ORIGINAL RESEARCH
Schoolchildren's eye health: nurses' role
Mayara Larissa Nilsen SchumaherI; Maria Elisabete Rodrigues Freire GasparettoII
I
Nurse; Master in Health, Interdisciplinarity and Rehabilitation.Ph.D.
students in Health Sciences, State University of Campinas. São Paulo,
Brazil. E-mail: mlnilsen@yahoo.com.br
II
Pedagogue.Ph.D. in Medical Sciences; Professor of the State University of
Campinas.São Paulo, Brazil. E-mail: gasparetto@fcm.unicamp.br
DOI: http://dx.doi.org/10.12957/reuerj.2016.15108
ABSTRACT
Objective : to train and accompany family health strategy nurses in investigating altered vision in first year primary school students. Method: in this cross-sectional study at five schools in a municipality in São Paulo State in 2011, after approval by the research ethics committee (CAAE: 0378.0.146.000-11), data were collected by seven specifically trained nurses using the Snellen Table and a data collection instrument. Results: the sample consisted of 143 students with mean visual acuity of 0.913 in both eyes. Signs of visual impairment were detected during the evaluation. A significant relation was found between visual acuity and the presence of symptoms (p ≤ 0.05). The nurses referred 38 (26.6%) of the students to the ophthalmologist. Conclusion: nurses demonstrated competence in performing the test, and guided clinical decision making, contributing significantly to early detection of altered vision, which could lead to student's repeating a year or dropping out.
Keywords : Visual acuity; eye health; school health; nursing.
INTRODUCTION
According to the World Health Organization (WHO), about 7.5 million children in the school stage have some visual changes, and only 25.0% of these children present symptoms, while the other 75.0% need of a specific test to identify the problem1. Also, more than 31% of the millions of Brazilians are enrolled in basic education, constituting a singular place for the elaboration of public policies for prevention and health promotion2,3.
Vision is one of the most relevant factors in school learning4. Therefore, activities aimed at the ocular health of schoolchildren need to be improved, highlighting the importance of expanding nurses´ actions to actions in the school environment. The intersectoral relationship between primary care and the school environment is a fertile environment for training future citizens5,6.
The ophthalmologic screening is easy to perform and reliable, and it should be part of programs in schools7. Through the performance of the visual acuity test in schoolchildren, the visual screening program is feasible, effective and it should have its place in school health programs, involving public and private teaching networks8.
Considering this and the importance of the nurse performance of the Family Health Strategy (ESF) in the school health area, this research proposed the objective of training and accompanying the nurse of the ESF in the investigation of visual change in students of the 1st grade of Elementary School.
LITERATURE REVIEW
In Brazil, there are programs and policies that demonstrate the importance of acting in the eye health of schoolchildren. Since 1989, the Hygiene Inspection Service was created, identified as one of the first governmental measures related to public health, and later extended to the school environment9.
In 1999, the Ministry of Education and the Brazilian Council of Ophthalmology developed the National Campaign for Visual Rehabilitation, entitled Eye-to-Eye Campaign, aimed at promoting visual health through the Visual Acuity Test using the Snellen Table10.
In Brazil, since December 5, 2007, the Ministry of Education and Health have established the Health in School Program (PSE) through Presidential Decree 6.286, in which priority is given to promotion, prevention, and health in the school area. Among the objectives of the PSE, ophthalmologic assessments are contemplated11-13. The Projeto Olhar Brasil was created to complement this program, with the target audience of students from schools linked to the PSE, and proposes to work in the identification and correction of vision problems in students enrolled in the public network, besides cases in which signs and symptoms of visual changes are detected14, the student should be referred to specialized services.
These evaluations should occur as early as possible since the child cannot be expected to express his or her difficulty in seeing because the number of children who can report this deficiency is very small15. This difficulty may interfere with learning and consequently in school performance4.
Many times, children in domestic environments do not have the dimension that they see badly because they do not perform activities requiring greater visual effort. When they enter the school, they present visual difficulty to see the blackboard and other academic activities; the students can be compared to the teachers, with the other classmates and, the visual difficulty can be confused with the disinterest or with shyness 15.
The use of the Snellen Table to test visual acuity is defined by the WHO as simple, reliable, high sensitivity and specificity, low cost and not requiring prolonged professional training16.
The teacher presents difficulties in identifying some symptoms, not only due to lack of knowledge in ocular health but also due to the lack of specific terminology such as nystagmus, photophobia, and head positioning 17.
