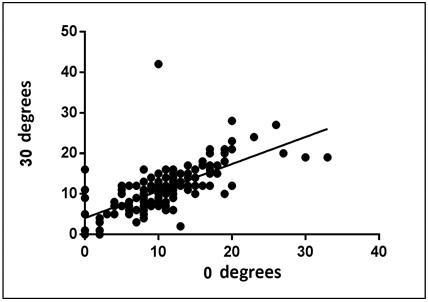
FIGURE 1: Correlation between PVCs at 0o and 30o (bed head). São José do Rio Preto, 2013
ORIGINAL RESEARCH
Central venous pressure measurement with patient at different angles
Lidia Maria Beloni SilvaI; Daniele Cristiny SilvaII; Lucia Marinilza BeccariaIII
I
Mestre pelo Programa de Enfermagem da Faculdade de Medicina de São José do
Rio Preto. São Paulo, Brasil. E-mail: lidiabelonisilva@gmail.com
II
Mestranda pelo Programa de Enfermagem da Faculdade de Medicina de São José
do Rio Preto. São Paulo, Brasil. E-mail: dani_cristiny@hotmail.com
III
Doutora, Docente do Departamento de Enfermagem Especializada da Faculdade
de Medicina de São José do Rio Preto. São Paulo, Brasil. E-mail: lucia@famerp.br
DOI: http://dx.doi.org/10.12957/reuerj.2016.14502
ABSTRACT
Objective: to investigate whether central venous pressure values differ with patient bed inclination. Method: this quantitative, analytical, longitudinal study was conducted from November to August 2013 at four intensive care units at a large hospital in northwest São Paulo. Central venous pressure was measured in 156 patients at four different bed inclinations each, totaling 624 measurements. The data are expressed in absolute and percentage values, variables were analyzed using the Mann-Whitney and Wilcoxon tests, and associations between measurements were tested by Pearson's correlation coefficient (r).Conclusion: measurements were found to be accurate at 0 o and 30o (a positive correlation between measurements), but a weak correlation at 0o and 45o (revealing little association between the variables).
Keywords: Central venous pressure; nursing care; intensive care; blood volume.
INTRODUCTION
According to the Collegiate Board Resolution (RDC) Nº 307 of 14 November 2002 by the National Health Surveillance Agency (ANVISA), monitoring in the intensive care unit (ICU) is mandatory and essential in patient care. Therefore, team of critical care professionals should have specific knowledge to use the technology necessary1.The methods used for basic hemodynamic monitoring are: heart rate (HR), electrocardiogram (ECG), oxygen saturation (SaO2), Mean blood pressure non-invasively (PAMNI), invasive mean arterial pressure (PAMI), respiratory rate (RR), temperature (Tº), urine output and central venous pressure (CVP)2.3.
PVC is the term used to describe the pressure in the superior and inferior vein caves during the venous return in the systemic circulation and must be measured when there is doubt about the volume status such that the correction might interfere with the patient's therapy. The main indications are shock of any etiology, severe respiratory distress, acute renal failure, severe sepsis, cardiac surgery, thoracic surgery, cardiac, liver and kidney transplants and other major surgeries, nephritic syndrome, severe dehydration, liver failure and large burnt4.
Despite the limitations as a method for assessment of blood volume, it is the most simple, minimally invasive, quickly available practice at the bedside and indicated as a monitoring method2.
The techniques described in the literature for assembly and measurement of PVC contain no information about the elevation of the head of the bed may significantly alter the pressure values. So this study aimed to identify whether there are differences in the values of central venous pressure with the head of the patient's bed lifted.
LITERATURE REVIEW
The invasive procedures for hemodynamic monitoring as central venous catheter insertion and the first steps of intravascular pressure became reality after the discovery of anticoagulants in 1917 (heparin), and the electronic revolution in the 60s and the use of pressure transducers 19745. Noteworthy are the studies by Swan and Ganz that enabled the monitoring of physiological parameters important in the care of critically ill patients6. In 1959 Hughes and Magovern described a right atrial monitoring technique as a guide for replacement of blood volume in patients undergoing thoracotomy. These authors reported a drop in PVC blood loss and a relationship between this pressure and blood transfusion. Wilson and Grow improved the technique and soon it became routine with patients undergoing thoracic surgery7. The measure was introduced only as intravascular blood volume parameter in 19628.
