ORIGINAL RESEARCH
Home ambience for peritoneal dialysis
Ana Cristina Freire AbudI; Maria Lúcia ZanettiII; Ana Dorcas de Melo InagakiIII; André Faro SantosIV; Raíssa Santana LimaV; Renata Pinto Moura VI
I
PhD in Nursing. Nurse. Adjunct Professor, Federal University of Sergipe.
Department of Nursing. Aracajú, Sergipe, Brazil. E-mail: acfabud@uol.com.br
II
PhD in Nursing - Lecturer. Nurse. Associate Professor, University of São
Paulo. Ribeirão Preto, São Paulo, Brazil. E-mail: zanetti@eerp.usp.br
III
PhD in Medical Sciences. Nurse. Adjunct Professor, Federal University of
Sergipe, Department of Nursing. Aracajú, Sergipe, Brazil. E-mail: ana-dorcas@hotmail.com
IV
PhD in Psychology. Psychologist. Professor, Department of Psychology,
Federal University of Sergipe. Aracajú, Sergipe, Brazil. E-mail: andre.faro@yahoo.com.br
V
Nurse. Municipal Secretariat of Health of Nossa Senhora da Glória. Sergipe,
Brazil. E-mail: raissasantanaa@hotmail.com
VI
Nurse. Federal University of Sergipe. Department of Nursing. Aracajú,
Sergipe, Brazil. E-mail: renatappinto@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2017.15210
ABSTRACT
Objective: to investigate the physical structure of homes of patients undergoing peritoneal dialysis. Method: in this quantitative, cross-sectional study of 90 peritoneal dialysis patients, data was collected by interview and direct observation at their homes. The study was approved by the ethics committee (CAAE 0310.0.107.000-11). The 'Structure' component of health care assessment was used for the analysis. Results: most of the patients were older adults, male, with little schooling and low income. Peritoneal dialysis was performed mostly in the bedroom, where walls were intact and ceilings, lined. Cracked were observed in floors (4.4%), and cracks and damp, in walls (15.6% and 11.1%, respectively). Most of the houses had bedroom sinks for hand hygiene (76.6%), treated water (87.8%), appropriate storage for material (73.3%) and sewerage (76.7%) where waste was discharged. Conclusion: the 'Structure' component revealed patients exposed to risks that might aggravate their health condition.
Keywords: Renal insufficiency chronic; peritoneal dialysis; home nursing; nursing care.
INTRODUCTION
Chronic kidney disease (CKD) is a worldwide public health problem. In the United States, in the period from 2009 to 2010, the population with CKD grew by 4%1. The worsening of this disease leads to end-stage chronic renal failure (ESCRF), with the possibility of need enrolling in a renal replacement therapy (RRT) program, either hemodialysis (HD), peritoneal dialysis (PD) or renal transplantation.
In Brazil, the number of patients undergoing dialysis increased from 112,004 in 2014 to 122,825 in 20162,3. Regarding the modality of RRT, in 2016, 92% of patients were on hemodialysis and 8% on PD3 .
PD is considered an efficient renal replacement therapy method for removal of fluid and degradation products in uremia. The use of safe materials and biocompatible solutions coupled with the development of cycling machines has promoted important results over the years in relation to the effectiveness of dialysis, comfort and patient safety. Although advances have been made, variables such as the socioeconomic level of the family, hygiene conditions and schooling of the caregiver are fundamental aspects in the efficacy of treatment4,5.
PD is characterized as a treatment modality with similar results to HD and has several advantages, among them the improvement of the quality of life of patients. However, problems such as peritonitis, inadequate ultrafiltration and deficient elimination of uremic solutes as well as social factors may be an indication for the need to switch from PD to HD. This indication has been observed mainly when there is a decline in residual renal function6.
