doi.org/10.1590/S0080-6234201400005000016
15.Costa CA, Candido KJ, Filho AM, Souza-Lemos C. End-stage renal disease on hemodialysis: change in habits and bone disease. Rev Eletrônica Novo Enfoque [Internet]. 2013 [cited 2017 Dec 19]; 17(17): 196-201. Available from: http://www.castelobranco.br/sistema/novoenfoque/files/17/29-artigo-pibict-27092013.pdf
16.Fortes VLF, Bettinelli LA, Pomatti DM, Brock J, Dobner T. The itinerary of chronic kidney disease: from foreshadowing to discovery. Rev RENE [Internet]. 2013 [cited 2017 Dec 19]; 14(3):531-40. Available from: http://www.repositorio.ufc.br/handle/riufc/11624
17.Santana SS, Fontenelle T, Magalhães LM. Nursing care provided to patients on hemodialysis treatment in nephrology units. Rev Científica do ITPAC [Internet]. 2013 [cited 2017 Dec 19]; 6(3). Available from: https://www.itpac.br/arquivos/Revista/63/5.pdf
18.Lima AFC. Direct cost of conventional hemodialysis monitoring performed by nursing professionals. Rev bras enferm [Internet], 2016 [cited 2017 Dec 18]; 70(2): 374-81. Available from: http://www.scielo.br/pdf/reben/v70n2/pt_0034-7167-reben-70-02-0357.pdf
19.Radovanovic CAT; Bevilaqua CA; Molena-Fernandes CA; Marcon SS. Multi-professional intervention in adults with hypertension: randomized clinical trial. Rev bras enferm [Internet]. 2016 [cited 2017 Dec 18]; 69(6): 1067-73 Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672016000601067
20.Barretto MS, Marcon SS. Chronic kidney disease: experiences and expectations of the caregiver. Rev enferm UERJ [Internet]. 2012 [cited 2017 Dec 18]; 20(3): 374–9. Available from: http://www.e-publicacoes.uerj.br/index.php/enfermagemuerj/article/view/2193/2886.
21.Teixeira RB, Resck ZMR. The feelings of the patients assisted with recreational activities during the hemodialysis session. Rev RENE [Internet]. 2011 [cited 2017 Dec 18]; 12(1): 120–6. Available from: http://www.revistarene.ufc.br/vol12n1_pdf/a16v12n1.pdf
22.Moimaz SAS, Lima AMC, Garbin CAS, Corrente JE; Saliba NA. Patient assessment on dental care in the Unified Health System: an approach based on the humanization. Ciênc. saúde coletiva [Internet]. 2016 [cited 2017 Dec 19]: 21(12): 3879-87. Available from: https://scielosp.org/scielo.php?script=sci_arttext&pid=S1413-81232016001203879
23.Prestes FC, Beck CLC, Tavares JP, Silva RM, Cordenuzzi OCP, Burg G, et al. Perception of nursing workers on work dynamics and patients in a hemodialysis service. Texto contexto enferm [Internet]. 2011 [cited 2017 Dec 19]; 20(10): 25-32. Available from: http://dx.doi.org/10.1590/S0104-07072011000100003
24.Seleghim MR, Marangoni SR, Marcon SS, Oliveira MLF de. Family link of crack users seen at a psychiatric emergency unit. Rev Latino-Am Enfermagem [Internet]. 2011 [cited 2017 Dec 19]; 19(5): 1-8. Available from: http://dx.doi.org/10.1590/S0104-11692011000500014
25.Zolfaghari M, Asgari P, Bahramnezhad F, Rad SA, Haghani H. Comparison of two educational methods (family-centered and patient-centered) on hemodialysis: related complications. Iran J Nurs Midwifery Res [Internet]. 2015 [cited 2017 Dec 19]; 20(1): 87-92. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4325420/
26.Figueira TR, Davis NA, Morais MN, Lopes ACS. Perception about adoption and counseling of healthy lifestyles by health professionals. Trab educ saúde [Internet]. 2014 [cited 2017 Dec 19]; 13(1). Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1981-77462015000100181