The assessment of blood volume and pressure indicator must be performed by the response to infusion of liquids in series mode. The absence of increases in PVC up to 3 millimeters of mercury (mm Hg) after standardized volume of evidence and analysis of the clinical presentation is heart good performance guarantee and space for volume replacement2.
Some authors claim that PVC should not be routinely checked for not being a good intravascular volume predictor. Nevertheless, they should be used in selected circumstances, such as patients who have undergone heart transplantation, suffered a heart attack of the right ventricle, or the embolism frames as a marker of acute lung right ventricular function, rather than the blood volume status indicator7.9. Thus, the analysis of PVC results is subject to other monitoring parameters, the patient's condition, and heart function10.
Determining the access road is the starting point for measurement of PVC. The catheter can be installed via the internal jugular, sub-clavian, femoral, central catheters peripherally inserting the Peripherally Inserted Central Catheter (PICC) by either puncturing or dissection2, 9-12. The choice of the insertion site should consider the risks and benefits of each site. Imaging tests must confirm the catheter tip position, mainly to access the superior vein where the appropriate point is the middle third of the vein. The position of the femoral access is not routinely checked, as catheters are shorter with less risk of becoming intracardiac4.
The risks for the patient, as the verification of PVC, are related to the catheter used. Possible complications can be infectious or noninfectious and can occur during insertion or maintenance of the device used. In this process, the assistance and care provided can reduce the risk of complications13.
For multi-way catheters there is no way considered suitable for measurement, there are statistical differences between the tracks, but they are not clinically significant. Ideally, the measures are always taken in the same way that the pressure trend curve has no bias12.
Four points should be considered in the pressure monitoring process: System assembly, leveling, zeroing and dynamic response4. Check parameter is complex and linked to detailed realization of assembly technique, because if the steps are not followed correctly, errors may occur when reading results8.
The assembly is done by means of two systems: water column or electronic pressure transducers. As in water column is simple and low cost, but makes it impossible to view the pressure curve and the values obtained are in centimeters of water (cm H2O). The use of pressure transducer allows visualization of the continuous curve, but the cost is higher and it is necessary specific monitoring equipment. The results are in mm Hg2.4.
As the PVC through the water column is less accurate than continuous with the use of electronic pressure transducers. When continuous digital monitoring is not possible, then it should be used on internal jugular veins or left sub-clavian because the measurements are more accurate2.4.
For best uniformity of communication and information, the results may be converted mm Hg to cm H2O or other, since it should be known that 1 mm Hg = 1.36 cm H2O. The conversion from cmH2O to mm Hg is performed by dividing the value obtained in cm H2O 1.36 and a conversion into cm H2O is done by multiplying the value obtained in mm Hg por 1,364.10.
Leveling is accomplished by identifying the phlebostatic axis or physiological zero reference point for the average arterial14. The localization can be performed by drawing a vertical line drawn down from the fourth intercostal space and an imaginary horizontal line drawn midway between the anterior and posterior surfaces of the thorax. Where the lines intersect is the approximate height of the right atrium, this point is between the axillary line and anterior axillary4. Another point described for the axis is in the mid-axillary line in the fourth or fifth intercostal space, however, important to remember that the use of this point may overstate the actual PVC up to five mm Hg2,9,15.
Zeroing and dynamic response test should be performed only when in use of pressure transducers. Zeroing is the transducer calibration at bedside and the dynamic response is made pressing the flush for two seconds at the moment the PVC wave appears square on the monitor and so interrupted flush occurs one or two oscillations before returning normal wave4,11.
There is no consensus on the range considered normal parameters of PVC. The proximity of the position of the catheter to the right atrium, the right arterial pressure values (PAD) can be considered. The normal DBP is from 1 to 10 mm Hg to 5 mm Hg average. These values are appropriate for leveling obtained between the previous average axillary and axillary line4.10. Leveling the axillary line has as parameter 2 to 6 mm Hg11. With children, the values considered normal are 0-6 mm Hg with an average of 3 mm Hg16.