National and international publications have directed the investigative focus of PD to the complications related to the use of the peritoneal catheters, among them peritonitis, a complication recognized in the world as one of the major causes of patient withdrawal from PD programs. Other described complications are feelings of distress and physical pain related to personal and social limitations arising from the disease and treatment. Since 1996, several studies on peritonitis have been published addressing the guidelines for prevention, diagnosis and treatment7,8. However, little has been published about the home ambience for PD, which may be a factor that contributes to complications.
It is recognized that patients face difficulties with the insertion in dialysis programs extending to the home setting, where the procedures are performed without the direct supervision of the health team. In view of the above, this study aimed to evaluate the physical structure of the domicile of patients undergoing PD. We hope that the results provide subsidies for the safe practice of care in relation to the ambience in which PD occurs.
THEORETICAL FRAMEWORK
The use of PD was started in 1923 with the infusion of saline solution into the peritoneal cavity in patients with chronic renal failure (CRF), and in 1962 this method was applied in CKD patients. Over the years, PD has improved, making the technique easier and safer and with reduced incidence of complications. This evolution made PD a dialysis method equivalent to hemodialysis, representing an alternative treatment for CKD patients 4.
Continuous exposure of the peritoneal membrane to conventional solutions containing high glucose concentrations, low hydrogenation potential (pH) and high osmolarity in the long term causes damage to the peritoneum. This inflammatory effect has been reduced with the use of new solutions containing less glucose degradation products (GDP), neutral pH, lactate, bicarbonate with lactate, or bicarbonate alone9. Regarding peritoneal catheters, these are made of silicone or polyurethane, with one or two Dacron cuffs and several pores at the extremity. The cuffs have the purpose of promoting the formation of granulation tissue and fibrosis, allowing the fixation of the catheter and preventing bacterial migration into the peritoneum, thereby reducing the chances of peritonitis 10.
After the initiation of the therapy, follow-up occurs through monthly medical consultations and nursing follow-up, through nursing consultations and home visits4,11. The health team, represented by a physician, a nurse, nursing technicians and assistants, a psychologist, a nutritionist and a social worker, plays a fundamental role in the continuous assistance to patients undergoing PD. When care is provided by a multiprofessional team, the chance of adherence to therapy is greater 12,13. Educational activities are primary factors in the management of renal disease. When well planned, they contribute to reduce complications that may arise during the course of treatment. It is known that CKD causes significant changes in the patients' daily life, leading them to seek ways to adapt to their new life condition14. The main goal of the health team is to maintain and improve the quality of life of CKD patients.
In this aspect, all efforts should be directed to avoid complications due to therapy. However, infectious complications are frequent4.
To evaluate the home structure component, a health care assessment was carried out grounded on the theoretical framework proposed in 1980, based on the concepts of three basic elements related to the General System Theory15.
This benchmark allows the evaluation of the quality of care provided, since it involves all the activities carried out between health professionals and patients15. The author proposes three concepts for health assessment: structure, process and outcome. The structure refers to the physical, human, material and financial resources needed for medical care. The process consists in the protocols established by the institution in which the activities developed by the professionals and those performed by the patients are described. This analysis may occur from a technical and/or administrative point of view. And finally, the outcome is related to the final product of the care provided and must consider the satisfaction pattern and the expectations of the professionals and patients involved in the institution15.
In this study, we sought to evaluate the physical structure of the domiciles of patients who perform home PD. The choice of this theoretical framework made it possible to identify the factors related to the physical structure of the home environment that interfere with the care of patients undergoing PD.
METHODOLOGY
This is a cross-sectional quantitative study performed with all adult peritoneal dialysis patients attended at a clinic serving the Unified Health System in the State of Sergipe.
To obtain the data, we initially analyzed all medical records. Based on these documents, 90 patients who had been under PD for at least 6 months and who were aged 18 years or over were selected for the study. After the patients were selected, the researchers made a telephone contact to schedule the visit. The visit was scheduled 24 hours before the interview in order to avoid time for changes in the home environment.
