 p ≤ 0.05 statistically significant calculated by the Fisher test
p ≤ 0.05 statistically significant calculated by the Fisher test
BMI = body mass index GO = kidney failure
RESEARCH ARTICLES
Characteristics of critical patients with hypoglycemia: safe use of continuous infusion of insulin
Raquel de Mendonça NepomucenoI; Lolita Dopico da SilvaII; Sandra Regina Maciqueira PereiraIII
I
PhD student of the Post-Graduate Program in Nursing at the Rio de Janeiro State University. Visiting Professor of the Postgraduate course in Intensive
Nursing at UERJ. Routine Nurse of the ICU Hospital Américas Medical City and the National Institute of Cardiology. Rio de Janeiro, Brazil. Email: raquel.nepomuceno@gmail.com
IIPermanent Professor of the graduate program in nursing, Faculty of nursing Rio de Janeiro State University, Department of medical-surgical Nursing.
Coordinator of the Intensive Nursing Course Email: lolita.dopico@gmail.com
III
Associate Professor, Department of Nursing Medical-Surgical Nursing Faculty of the State University of Rio de Janeiro - Nurse Pro-Cardiac Hospital. Email: sandregina@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.14505
ABSTRACT
This cross-sectional, prospective study to describe the characteristics of critically ill patients with severe hypoglycemia was conducted in 2014 at a federal public hospital, with 42 post-operative cardiac surgery patients receiving intravenous insulin, 15 of whom presented hypoglycemia. Characteristics with positive associations and statistical significance for occurrence of hypoglycemia were low hematocrit (p=0.03852) and emergency surgery (p=0.02884). Other features showing positive associations only included kidney failure treated with dialysis, PaO2≥90mmHg, and use of vasoactive amine (OR>2). It was concluded that nurses must take account of characteristics that influence glycemia so as to avoid errors in titration of insulin doses for administration.
Keywords: Insulin; glycemia; nursing; intensive care.
INTRODUCTION
Critical patients are under a state of physiological stress due to the severity of their clinical condition, predisposing them to various endocrine disorders such as hyperglycemia1. Hyperglycemia causes deleterious effects micro and macro-vascular, as kidney, immune system disorders, neuropathies, hydroelectrolytic disorders and endothelial dysfunction that predisposes them to thrombogenesis.1
For the control of hyperglycemia, insulin is the only hormone that makes the transport to cells so that they don't become deprived of energy. In Brazil, it is nurse's responsibility for preparation and administration of continuous insulin infusion (CII) in most hospitals. With this, the nurse should be aware of the aspects that involve these steps including the monitoring of the effects of insulin in the control of hyperglycemia, as well as to prevent the onset of severe hypoglycemia. This care is centered mainly in the setting of infusion from the blood glucose measurement performed by nurses using portable glucose meters.
In the intensive care units (ICU), CII protocols recommend the use the glucometer for practicality of use and low cost of the method, which presents good correlation of accuracy, when compared with the laboratory testing.2
However, various aspects can influence the accuracy of the results obtained, such as those related to the procedure, such as the volume and origin of blood sample, the incubation time of the sample, the calibration of the device, the moisture and temperature on storage of test strips. However, there are other features related to the patient as the presence of peripheral edema, the hypo-perfusion, the hematocrit and the use of vasoactive medications, which for different reasons may interfere with the blood-glucose measurement, resulting in the inadequate adjustment of insulin.3,4
Rarely, there is the nurse to consider these factors in critically ill patients as a source of erroneous blood glucose results. The most common is to observe the nurse concerned with technical issues involving the blood-glucose procedure.