The Surviving Sepsis Campaign provides a target for the care of septic patients CVP between 8 to 12 mm Hg for patients breathing spontaneously and between 12 and 15 mm Hg for patients on mechanical ventilation17. For patients in neohepática phase and on the first day post liver transplant, to maintain PVC 8 mm Hg proved beneficial for decreased flow rate in the portal vein preventing portal hyperperfusion18.
The technique of measurement of pressure described in the literature, it is recommended that the patient should be kept in a horizontal position, and if not possible the PVC can be seen in the semi-recumbent position and the system must be reset every time you change the head bed4.19.
In ICU high head of maintenance at 30 ° or 45 ° is a practice used to prevent ventilator-associated pneumonia (VAP) and in the care of neurological patients. The position at 0º should be avoided even during daily procedures such as physical therapy and nursing care17, 20 - 23.
METHODOLOGY
This is a longitudinal, analytical and quantitative approach study. Data collection was performed in four ICUs of a large hospital in the northwest. Three of these units meet the clinical and surgical patients of various specialties and one of them serves only to coronary heart disease and clinical and surgical patients, totaling 78 beds. Data were collected in three shifts, morning, afternoon and evening, 13 patients per shift, a total of 39 individuals per unit. There were three months of data collection to obtain the same number of measures in all units and in all shifts. The collection took place from August to November 2013.
This study included adults older than 18 years, of both sexes, who needed verification of PVC in therapeutic practice after passing the catheter through the jugular or sub-clavian with the position confirmed by imaging superior vein cave.
The measurement was taken in subjects monitored with a pressure transducer, the possibility of moving the plate to zero, in the water column values as well as the glued tape values, when removed deteriorates and prevents reuse. Adult subjects were included for data analysis allow a homogeneous group and also to prevent excessive fluid infusion in children and neonates, the number of measures proposed. Individuals under hemodialysis procedure checks that were not in the supine position, with respiratory distress, hemodynamic instability, contraindication to change the headboard bed and using the PVC system in the water column were excluded from the study.
In the hospital studied the standardization and systematization of the routines are done by naming Standard Operating Procedure (SOP), available in computerized system, which are recorded all the techniques performed by the nursing staff. Among the existing SOPs, there is a specific on verification and monitoring of PVC describes the measurement with the head of the bed to 30 degrees.
The used data collection instrument contained ICU identification, turn, angulation and PVC found at measurements at 0º, 30º and 45º positioned by the researcher.
The first check was performed with pressure transducer in the angulation found at the time of data collection, i.e., placed by units of nursing staff, without resetting the system. The following readings were performed on the three proposals angulation (0thereof, 30th, 45), at the same time, with one-minute interval between checks, with zeroing after positioning. The correct angulation were obtained using the protractor, considering 30 inside the bed, in contact with the mattress. In all measures, the patient was supine.
The physiological zero has been identified by positioning one end of the zeroing rule in the fourth intercostal space in the mid-axillary line and the other end into the pressure transducer. The subjects were in a supine position, with no cushions or pillows. The necessary materials were previously installed by the local team, they are: pressure transducer, pressurizer, saline (SF) 0.9% 250 ml or 500 ml, multi parameter monitor and invasive pressure cable. Measurements were obtained in mm Hg.
This study met the Resolution of the National Health Council (CNS) in.466/12. The Research Ethics Committee (CEP) under No. 168,807 approved it. The committee waived the free and informed consent.
The data were presented in absolute numbers and percentages. Continuous variables were analyzed using the Mann-Whitney test, appropriate to ascertain whether the medians of two continuous and independent populations are equal. The nonparametric data were analyzed using the Wilcoxon test to be applied for symmetric distribution of samples. P values <0.05 were considered significant.