Data were collected from November 2011 to July 2012, after approval of the study project by the Research Ethics Committee of the Federal University of Sergipe under CAAE 0310.0.107.000-11, in accordance with Resolution 466/2012. For this purpose, a semi-structured questionnaire with open and closed questions on variables related to the physical structure of the home and socio-demographic aspects (gender, age, schooling and income) was used. The interviews and observations lasted up to 40 minutes on average.
Direct observation of the environment favored the collection of data regarding the realization of the dialysis procedure. The following aspects were observed: walls, floor of the place where the solution was exchanged, sink for hand hygiene, piped water system and sanitary sewage, conditioning of the material and place used to dispose the dialysate effluent. The structural component of health care assessment was used in the analysis.
RESULTS AND DISCUSSION
From 90 home PD patients, 41 (45.5%) were older than 60 years. Morphofunctional aspects such as decreased thickness of the renal cortex and reduced renal plasma flow are some factors that trigger CKD in the elderly9, justifying the high frequency of this age group in the study. In addition, therapeutic and technological advances in the treatment of chronic diseases have increased life expectancy, contributing to the growth of the elderly population.
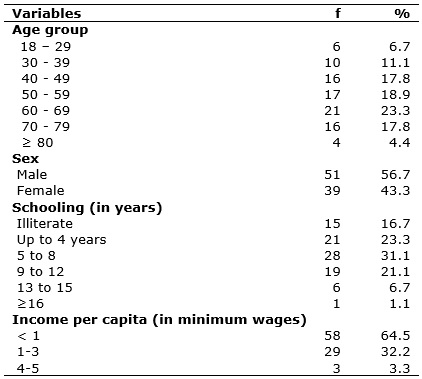
Regarding sex, 51 (56.7%) participants were men, as shown in Table 1. This finding corroborates a study carried out in the Southeast Region 16. The 2014 census on dialysis revealed that 58% of renal replacement therapy patients were males2.
TABLE 1:
Distribution of patients undergoing home peritoneal dialysis according to
socio-demographic variables. Sergipe, 2012. (N = 90).
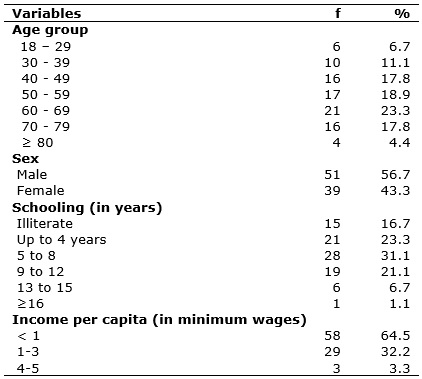
Regarding schooling, 28 (31.1%) participants had 5 to 8 years of schooling, constituting the predominant group. National research data show that, the proportion of 15-17 year–old young people attending schools increased by 2.7 per cent in 10 years, from 81.5 per cent in 2002 to 84.2 per cent, in 201217, showing that there was a growth, albeit small, in the access to the Brazilian educational system in the last decade. Thus, much still needs to be done to improve basic education.
With regard to per capita income, the majority of participants - 58 (64.5%) - received less than one minimum wage, as shown in Table 1. These finding indicates that the majority of the study population was in the economy class classified as low. It is important to take into account the bidirectional relationship between poverty and chronic diseases, since poverty can lead to chronic diseases, but also chronic diseases can lead to poverty in result of the expenses incurred by the treatment, lack of income, and marginalization due to the patients' precarious situation 18. Low income also causes difficulty to access health services, adequate nutrition, transportation, pharmacological items and dialysis treatment, worsening the quality of life19. However, socioeconomic and cultural characteristics do not constitute a limitation for the indication of PD.