This study is justified by data found in the literature indicate that among the critical patients who receive CII, there is an incidence between 4% and 16% of severe hypoglycemia, without pointing however, if the characteristics of the patients could influence the onset of hypoglycemia. They are expected to contribute information for ensuring the adequacy and the strict control of the administered insulin, because in Brazil, is the responsibility of nursing for the preparation and administration of CII, leaving the monitoring of insulin action under supervision of nurses in order to avoid severe hypoglycemia. 5
This monitoring is focused on the measurement of blood glucose by nurses, so that the control of the insulin infusion flow occurs from blood glucose values found and the adjustment guided by protocols to keep blood glucose levels within the established target range, minimizing the risk of hypoglycemia.
The nursing staff in their practice in the care of these patients in the ICU, does not usually consider aspects of the patient, as the use of vasoactive amine, presence of edema and peripheral hypo-perfusion, hematocrit and the history of diseases (diabetes, hypertension and renal failure, for example).
From the concern with the issues surrounding the blood-glucose measurement of critical patients receiving CII, this research was conducted in order to identify critical features in patients with hypoglycemia during intravenous insulin infusion.
LITERATURE REVIEW
In recent years, the intensive glucose control achieved by continuous infusion of insulin (CII) began to occupy a prominent position in the management of critical patients. The premise is that the maintenance of normoglycemia is associated with lower rates of infections and organic failure. Insulin is the only hormone that makes this transport and without it, the cells are deprived of energy2.
The safety of insulin therapy can be expressed by the absence of hypoglycemia that, in patients with continuous intravenous insulin (CII), can be avoided, especially by the proper adjustment of the infused insulin dose. In addition, this adjustment depends directly on the blood glucose levels being measured regularly. It is then necessary to ensure that this measure is the most accurate possible.
In the treatment of critical patients, studies were motivated by the need to think about how insulin was administered with respect to concentration, the dosage, the indications, routes of administration, the therapeutic objectives and the risks associated with therapy. The study, considered a pioneer, tested the hypothesis that the normalization of blood glucose with insulin intravenous therapy or intensive glucose control would reduce the morbidity and mortality in critical patients. It is noted that insulin therapy decreased the mortality rate from 8% to 4.6%.3
Despite the reduction in mortality, there was an increase in six times the incidence of hypoglycemia in patients with intensive blood-glucose control, receiving CII, so that many authors consider hypoglycemia and only adverse event related to intravenous insulin therapy.1,3
Thus, the implementation of protocols to steer intravenous therapy with insulin and monitoring of their effects have been created. They indicate the concentration of infusion solution, the initial dose, therapeutic effect and monitoring as the subsequent doses. They seek to correct hyperglycemia, avoiding hypoglycemia. In general, they have been seen that the protocols have the nurses as principal executor agent. 1.4
METHOD
An epidemiological study with cross-sectional design developed an intensive care of a large public hospital in the city of Rio de Janeiro. The data collection took place from May to October 2014. The population was composed of patients receiving an intravenous insulin at 100U/ml concentration for at least 12:0, over 18 years, with record of glucose measurements performed with arterial samples and consent of patients or their relatives by an informed consent. The following patients were excluded: brain dead, those that showed Diabetic Ketoacidosis or hyperosmolar coma and undergoing re-surgical exploration. Have been assessed, age, gender, body mass index (BMI), type of surgery, elective or emergency, arterial hypertension (AHT), diabetes mellitus (DM), sepsis, renal failure (KF) and dialysis treatment, cerebral vascular accident (CVA); triglycerides > 1000 mg/dl uric acid > 7mg/dl, hematocrit≤ 35%, and arterial oxygen pressure PaO2 ≥ 90 mmHg; vasoactive amine OS, mean arterial pressure (map) < 65mmhg and measured blood glucose.
Mean arterial pressure was collected at the time of glucose measurement for further evaluation of circulatory status. The unit brand was the glucometer Accu-Check Active/Roche ® used with its respective reagent strips, being all the blood-glucose checks were made with a single piece of equipment.
BMI were considered the possibilities of eutrophic (18.5-24.9) and overweight (25-29.9).