The association between measures of PVC were established by analysis of the Pearson correlation coefficient (r) which is a measure of the association of power between two variables with values between - 1 and 1. A positive correlation indicates that both variables increase or decrease together, while negative indicates that while one variable increases the other decreases and vice versa. Coefficient close to zero indicates no correlation between the variables. The t-test is used to determine whether the correlation coefficient is significantly different from zero and that therefore no evidence of association between the two variables.
RESULTS AND DISCUSSION
The sample consisted of 156 individuals and 654 PVC measurements, as four measures were performed with each patient. Of these, only two had a prescription to keep the head of the bed at 45 degrees, the others should, according to the hospital routine, being with the head to the 30º. But 87 (54%) of patients were in angles different from 30º.
The elevation of the head of the bed at 30 or 45 is a common practice in the ICU for the prevention of VAP by decreasing the risk of gastrointestinal content aspiration or discharge or nasopharyngeal and an improvement in ventilation that patients have these positions8, 20 - 22. Neurological patients may also benefit from elevation of the head, because the position prevents venous stasis and facilitates cerebral venous drainage23.
In the hospital studied the measure of PVC should be performed, according to the hospital POP, with the patient 30 seeking to decrease the health problems. One of the probable reasons for the differences in angulation found is in identifying the angle using the protractor, it is a manual process and prone to errors in the hospital several beds are electronic and provide different angles, but are various brands and models and there are differences of height at the same angle from one bed to another.
Even with the benefits of elevation of the head, the practical maintenance is a challenge, requiring the adoption of standards and routines by the nursing staff, and other strategies and interventions to achieve the expected results19. In describing, the procedure should show great detail in the sequence. For example, where the exchanger should be positioned, the angle in relation to the bed (below or above the mattress). The location of the axis phlebostatic or physiological zero point should be well described.
The standardization of a clear and easy protocol allows data to be obtained and analyzed in the same light. Knowledge must be shared by nursing staff, seeking completeness in assistance and the involvement of everyone in this process of looking for a safe care that provides welfare to the patient, so the staff should understand the importance of the steps involved and be in the labor process, and their doubts resolved, perceptions and valued experiences24.
The supine position with the head of the bed 0º is indicated in the literature for verification of PVC and its values are considered reliable4But as this position can bring risks to the patient17, 20 – 22. The value obtained at 0º was compared with the figures for the headboard of maintenance that are 30º or 45º.
According to the Mann Whitney test there was not significance in the values of PVC between 0º and 30º, the P values were> 0.05 (with power of 5% significance), i.e. it did not identify significant differences in the values of pressure between the two angles. Other data reinforcing this information are the results of Pearson's correlation coefficient showing that verification of PVC with the headboard at 0º and 30º can be accomplished without compromising the obtained results. The values can not be identical but also change in the two angles. The correlation coefficient of Pearson (r) obtained was 0.66 and P <0.0001 (with power of 5% significance), which means that correlation between the measures is strong, as shown in Figure 1.
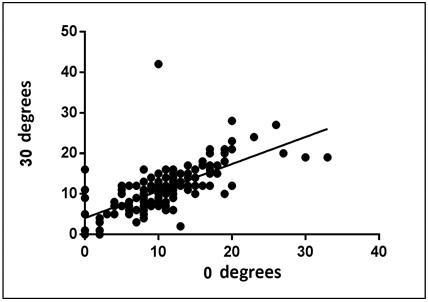
FIGURE 1:
Correlation between PVCs at 0o and 30o (bed head). São José do Rio Preto, 2013
For pressure values measured between 0º and 45º, the Mann-Whitney test showed no significance in CVP, the results P> 0.05 (with a power of 5% significance), or was not identified as significant differences in pressure values between the two angles. However, this finding was not supported by the Pearson correlation coefficient showing a weak correlation between the measurements when a changes to another can not change. The value obtained Pearson was 0.086, and according to the value of P = 0.2841 (with power of 5% significance) this result shows little association between variables, making the obtained data not reliable for measuring pressure, compared to the 0 ° angle, as shown in Figure 2.