Regarding treatment time, 27 (30%) patients were in the first year of PD, 29 (32.2%) had been for 1 to 3 years under treatment, and 12 (13.3%) from 3 to 5 years. Only 22 (24.5%) had been enrolled in a PD program for more than 5 years. The high mortality rate and the presence of complications have been referred as reasons for the abandonment of PD programs. The BRAZPD study showed that patients from the Southeast of Brazil remained on average 12.3 months in treatment, and those in the Midwest Region, 8.9 months 20.
In order to evaluate the home environment, the areas where the following procedures were conducted were considered: dialysis, storage of material and hand washing. For the effectiveness of the PD procedure, 89 (98.9%) patients used the bedroom. As for the integrity of the walls, the presence of intact walls was found in the case of 66 (73.3%) houses, cracks were seen in 14 (15.6%) houses, and infiltrations in 10 (11.1%) houses, as shown in Table 2.
TABLE 2:
Distribution of variables related to the physical structure of the home
ambience. Sergipe, 2012 (N = 90).
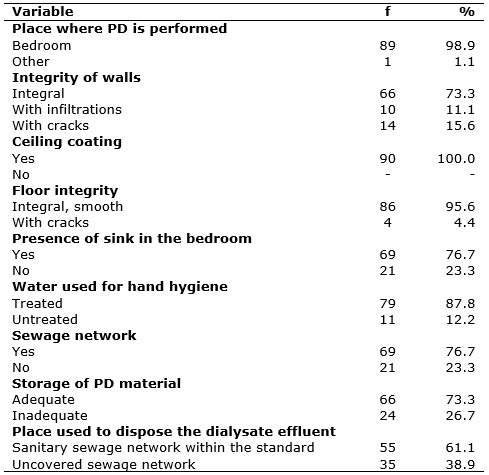
Concerning the ceiling conditions, it was found that 90 (100%) households were protected with various materials, such as polyvinyl chloride (PVC), slab, plaster and wood. It is important to point out that the presence of infiltrations causes mould due to the presence of microorganisms belonging to the fungi group21.
Regarding the quality of the flooring, most of the bedrooms - 86 (95.6%) - had preserved, smooth and intact flooring. However, the presence of cracks was found in 4 (4.4%) of them, as shown in Table 2. The integrity of the floor is one of the ambience-related recommendations for the performance of the procedure under study, due to the ease of cleaning for prevention of infections.
Careful diagnosis of the housing conditions for the realization of home PD has as purpose the safety of the patients. Inadequate environmental conditions, such as lack of hygiene, inappropriate physical space, presence of dust, mildew, low luminosity, untreated water, humidity or environment under construction, have been pointed out by caregivers as possible determinant failures leading to home PD complications5,13. In a study carried out in Rio de Janeiro, the packaging of materials was also a reason for concern in the case of patients who, for the most part, lived in small environments14. It is up to the nurse to guide the families, patients and caregivers in the construction or adaptation of suitable spaces for home dialysis to avoid possible complications.
Regarding the water used by patients and/or caregivers, for hand hygiene and body hygiene, it was found that in most households - 79 (87.8%) - water came from the Sanitation Company (DESO). On the other hand, water from an artesian well was also found in 11 (12.2%) domiciles. In 8 (72.7%) of these houses, the water taken from the artesian well was used after boiling, while in three (27.3%) houses, they used water in improper conditions for human consumption. It should be noted that, during body hygiene, patients perform the hygiene of the site of insertion of the catheter. According to Ministry of Health Ordinance nº 2914 of December 12, 2011, appropriate water for human consumption is defined as drinking water intended for ingestion, preparation and production of food and personal hygiene, regardless of its origin22.
Regarding the presence of sanitary sewage networks, it was observed that sewage network according to basic sanitation standards was present in 69 (76.7%) houses, , and uncovered sewage was found 21 (23.3%) houses. It is known that untreated water and exposure to sewage favor the spread of diseases. The provision of sewage and potable water is the responsibility of the State, and it is up to the population to claim these rights.