The investigation of eye problems of schoolchildren by ophthalmologists becomes very expensive in mass examinations due to the lack of specialized resources, so the solution would be to apply the visual screening by nonmedical and trained personnel to the populations clustered in schools and social programs18.
Studies show that primary care to the individual performed by nurses is of great consideration for the prevention of visual changes, and their performance must become routine in health promotion19-22. This action is essential and an excellent alternative, because it has as routine, to carry out the household follow-up of the families, observing the reality and social and cultural situation of each member in school age, being able to encourage the adherence to the ophthalmological treatment.
This research used an evidence-based nursing proposal, looking for evidence that proves the visual changes of the students, through an examination performed by the nurse. The main evidence of visual changes was the visual acuity test, one of the main ocular functions. This evidence was also willing to provide evidence for decision-making (referral to specialized service).
METHODOLOGY
It is a cross-sectional analytical study, characterized as quantitative research23. The study complied with Resolution 196/96, and it was approved by the Research Ethics Committee of the State University of Campinas under the CAAE: 0378.0.146.000-11.
The research was conducted in the city of Limeira, in the interior of São Paulo, with a geographical area of 581.00 km2. In the year in which the data were collected, there were 50,099 schoolchildren enrolled in the municipality distributed at various levels of education. The city covers 10 ESF units.
As inclusion criteria were only the schoolchildren from the municipal schools that were located near the ESFs of the City of Limeira, as well as the nurses who worked on these ESFs and agreed to participate in the study by signing the Free and Informed Consent Form (TCLE). Students who were absent on the day of data collection and those whose parents refused to participate in the study and did not sign the TCLE were excluded from the study.
The study was carried out in 2011 in five municipal schools of the city of Limeira, with 143 schoolchildren and seven nurses from the ESFs selected. Initially, the researcher contacted the seven nurses who worked at the ESF, explaining the objectives and the importance of the study. It is necessary that there be an incentive to broaden and solidify the nurses' actions in school health actions through training, including visual acuity tests, periodically or at least annually5. The training program for nurses was started.
For this purpose, a meeting was held for approximately 1 hour and 30 minutes, in which the nurses received information about visual screening, training for the evaluation of visual acuity and the observation of signs and symptoms indicative of visual difficulty.
The nurses made occluders for the eyes and the letter E, presented to the students and used in a playful way to facilitate the performance of the evaluation of visual acuity.
An instrument was developed for the ESF nurses to apply to the students through an interview to collect the data based on the following variables: name, gender, and age of the student, identification of the school, school series, use of glasses, visual acuity values and symptoms presented during visual acuity assessment.
For the evaluation of visual acuity, the Snellen's Optometric Table, pointer or black pencil, letter E, occluder, chair, tape measure, tape and printed for the results annotation were used.
Subsequently, the contact with the principal and teachers explained the objectives and the importance of the study for the students. According to the teachers' guidance, the TCLE was sent in the notebooks of the students, along with an explanation of the study and the period the evaluations would be carried out.
There were ten days waiting for the receipt of the TCLE signed by the parents or guardians. It was verified that there was fear among the parents, because although the units of the ESFs had a schedule of action in the schools, rarely they were clarified to the relatives.
The data collection was carried out during the classes period of the students, between April and September of 2011, in the morning and evening shifts, by the researcher and the nurses of the ESFs, in a room with natural light and chosen strategically, in an area of the school without noises, in order to avoid mistaken results24. It was explained to the students how the test would be performed. The teachers sent four students each time, who were received by the nurses to fill out the instrument and to evaluate the visual acuity of the right eye (AVOD), the left eye (AVOE) and both eyes (AVAM).
The Snellen Table (ocular chart) was positioned at a distance of 6 meters from the child being examined24 to perform the visual acuity test and fixed it so the line 0.8 was at the same level as the eyes of the schoolboy. It was initially requested that the students keep the right eye open and cover the left eye (without compressing it) with paper or cardboard, because for evaluation purposes it is important to evaluate each eye separately and with the best correction4.
Then, the students were asked to read the optotypes of each row of the table, until he could no longer discriminate against them. It was expected to read at least two-thirds of the optotypes of each line24.
During the application of the Snellen Table, it was recommended that the nurse verifies the presence of signs or symptoms of visual difficulties such as tearing, head tilting, intermittent eye blinking, strabismus, discomfort or frowning1.
The Brazilian Council of Ophthalmology (CBO) advises that children who present reduced visual acuity after visual acuity evaluation should be reassessed before referral to specialized services to obtain greater reliability in the results found if false positives. Also, children who presented with a vision of less or equal to 0.7 in at least one eye, those presenting a difference of 0.2 or more between the eyes and those with signs and symptoms of visual changes should be re-evaluated25.