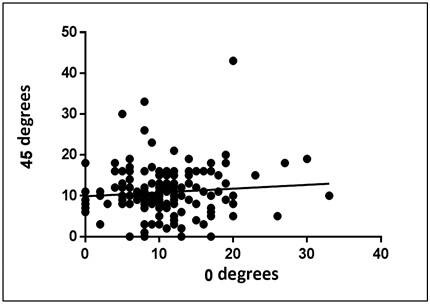
FIGURE 2:
Correlation between PVCs at 0o and 45o (bed head). São José do Rio Preto, 2013
As previously said, the continued high head of the bed is a common and necessary practice in ICU8, 20 - 23. According to the data obtained from the research, if the patient requires monitoring of PVC, the measurement with the head of the bed at 30º showed reliable results and can be maintained without compromising the obtained values. However, when the patient needs the increase to 45º, it is important to consider that the value of the PVC is not trusted and may not express the actual changes of pressure.
There zeroing recommendation system before each measurement, as pressure transducers are sensitive and may change, affecting the results4. But, according to the Wilcoxon test applied to the variables, there was no significant difference between the amounts in angulation of 30 and 45 and the measures after repositioning and zeroing by the researcher, the same elevations with P> 0.0001 (with power of 5% meaningfulness). Zeroing the system did not change the values of PVC in any significant way, but it was not possible to know at what time the last zeroing was made by the ICU staff because the parameter is not noted by the nursing team in the patient's record. Worth noting there is he importance of training and training of staff involved in patient care. The ICU is an environment with many technologies and lack of training and knowledge can interfere with the quality of care25.
Obtaining reliable figures is subject to systematization and the team technical maintenance, ensuring that all steps are performed in the same manner of nursing, the analysis of the results under the same parameters of normality by the medical team, the clinical status of the patient and knowledge of the evaluator in pathophysiology11.
Therefore, it is necessary to seek evidence on the procedure and measurement of PVC according to the reality of each service, and the establishment of protocols to ensure systematization of technical research and the best way to gain knowledge in order to provide safer care26.
A single PVC measure alone does not provide sufficient data for decision making, regardless of the value. Ideally, the analysis of values, based on systematic measurements, after interventions such as vasoactive drugs, inotropic or volume of evidence associated with the submitted clinical2,4,17,27.
CONCLUSION
The PVC can be checked with the headboard at 0º and 30º, with the patient supine without cushions or pillows, with leveling and zeroing in the fourth intercostal space in the mid-axillary line, because the values have positive linear correlation, or is, although the values are not identical when one changes by increasing or decreasing the other monitors the change. Therefore, it is essential that the same technique is used in all checks so there is no interference in the results which may compromise the analysis.
The values of PVC at 0º and 45º show a correlation between the measures, indicating little association between the variables, i.e., the changes can not also happen in these two angles, making the data unreliable.
This study presents the limitation of measurement describing only a specific technical measure of PVC. Further study is needed to identify whether there are differences between the various forms of performing the procedure, and if the values change according to the standard technique.
REFERENCES
1. Ministério da Saúde (Br). RDC nº 307, Regulamento técnico para planejamento, programação, elaboração e avaliação de projetos físicos de estabelecimentos assistenciais de saúde. Brasília (DF); 2002.
2. Dias FS, Rezende E, Mendes CL, Réa-Neto A, David CM, Schettino G, et al. I Consenso brasileiro de monitorização e suporte hemodinâmico: parte II monitorização hemodinâmica básica e cateter de artéria pulmonar. Rev bras ter intensiva. 2006; 18:63-77.
3. Busse L, Davison DL, Junker C, Chawla LS. Hemodynamic monitoring in the critical care environment. Adv Chronic Kidney Dis. 2013; 20:21-9.
4. Scales K. Central venous pressure monitoring in clinical pratice. Nurs Stand. 2010; 24:49-55.
5. Cintra EA, Nischide VM, Nunes WA. Assistência de enfermagem ao paciente gravemente enfermo. 2ª ed. São Paulo: Atheneu; 2005.
6. Headley JM. Invasive hemodynamic monitoring: physiological principles and clinical applications. Irvine: Eduards Lifesciences; 2001.
7. Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of the seven mares. Chest. 2008; 134:172-8.