We calculated the Odds Ratio OR value was calculated by Fisher's exact test, and adopted significance level of 5% (p <0.05). All calculations were made through the program available free via the website www.openepi.com. This research was approved under paragraph 3083/2012.
RESULTS
In the research unit, 42 patients used insulin infusion, of which 15 had at least two episodes of hypoglycemia. The population was divided into two groups, the first (G1) of patients who have hypoglycemia ≤60mg/dl (n=15), and the second (G2), of patients who showed no hypoglycemia (n= 27). In table 1 are the main features of the patients according to these groups.
TABLE 1:
Clinical characteristics of patients with ICI. RJ, 2014. (F=42)
 p ≤ 0.05 statistically significant calculated by the Fisher test
p ≤ 0.05 statistically significant calculated by the Fisher test
BMI = body mass index GO = kidney failure
As the institutional protocol, all patients using CII received caloric support with intravenous infusion of dextrose at 10%. There was no occurrence of stroke and sepsis, as well as the data on the levels of uric acid and triglycerides were measured in patients during the collection.
In both groups, there was the same trend in relation to most of the characteristics. We found 24 patients with female predominance (57.14%), 24 overweight (57.14%), 33 without diabetes (78.57%), 38 without renal failure without dialysis treatment (90.48%), 32 undergoing elective surgery (76.19%). In relation to age, showed an average age of 48 (±15.85) years and median of 62 years and 61 years, respectively, in patients from G1 and G2.
MAP was observed with an average of 77 (±10.29) mmHg and by using vasoactive amine (80.95%) In 85.71% of cases met arterial oxygen partial pressure≥ 90 mmHg and hematocrit <35% in 71.42%.
The variables with difference significantly between groups statistics for the occurrence of hypoglycemia were emergency surgery (p=0.02884) and hematocrit (p=0.03852). The other characteristics, although not present statistical significance showed positive association with the occurrence of hypoglycemia.
For verification of this Association has calculated the Odds Ratio (OR). Specifically, in the 15 patients with hypoglycemia (G1), the characteristics of patients who had higher association (OR> 2) with the occurrence of hypoglycemia were hematocrit <35%, emergency surgery, renal failure with dialysis treatment, and use of vasoactive amine PaO2 ≥90mmHg.according to table 2.
TABLE 2
: Association between the occurrence of hypoglycemia and clinical characteristics of patients with ICI. RJ, 2014. (F=42)
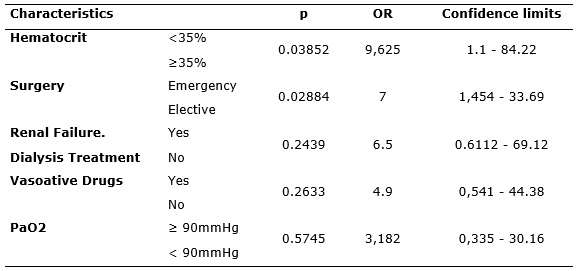
In this study, low hematocrit was the clinical trait with greatest association with hypoglycemia. Patients with this condition have a chance 9,625 times greater to compromise the accuracy of the glycemic outcome than those with normal hematocrit. Then it was observed in patients undergoing emergency surgery at a 7, OR what can raise in 7 times the chance of compromising the accuracy of the blood-glucose measurement. It should be noted that, in both, the minimum value of the confidence interval was > 1 representing statistical significance equivalent to the p value.
The presence of renal failure with dialysis treatment, the use of vasoactive amine and the elevation of PaO2above 90 mmHg, presented positive association with hypoglycemia, but there were no statistically significant differences.
DISCUSSION
We found an incidence of hypoglycemia 35.7% (n = 15), which is well above that recorded in the literature which is around 4% to 16%.6
Traits with positive association and statistical significance for the onset of hypoglycemia were low hematocrit (p=0.03852) and emergency surgery (p=0.02884). Other features only showed positive Association, like renal failure with dialysis treatment, the PaO2 ≥ 90mmHg and the use of vasoactive amine(OR > 2).