With the students who used glasses, visual acuity assessment was performed with and without corrective lenses. After the evaluation, the parents were informed by a document on the results of visual acuity. The parents of the students who presented bilateral or unilateral visual acuity were informed that the student would be referred to the ophthalmological service, and the teacher would contact, informing the day and time of the consultation. For the parents of students who did not have visual acuity, the need for periodic exams to prevent any change was reported.
RESULTS AND DISCUSSION
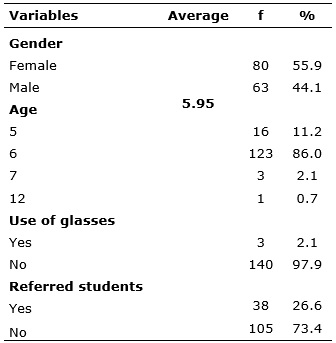
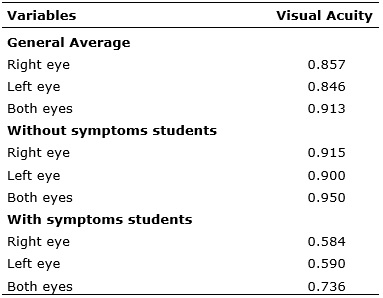
A total of 143 (100%) students were evaluated, most of them being female, with a mean age of 5.95 years old, with a minimum age of 5 years old and a maximum of 12 years old. See Table 1
TABLE 1:
Distribution of socio-demographic variables, use of corrective lenses and
referral to specialized service of subjects. Limeira-SP, 2011. (N=143)
Most of them are in the 6 years old age group, that is the recommended age at the beginning of the first grade of elementary school and the ideal age for the evaluation of visual acuity, because in this age group the discovery and treatment of some visual disturbances can avoid irreversible problems that affect the intellectual and social development of the child 5,18.
For the 118 (82.5%) students who did not show any symptom or signal indicative of visual impairment, the mean visual acuity was higher. However, 25 (17.5%) students presented some change with suspicion of the presence of visual impairment and, in these cases, the mean visual acuity was lower.
All students were questioned if they used glasses and it was found that only 3 (2.1%) students were already users of corrective lenses. However, only two had their glasses on the day of data collection. See Table 1.
Of the total number of students evaluated, it was necessary to send 38 (26.6%) students to the specialized ophthalmology department, according to the criteria that all the patients with visual acuity lower than 0.7 or difference of 0.2 between the eyes, should be attended by ophthalmologists. In some cases, visual acuity less than 0.7 and difference of 0.2 were observed. Such data corroborate another similar study25.
In this study, 10 (7.0%) students had a visual acuity difference between the eyes of 0.2 or more, and a total of 36 (25.2%) with a low visual acuity (less than 0.7).
All these students were retested by the nurses, before being referred to the ophthalmologist. The remaining students - 105 (73.4%) - did not need to be referred, as they did not meet the established criteria. See Table 1.
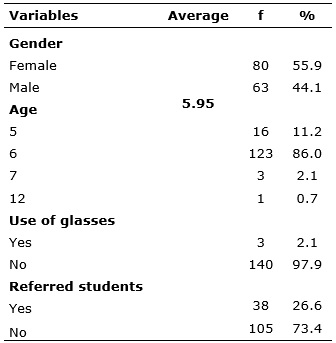
Among the most frequent symptoms revealed by the study subjects were the following: frowning (11.9%), restlessness (11.2%) and excessive blinking (9.1%). See Figure 1
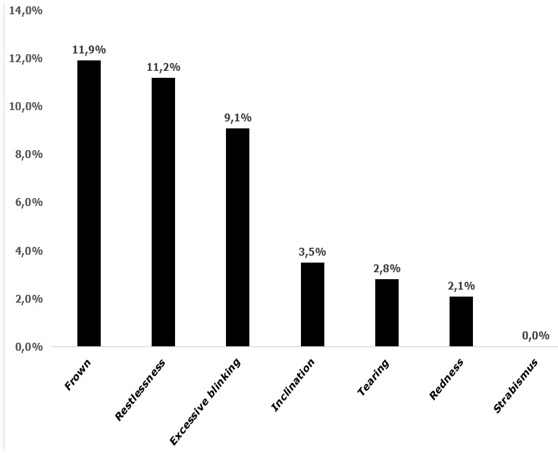
FIGURE 1:
Symptoms presented by the students during the visual acuity test.
Limeira-SP, 2011
The general results of the evaluation of the visual acuity of the subjects, using Snellen Test, are described in Table 2.