Regarding the presence of sinks for hand hygiene, it was found that in 69 (76.7%) domiciles there were sinks in the bedroom, near the place for the dialysis procedure, in order to reduce the risk of contamination of the material, favoring hand hygiene immediately before and after the procedure. It was also verified that patients and caregivers used sinks outside the bedroom for hand hygiene in 21 (23.3%) houses. This factor may increase the risk of infectious complications, since external sinks are also used by other family members and for other purposes. Depending on the distance between the room and the sink located outside it, there is a risk of hand contamination during the journey. This risk is reduced when hand hygiene is performed at the site where the procedure is conducted.
As for the storage of the boxes containing the bags with solution used in the PD, 66 (73.3%) patients stored them as recommended, that is, lying on a support and away from the wall. In the case of 24 (26.7%) patients, the boxes were placed directly on the floor. This corroborates a study carried out in Minas Gerais with 30 children and adolescents undergoing PD and their caregivers, where one of the difficulties experienced by families was the lack of space for storage of the dialysis solution bags5. It was also found that in 10% of the houses there was no sink in the room for hand hygiene, besides problems regarding the disposal of the effluent in the sewer or toilet, among others, and the inadequacy of the dialysis technique in 60% of the cases5.
Regarding the site used to dispose the dialysate effluent from the abdominal cavity, 55 (61.1%) patients used the sanitary sewage network, and 35 (38.9%) used the drainage network outside the standards of sanitation. Resolution 306 of December 7, 2004, issued by the National Sanitary Surveillance Agency and the Resolution of the National Environmental Council (CONAMA) nº 358 of April 29, 2005, determine that biological waste must be thrown in a basic sanitation network13,23.
CONCLUSION
The structure-related component evidences that the most used environment for home PD was the bedroom, with the majority presenting intact walls, ceiling coating, intact floor, presence of sink, and use of treated water for hand hygiene, and sewage network. In addition, patients stored the PD materials in an adequate manner and place. However, in some cases, cracks, infiltrations and the use of water from artesian wells were observed, as well as improper storage of the material and incorrect disposal of the dialysate effluent, exposing patients to risks that may aggravate their health status.
The limitation of this study is that it was performed with patients from only one dialysis clinic in the State of Sergipe, although four clinics perform this procedure. However, this does not compromise the relevance of the findings, once they portray the reality of the cases served, providing subsidies for further studies that represent the universe of the phenomenon.
REFERENCES
1.Letsios A. The effect of the expenditure increase in the morbidity and the mortality of patients with end stage renal disease: the USA case. Hippokratia. 2011;15(suppl 1):16-21.
2. Sesso RCC, Lopes AA, Thomé FS, Lugon JR, Martins CT. Brazilian chronic dialysis survey 2014. J bras nefrol. 2016; 38 (1): 54-61.
3. Brazilian Society of Nephrology. Peritoneal dialysis in Brazil: current scenario and challenges. [Internet] 2016 [cited on Oct 21, 2017]. Available from: http://www2.camara.leg.br/atividade-legislativa/comissoes/comissoes-permanentes/cssf/arquivos-de-eventos/audiencia-publica-27-04.17/milena-daher-sbn
4.Pecoits-Filho R, Moraes TP. Peritoneal dialysis. In: Riella MC. Principles of nephrology and hydroelectrolytic disorders. 5th ed. Rio de Janeiro: Guanabara Koogan S. A; 2010. p.1032 - 46.
5.Abrahão SS, Ricas J, Andrade DF, Pompeu FC, Chamahum L, Araújo TM et al. Descriptive study on the practice of home peritoneal dialysis. J bras nefrol. 2010; 32 (1): 45-50.
6.Brown EA, Bargman J, Biesen WV, Chang M, Finkelstein FO, Hurst H et al. Length of time on peritoneal dialysis and encapsulating peritoneal sclerosis - position paper for ISPD: 2017 Update. Perit dial int. 2017; 37 (4): 362-74.