Low hematocrit
Several studies agree that low hematocrit interferes with blood glucose measurement overestimate blood glucose, i.e., the results are falsely elevated. There is time, if you know its effects in the precision of the analysis of the portable glucometer. Instructions for operation of these devices suggest that hematocrit levels must be between 25 to 55% to provide trusted values of capillary glycemia.6,7
The study8 pointed out that the smaller the hematocrit value, the greater the effect on accuracy of glucometers, reaching up to 30% of inaccuracy with falsely elevated blood glucose results. A mathematical correction of hematocrit values was proposed, as glucose meters to analyze the sample require a hematocrit value of 40%.
Currently, various glucometers outweigh the hematocrit values, reducing these errors. Still, it is not recommended the use of glucometers in individuals with very low hematocrit, because authors have observed occurrence of more than 5% of errors in patients with hematocrit below 34%, resulting in a falsely increased blood-glucose.8,9
With this, it can be affirmed that the smaller the hematocrit greater the chance of error in measurement. It is known that a blood-glucose measurement, falsely elevated indicates for the nurse, to maintain or increase the dose of insulin, which can later generate the hypoglycemic event.
This effect occurs by mechanical impedance of diffusion of plasma in the reagent layer test strip, so the sample more diluted, less hemo-concentrated, results in a faster diffusion of glucose which can mask hypoglycemia in anemic patients.9
In addition, studies point out that surgical patients have higher risk of mistakes in glucose measurements due to the fluctuating hematocrit arising from the surgery, which may justify the occurrence of hypoglycemia found in this study (35.7%).9
However, in daily practice, is not observed patient care hematocrit by the nursing as a recommendation that can make a difference in insulin adjustments.
Emergency surgery
The population in question, the elective surgeries represented 76.19% with predominance of valve replacement surgery aortic and mitral (n=22), followed by myocardial revascularization (n=10).
Myocardial revascularization surgery is still the most cardiovascular operation performed in Brazil, but when compared with the heart valve operations, presents a lower growth in recent years. Therefore, the profile of the procedures has been changing with increased growth of the approach on the heart valve, correction of congenital anomalies and arrhythmia. 10.11
Regarding the emergency surgery, most happened in patients who have hypoglycemia (G1). They underwent exploratory Thoracotomy (n = 8) and the system of implant circulatory assistance with extracorporeal membrane oxygenation (ECMO) (n = 2). The explorative Thoracotomy occurred in patients with pericardial effusion by coronary artery disease, studying with cardiac tamponade. And the ECMO system, in this study, it was indicated for patients in cardiogenic shock after acute myocardial infarction, for maintaining tissue perfusion with oxygenated blood pending the recovery of the organ primarily affected, heart, lungs or both. Both situations indicate patients with high levels of mortality.12
As it is known, acute hyperglycemia is the manifestation of metabolic and hormonal changes associated with responses to stress and injury, including surgical trauma. It should be noted that heart surgery is a complex procedure, which influences several physiological mechanisms; uses medicines and equipment, which may cause harm to the patient, imposing a great organic stress. Studies have shown that neuroendocrine and metabolic response to surgical stress starts in pre-op, because anxiety and fear related to anesthesia and surgery generate elevation of plasma catecholamines. 13.14
Patients undergoing cardiac surgery may present on "insulin resistance", due to various factors such as the adsorption of insulin on the surface of the reservatory circuits and system components of cardiopulmonary bypass (CPB); the endocrine-metabolic response to surgery; CPB and the cardiac reperfusion itself. The magnitude of these responses is strongly associated with surgical size, so that minor surgery induce fewer answers than medium and large, as in cardiovascular surgery with cardiopulmonary bypass (CPB).14
It reflects in the case of patients hypoglycemic observed in this study, the most complex and undergoing emergency surgery impose higher organic stress and hence greater chance of postoperative hyperglycemia and insulin use, increasing the risk of hypoglycemia.