8. Galvão ECF, Puschel VAA. Aplicativo multimídia em plataforma móvel para o ensino da mensuração da pressão venosa central. Rev esc enferm USP. 2012; 46:107-15.
9. Pacheco SS, Machado MN, Amorin RC, Rol JL, Corrêa LCL, Takakura IT, et al. Pressão venosa central em cateter femoral: correlação com acesso superior após cirurgia cardíaca. Rev bras cir cardiovasc. 2008; 23:488-93.
10. Magder S. Central venous pressure: useful but not so simple measurement. Crit Care Med. 2006; 34:2224-7.
11. Cole E. Measuring central venous pressure. Nurs Stand. 2007; 22(7):40-2.
12. Peterson KJ. Measuring central venous pressure with a triple-lumen catheter. Crit Care Nurs. 2012; 32:62-4.
13. Pedrolo E, Santos MC, Oliveira GLR, Mingorance P, Danski MTR, Boostel R. Curativo impregnado com clorexidine para cateter venoso central: análise de teste piloto. Rev enferm UERJ. 2014; 22:760-4.
14. Oliveira Filho GR, Bernal REJ, Pivatto SL, Tomasi AT, Soares LF, Helayel PE. A articulação acrômio-clavicular como ponto de referência alternativo para o nível flebostático. Rev bras anestesiol. 2001; 51:511-7.
15. Ramos FJS, Azevedo LCP. Avaliação da responsividade a volumes em pacientes sob ventilação espontânea. Rev bras ter intensiva. 2009; 21:212-8.
16. Belela ASC, Pedreira MLG, Peterlini MAS, Kusahara DM, Carvalho WB, Gentil GC. Variabilidade na determinação do ponto externo de referência para a medida de pressão venosa central em crianças. J Pediatr (Rio J.). 2006; 82:389-94.
17. Dellinger RP, Levy MM, Rhodes A, Djillali A, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41:580-637.
18. Ryu TH, Jung JY, Choi DL, Han YS, Kim JD, Kim JH. Optimal central venous pressure during the neohepatic phase to decrease peak portal vein flow velocity for the prevention of portal hyperperfusion in patients undergoing living donor liver transplantation. Transplant Proc. 2015; 47:1194-8.
19. Lee HI, Jeung KW, Jung HY, Lee SG. Estimation of central venous pressure using inferior vena caval pressure from a femoral endovascular cooling catheter. Am J Emerg Med. 2013; 31:240-3.
20. Institute for Healthcare Improvement [site de Internet]. How-to guide: prevent ventilator-associated pneumonia. [cited 2015 Apr 12] Available from: http://www.ihi.org/resources/pages/tools/howtoguidepreventvap.aspx
21. Mietto C, Pinciroli R, Pharm DNP, Berra L. Ventilator associated pneumonia: evolving definitions and preventive strategies. Respir care. 2013; 58:990-1007.
22. Barbas CSV, Ísola AM, Farias AMC, Cavalcanti AB, Gama AMC, Duarte ACM, et al. Recomendações brasileiras de ventilação mecânica 2013: parte 2. Rev bras ter intensiva. 2014; 26:215-39.
23. Alcântara TFDL, Marques IR, Avanços na monitorização neurológica intensiva: implicações para a enfermagem. Rev bras enferm. 2009; 62:894-900.
24. Montanha D, Peduzzi M. Educação permanente em enfermagem: levantamento de necessidades e resultados esperados segundo a concepção dos trabalhadores. Rev esc enferm USP. 2010; 44:597-604.
25. Perez Junior EF, Oliveira EB, Souza NVDO, Lisboa MTL, Silvino ZR. Segurança no desempenho e minimização de riscos em terapia intensiva: tecnologias duras. Rev enferm UERJ. 2014; 22:327-33.
26. Shekelle PG, Pronovost PJ, Wachter RM, McDonald KM, Schoelles K, Dy MS, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med. 2013; 158:365-8.
27. Magder S. Bench-to-bedside review: an approach to hemodynamic monitoring: Guyton at the bedside. Crit Care. 2012; 16:236.