7. Szeto CC, Li PKT, Johnson DW, Bernardini J, Dong J, Figueiredo AE, et al. Peritoneal dialysis-related infections recommendations: 2017 update. Perit dial int. 2017; 37 (2): 141-54.
8.Sadala MLA, Bruzos GAS, Pereira ER, Bucuvic EA. The experience of patients under home peritoneal dialysis: a phenomenological approach. Rev Latino-Am Nursing. 2012; 20 (1): 1-8.
9.Poitevin AA, Viezzer C, Machado DC, Costa BEP, Figueiredo AE, D'Ávila D. The effect of peritoneal dialysis solution with neutral and standard pH on the proliferation of fibroblasts. J bras nefrol 2014; 36(2): 150-54.
10.Daugirdas JT, Blake PG, Ing TS. Manual of dialysis. 5th ed. Rio de Janeiro: MEDSi; 2016.
11. Figueiredo A, Bak-Leong G, Sarah J, David WJ, Robert M, Santhanam R, et al. Clinical practice guidelines for peritoneal access peritoneal. Perit dial int. 2010; 30 (4): 424-9.
12.Bastos MG, Kirsztajn JN. Chronic renal disease: importance of early diagnosis, immediate referral and structured interdisciplinary approach to improve the outcome in patients not yet undergoing dialysis. J bras nefrol. 2011; 33 (1): 93-108.
13.Ministry of Health (Br). National Health Surveillance Agency. Resolution - RDC nº 11 of March 13, 2014. It provides rules for good operating practices of dialysis services and provides other measures. Brasília (DF): ANVISA; 2014.
14.Tavares JMAB, Lisboa MTL. Peritoneal dialysis treatment: the practice of self-care in the family context. Rev Enferm UERJ. 2015; 23 (3): 344-49.
15.Donabedian A. Basic approaches to assessment: structure, process, outcome. In: Donabedian A.Exploration in quality assessment and monitoring. Ann Arbor: Health administration press; 1980. p. 77-125.
16.Scatolin BE, Vechi AP, Ribeiro DF, Bertolin DC, Canova JCM, Cesarino CB, et al. Daily life activity of patients undergoing intermittent peritoneal dialysis with cycler. Arq ciênc saúde. 2010; 17(1): 15-21.
17.Brazilian Institute of Geography and Statistics. Synthesis of social indicators: an analysis of the living conditions of the Brazilian population. [Internet] 2013 [cited on Oct 20, 2017]. Available from: https://biblioteca.ibge.gov.br/visualizacao/livros/liv66777.pdf
18.World Health Organization. Innovative care for chronic conditions: structural components of action: global report. Brasília (DF): WHO; 2003.
19. Frazão CMFQ, Ramos VP, Lira ALBC. Quality of life of patients undergoing hemodialysis. Rev Enferm UERJ. 2011; 19 (4): 577-82.
20. Fernandes NMS, Chaoubah A, Bastos K, Lopes AA, Divino-Filho JC, Pecoits-Filho R, et al. Geography of peritoneal dialysis in Brazil: analysis of a cohort of 5,819 patients (BRAZPD). J bras nefrol. 2010; 32 (3): 265-71.
21.Paz LAF, Costa LCA, Paula MO, Almeida WJB, Fernandes FAZ. Survey of pathologies caused by humidity in a building in the city of Palmas - TO. Reget/UFSM. 2016; 20 (1): 174-80.
22. Ministry of Health (Br). Ordinance no. 2914 of December 12, 2011. It provides rules on the procedures of control and monitoring of the quality of water for human consumption and its standard potability. Federal Legislation. Brasília (DF) [website] 2011 [cited on Oct 22, 2017]. Available from: http://site.sabesp.com.br/uploads/file/asabesp_doctos/kit_arsesp_portaria2914.pdf
23. National Environmental Council (Br). Resolution nº 306 of December 07, 2004. Brasília (DF): CONAMA; 2005.