It should be noted that in this study, this type of surgery presented positive association with hypoglycemia, representing a 70% risk for patients undergoing the emergency surgery expressing statistical significance (p= 0.02884). Therefore, patients who had emergency surgery with signs and symptoms of ventricular failure had a 2.8 times greater risk than those who do elective surgeries, and greater chance of hypoglycemia (OR=7).
Renal failure with dialysis treatment
Acute renal failure (RF) is commonly associated with hyperglycemia, either by acidosis or by the catabolic state, or due to a resistance to insulin action. However, in this study, patients with this condition were submitted to dialysis therapies, which may justify the association with hypoglycemia.
In the ICU, the incidence of RF ranges from 17% to 35%, of which 49% to 70% of patients require dialysis treatment. At the beginning of this treatment is necessary a vascular access, which involves the percutaneous puncture of a large blood vessel (internal jugular, Subclavian or femoral vein) and the diversion of blood through equipment to a blood filtering system. 15
Studies suggest that metabolic complications were statistically more frequent dialysis group when compared with patients with RF without dialysis, however does not indicate the nature of these complications.14
It is believed that the hypoglycemia in patients with dialysis therapy is related to the method and materials used in its execution, which have not been fleshed out in this study, as the concentration of glucose in dialytic solution and the occurrence of the phenomenon of adsorption (adhesion) of insulin in equipment and filters used.16
Effect of vasoactive amine
The infusion of vasoactive amine, being norepinephrine the first choice as seen in this research, is indicated in the immediate postoperative period of cardiac surgeries in order to maintain blood pressure levels above 65 mmHg to ensure cell perfusion.
Studies point the use of vasoactive amine ranging from 35.2 to 62% in patients of mixed population, clinical and surgical during the use of the CII. 17-18
In this study, the vasoactive amine were administered in 80.95% of patients during intravenous insulin infusion, which is expected due to the nature of the surgeries performed. Among patients who used vasoactive amine, 33.33% presented hypoglycemia.
It is known that the vasoactive medications have action in alpha and beta-adrenergic receptors producing the effects of vasoconstriction, relaxing smooth muscles in the gastrointestinal tract and metabolic changes.19
Among the metabolic changes in the blood have been reported the activation of beta-adrenergic receptors in fat cells that results in increased lipolysis, with increased release of free fatty acids and glycerol. On the other hand, the activation of alpha-2 receptors of the lipocytes inhibits lipolysis. Yet, the alpha and beta-adrenergic receptors in pancreatic islets tend to increase and to decrease the secretion of insulin, respectively.19
Reflecting on these changes, dares to infer the presence of glycerol, as a precursor of glucose in the bloodstream, could contribute to the occurrence of false results, the possibility of reaction with the enzyme glucose oxidase method, which would explain the possible overestimation of glucose measures; however, this reasoning did not find support in the literature consulted.
Studies to compare the accuracy of glucose measurements performed with glucometers to the bedside, in two groups of patients, one using vasoactive amine and one without vasoactive amine , found 18% of inaccurate values in the first group and only 3% in the second and overestimation in values 40% blood glucose in capillary measurements in patients with vasoactive amine. It can be affirmed that the hair sample is not need in critically ill patients with intravenous vasoactive amine using the glucometer at the bedside.19
It is believed that the nature of the influence of vasoactive medications on blood glucose and on accuracy of measurement-Glycemic is complex and still obscure, perhaps, by the fact that its effects in different adrenergic receptor are dose dependent. That is, depending on the dose administered, there is a certain stimulus, adrenergic receptor generating various metabolic changes. This can make it difficult to predict which drug dose causes greater or lesser risk for hypoglycemia.