TABLE 2:
General results of visual acuity evaluation using the Snellen Test in
individuals. Limeira-SP, 2011. (N=143).
In the assessment of students´ visual acuity, it was found that symptomatic children tend to have the lowest visual acuity average, as shown in Table 2.
Correlating the visual acuity of the students (0.913) with all the symptoms presented, there was an association between visual acuity and tearing (p=0.001), visual acuity and redness (p=0.027), visual acuity and head inclination (p=0.005), visual acuity with excessive blinking of the eyes, and with forehead frown the significance was p <0.001.
Using the Mann-Whitney U Test, it was found that the association of visual acuity with tearing was significant with p=0.001. For the association of red eyes and Visual Acuity of the Right Eye (AVOD), the value of p=0.008 was found; for red eyes and Visual Acuity of the Left Eye (AVOE), p-value=0.017; and visual acuity of both eyes (AVAM) with values of 0.027.
In the association between head inclination and AVOE and AVAM, p=0.005 was significant and in AVOD, p=0.001. For the association, the excessive blinking of the eyes, frowning and in the restlessness, the significance was p <0.001.
These results showed that, after the training, the nurses were competent and could verify the visual acuity of the students, since they identified changes, contributing to the early detection of low visual acuity.
Ocular health care is often overlooked in ESFs and the role of nurses in the PSE. Therefore, researchers reinforce the need for nurses to perform prevention at the primary level as one of the ways to avoid or reduce the incidence of eye problems and blindness19.
It is necessary to mobilize health professionals to detect visual changes in time to avoid sequels, acting in partnerships with municipalities and with schools, creating bases for these professionals to have subsidies to develop actions that assess the visual problems perception in schoolchildren, providing better performance in school activities, aiming at the construction of new strategies for prevention and identification of visual changes in childhood25.
It was verified in this research that, in some ESF, trainees of the Undergraduate Nursing Course, who accompanied the evaluations, reported not being aware of this nurse´s performance, since they believed that only ophthalmologists could assess visual acuity. More information is suggested in the Nursing Undergraduate Courses regarding the participation of nurses in the ocular health area since it is essential to transform the model of academic training and work in service to qualify and commit professionals to face issues involving public health6.
CONCLUSION
The research trained and followed nurses of the ESFs in the evaluation of the visual acuity of schoolchildren, assisting them in the identification of changes and medical referral of those who presented visual changes.
It is evident that there is a need to offer theoretical subsidies for basic care professionals to carry out and effectively co-ordinate actions. The results showed that afte r training, ESF nurses acquired skills to perform the visual acuity test and to perform eye health programs.
It was verified that the nurse could contribute significantly to the early detection of visual problems, reducing repetition and school dropout.
The study highlights the need to strengthen the school health area with the integration of health and education sectors, seeking the provision of integral assistance to the student.
There was a limitation of the study in the great difficulty of parents or guardians in signing the TCLE. It is suggested to carry out orientations with an educational campaign to the parents, before beginning the data collection.
This research had a great social repercussion, considering that the Municipality of Limeira decided to include the project of the participation of the nurses of the ESF in the schools, identifying visual changes, for all the 10 ESFs of the city and not only the seven that participated in the study. Also, the nurses performed the visual screening for all elementary school students (first to fourth grade).
The research guided clinical decision-making through evidence-based practice, enabling solutions to the visual problems of schoolchildren and the implementation of interventions by nurses.
REFERENCES
1.Granzoto JA, Ostermann CSPE, Brum LF, Pereira PG, Granzoto T. Avaliação da acuidade visual em escolares da 1° série do ensino fundamental . Arq Bras Oftalmol. São Paulo. 2003; 66(2): 167-71.
2.Machado MFAS, Gubert FA, Meyer APGFV, Sampaio YPCC, Dias MSA, Almeida AMB, et al. Programa saúde na escola: estratégia promotora de saúde na atenção básica no Brasil. J Hum Growth Dev. 2015; 25(3): 307-12.
3.Laignier MR, Castro MA, Cabral de Sá PS. De olhos bem abertos: investigando acuidade visual em alunos de uma escola municipal de Vitória. Esc Anna Nery. 2010; 14(1): 113-9.
4.Moreira Neto CA, Moreira ATR, Moreira LB. Relação entre acuidade visual e condições de trabalho escolar em crianças de um colégio do ensino fundamental público de Curitiba. Rev bras oftalmol. 2014; 73(4): 216-19.