Effect of PaO2
Surgical patients tend to have hyperoxia, especially when performing cardiopulmonary bypass. The literature points out that the high pressure of oxygen reduces falsely glucose readings, featuring low pressures and hypoglycemia (hypoxia) overestimate blood glucose in 15% when glucometers with glucose oxidase method are used. 19
In this study, the glucometer glucose oxidase was used as analysis method. So it was not expected that patients with hyperoxia showed a positive association with hypoglycemia (OR=3.182). One might think that the Glycemic values found could portray a false or hypoglycemia, patients also showed low levels of hematocrit. What seems more likely is that the hematocrit has a stronger association (OR = 9.625) than hyperoxia as a determinant in the occurrence of hypoglycemic measures that could be misleading.
Thus, in the context of intensive care nurses must contribute to the reduction of severe hypoglycemia episodes, benefiting patients and hospital institutions on issues of patient safety that receives intravenous insulin and involving nursing. 20
CONCLUSION
In this population group, characteristics with statistical significance for hypoglycemia were emergency surgeries and low hematocrit. It was evidenced that factors such as the low hematocrit, the use of vasoactive amine and PaO2 high are directly related to the accuracy and the precision of measuring Glycemic held with glucometers, generating false results that compromise security in the administration of intravenous insulin, increasing the risk of hypoglycemic events.
Therefore, to ensure safe use on intravenous insulin infusion, it is recommended that nursing actions incorporate the identification of predisposing factors of each patient. The nurse should plan the procedures to avoid the delay or delay in performing tests that require fasting, performing dietary supply and the measurement of capillary blood glucose at certain times.
In this sense, it is understood that the nurse when caring for a patient receiving continuous infusion of insulin must meet these key traits for the onset of hypoglycemia. Due to the multifactorial nature of the onset of hypoglycemia, the knowledge of the predisposing factors is critical to the adoption of preventive and therapeutic measures.
The limitations of the study refers mainly to the loss of data due to the impossibility of having a team for data collection at all times.
It is recommended to carry out further studies to test which nursing care would be effective as a barrier to episodes of hypoglycemia; which factors signal the risk of the blood-glucose measurement to detect hypoglycemia and what are the predisposing factors that indicate the patient when combined with varying susceptibility to the occurrence of adverse events during the CII.
REFERENCES
1.Magalhães FGC. A insulinoterapia intensiva nos diferentes contextos de hiperglicemia em âmbito hospitalar [dissertação]. Portugal: Universidade do Porto, Instituto de Ciências Biomédicas Abel Salazar; 2010.
2.Goodman & Gilman. Manual de farmacologia e terapêutica. 20ª ed. Porto Alegre: AMGH; 2010.
3.Intitute for Safe Medication Pratices. ISMP's listo f high-alert medications. [Internet]. ISMP, 2012. [citado em 20 mar de 2014] Disponível em: http://www.ismp.org/tools/highalertmedications.pdf
4.Stamou SC, et al . Hypoglycemia with intensive insulin therapy after cardiac surgery: predisposing factors and association with mortality. Thorac Cardiovasc Surg [periódico na internet]. 2012 [citado em 20 mar de 2014] ; 32:82-97 . Disponível em: http://www.ncbi.nlm.nih.gov/pubmed/?term=Stamou%2C+Sotiris+C.%3B+Nussbaum%2C+Macy%3BCarew%2C+John+D.%3B+Dunn%2C+Kelli%3BSkipper%2C+Eric%3B+Robicsek%2C+Francis%3B+Lobdell%2C+Kevin+W
5.Guyton AC, Hall JE. Tratado de Fisiologia Médica. 10ª ed. Rio de Janeiro: Guanabara Koogan; 2009.
6.Sociedade Brasileira de Diabetes. Controle da hiperglicemia intra-hospitalar em pacientes críticos e não críticos. Posicionamento Oficial SBD Nº 02 /2011. Disponível em: http://www.nutritotal.com.br/diretrizes/files/228posicionamento_sbd_hiperglicemia.pdf.