5.Fontenele RM, Sousa AI, Rasche AS. Saúde ocular em escolares e a prática dos enfermeiros da atenção básica. Cogitare Enferm. 2016; 21(1): 1-8.
6.Gomes NP, Bonfim ANA, Barros RD, Silva Filho CC, Diniz NMF. Addressing domestic violence through the family health strategy. Rev enferm UERJ.2014; 22(4): 477-81.
7.Coelho ACO, Marta DC, Dias IMAV, Salvador M, Reis VN, Pacheco ZML. Olho vivo: acuidade visual das crianças e emprego do lúdico no cuidado. Esc Anna Nery. 2010; 14 (2): 318-23.
8.Lopes GJA, Casella AMB, Chui CA. Prevalência de acuidade visual reduzida nos alunos da primeira série do ensino fundamental das redes pública estadual e privada de Londrina-PR, no ano de 2000. Arq Bras Oftalmol. 2002; 65(6): 659-64.
9. Ferriani MGC, Gomes R. Saúde escolar: contradições e desafios. Goiânia: AB editora; 1997.
10.Ministério da Educação (Br). Campanha nacional de reabilitação visual olho no olho: manual de orientação do professor.Brasilia(DF): Conselho Brasileiro de Oftalmologia; 2005.
11.Pires LM, Queirós OS, Munari DB, Melo CF, Souza MM. A Enfermagem no contexto da saúde do escolar: revisão integrativa da literatura. Rev enferm UERJ. 2012; 20 (1): 668-75.
12.Ministério da Saúde e da Educação (Br). Orientações sobre o programa saúde na escola para a elaboração dos projetos locais.Brasília (DF): Editora MS; 2008.
13.Alves MR, Temporini ER, Kara-José N. Atendimento oftalmológico de escolares do sistema público de ensino no município de São Paulo: aspectos médico-sociais. Arq Bras Oftalmol. 2000; 63(5): 359-63.
14.Ministério da Saúde e da Educação (Br). Projeto olhar Brasil. Triagem de acuidade visual: manual de orientação.Brasilía(DF): Editora MS; 2008.
15. Fialho FA, Dias IMAV, Salvador M, Pacheco ZML, Nascimento L. A enfermagem avaliando a acuidade visual de estudantes do ensino fundamental. Rev baiana enferm. 2011; 25(1): 33-40.
16.Moratelli M Jr, Gigante LP, Oliveira PRP, Nutels M, Valle R, Amaro M, et al. Acuidade visual de escolares em uma cidade do interior de Santa Catarina, 2003. Revista da AMRIGS. 2007; 51 (4): 285-90.
17.Gasparetto MERF, Temporini ER, Carvalho KMM, Kara-José N. Dificuldade visual em escolares: conhecimentos e ações de professores do ensino fundamental que atuam com alunos que apresentam visão subnormal. Arq Bras Oftalmol. 2004; 67(1): 65-71.
18.Kara-José N, Temporini ER. Avaliação dos critérios de triagem visual de escolares de primeira série do primeiro grau. Rev saúde pública. 1980; 14 (2): 205-14.
19.Prado TCM, Lima AP. Eye health: the preventive job of nurses in a School Health Program. Unopar Cient Ciênc Biol Saúde. 2013; 15 (4): 327-30.
20.Jeveaux GC, Portes AJF, Couto Júnior AS, Shinzato Fl. Prevenção à cegueira em crianças de 3 a 6 anos assistidas pelo programa de saúde da família (PSF) do Morro do Alemão – Rio de Janeiro. Rev Bras Oftalmol. 2008; 67 (5): 226-30.
21.Moura MAV, Souza IEO, Lins S, Bastos VD. Qualidade de vida e condições de saúde do escolar: uma investigação de aluno da Escola de Enfermagem Anna Nery. Rev Soc Bras Enferm Ped. 2005; 5(1): 31-8.
22.Dantas AR, Pagliuca LMF, Almeida PC. Validação da escala optométrica: regionalizada para pré-escolares: contribuição da enfermagem. Rev esc enferm USP. 2009; 11(5): 4-7.
23.Gil AC. Como elaborar projetos de pesquisa. 5 ed. São Paulo: Atlas; 2010.
24.Lopes CL, Barbosa MA, Marques ES, Lino AIA, Morais NHF. O trabalho da enfermagem na detecção de problemas visuais em crianças/adolescentes. Rev eletrônica enferm. 2003; 5 (2): 55-9.
25.Laignier MR, Castro MA, Cabral de Sá PS. De olhos bem abertos: investigando acuidade visual em alunos de uma escola municipal de Vitória. Esc Anna Nery. 2010; 14(1): 113-9.