7.Diretrizes da SBC sobre angina instável e infarto agudo do miocárdio sem supra desnivelamento do segmento ST (II Edição, 2007) – Atualização 2013. Arq Bras Cardiol. 2014; 102(3Supl.1).
8.Via MA, Scurlock C, Adams DH, Weiss AJ, Mechanick JI. Impaired postoperative hyperglycemic stress response associated with increased mortality in patients in the cardiothoracic surgery intensive care unit. Endocr Pract [periódico na internet]. 2010 [citado em 05 fev 2014]; 16:798-804. Disponível em: http://www.ncbi.nlm.nih.gov/pubmed/20350912
9.Wiener RS, Wiener DC, Larson RJ. Benefits and Risks of Tight Glucose Control in Critically Ill Adults : A Meta-analysis Author Affiliations: VA Outcomes Group, Department of Veterans Affairs Medical Center, White River Junction, Vermont, and Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth Medical School, Hanover, New Hampshire (Drs Soylemez Wiener and Larson); and Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire (Dr Wiener). JAMA [periódico na internet]. 2008 [citado em 05 fev 2014]; 300: 933-44. Disponível em: http://www.ncbi.nlm.nih.gov/pubmed/18728267
10.Egi M, Bellomo R, Stachowski E, French CJ, Hart GK, Taori G, et al. The interaction of chronic and acute glycemia with mortality in critically ill patients with diabetes. [periódico na internet]. 2007 [citado em 05 fev 2014]; 35: 503-7. Disponível em: http://www.ncbi.nlm.nih.gov/pubmed/17713400
11.Carvalho D, Esteves C, Neves C. A Hipoglicemia no Diabético: controvérsia na avaliação, à procura das suas implicações. Acta Médica Portuguesa. 2012; 25: 454-60.
12.Morais GFC et al. O diabético diante do tratamento, fatores de risco e complicações crônicas. Rev enferm UERJ. 2009; 17: 240-45.
13.Silva WO. Controle Glicêmico em Pacientes Críticos em UTI. Revista HUPE. 2013; 12: 47-56.
14.Soares GMT, Ferreira DCS, Gonçalves MPC, Alves TGS, David FL. Prevalência das Principais Complicações Pós-Operatórias em Cirurgias Cardíacas. Rev Bras Cardiol. 2011; 24: 139-146.
15.Bastos MG, Bregman R, Kirsztajn GM. Doença renal crônica: frequente e grave, mas também
prevenível e tratável. Rev Assoc Med Bras. 2010; 56: 248-53.
16.Burmeister JE, Campos JF, Miltersteiner DR. Efeito de diferentes níveis de glicose no dialisato sobre o risco de hipoglicemia durante hemodiálise em pacientes diabéticos. J. Bras. Nefrol [periódico na internet]. 2012 [citado em 05 fev 2014]; 34: 323-27. Disponível em: http://www.scielo.br/pdf/jbn/v34n4/v34n4a03.pdf
17.Preiser JC, Devos P. Clinical experience with tight glucose control by intensive insulin therapy. Crit Care Med [periódico na internet]. 2007 [citado em 05 fev 2014]; 35: 503-7. Disponível em: http://www.ncbi.nlm.nih.gov/pubmed/17713400
18.Ellahham S. Insulin therapy in critically ill patients. Vasc Health Risk Manag [periódico na internet]. 2010 [citado em 05 fev 2014]; 6: 1089-1091. Disponível em: http://www.ncbi.nlm.nih.gov/pubmed/21191429
19.Pitrowsky M, Shinotsuka CR, Soares M, Salluh JIF. Glucose control in critically ill patients in 2009: no alarms and no surprises. Rev Bras Ter Intensiva [periódico na internet]. 2009 [citado em 05 fev 2014]; 21: 310-4. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-507X2009000300012&lng=en&nrm=iso&tlng=en
20.Silva LD. Segurança e qualidade nos hospitais brasileiros. Rev enferm UERJ. 2013; 21: 425-6.