(*) P-Value Fisher's Exact Test = 0.1675.
(**) We considered N: 395 for this analysis, considering that in 2 questionnaires the data concerning abdominal circumference were not filled.
ORIGINAL RESEARCH
Associations between blood pressure, and mid-upper arm and waist circumferences in individuals with high blood pressure
Silvana Maria Coelho Leite FavaI; Patrícia Costa dos Santos da SilvaII; Juliana Pereira MachadoIII; Jaqueline de LimaIV; Larissa Lucas VieiraV; Eugenia Velludo VeigaVI
I
Ph.D. in Health Science. Professor of the Nursing School at the Federal
University of Alfenas. Minas Gerais, Brazil. Email: silvanalf2005@yahoo.com.br
II
Post-Ph.D. of the Nursing Program at the Federal University of Alfenas.
Minas Gerais, Brazil. E-mail:
patriciacostaunifenas@hotmail.com
III
Ph.D. in Health Science. Professor at the University of São Paulo. Ribeirão
Preto, São Paulo, Brazil. E-mail: jpmachado@usp.br
IV
Nursing Student at the University of Alfenas. Minas Gerais, Brazil. E-mail: jaque_limma@yahoo.com.br
V
Nursing Student at the Federal University of Alfenas. Minas Gerais, Brazil.
E-mail:
larissavieira100@hotmail.com
VI
Ph.D. in Nursing. Professor at the University of São Paulo.
Ribeirão Preto, São Paulo. E-mail: eeveiga@eerp.usp.br
DOI: http://dx.doi.org/10.12957/reuerj.2016.14500
ABSTRACT
Objective: to analyze the associations between blood pressure, and mid-upper arm and waist circumferences in adults with systemic arterial hypertension (SAH). Method: this quantitative, descriptive, cross-sectional study examined 397 individuals in the Family Health Strategy in Minas Gerais. Data was collected using validated instruments during home visits in 2013 and 2014, when anthropometric and blood pressure measurements were taken. Chi-square and Fisher's exact tests were applied. Results: 41.1% of participants with mid-upper arm circumference equal to or greater than 27 cm had blood pressure values equal to or greater than 140/90 mmHg, and 38.6% of those with increased-risk or much-increased-risk waist circumference had blood pressure equal to or greater than 140/90 mmHg. Conclusion: although the associations showed no statistical significance, they do constitute important criteria for assessing not only SAH, but also risk factors for other cardiovascular conditions.
Keywords: Arterial pressure; hypertension; Mid-upper arm circumference; abdominal circumference.
INTRODUCTION
With the high population growing, caused by the continuous reduction in mortality rates, it appears that the number of people with weaknesses arising from chronic conditions tends to increase. Among them, the Non-communicable Chronic Diseases (NCDs) are highlighted, in particular, the systemic arterial hypertension (SAH), which significantly worsens the health of the population and causes irreparable damage to the autonomy, independence, and loss of quality of life.
Added to the magnitude of the problem, there is the high prevalence of hypertension, according to national data, reaching more than 50% of individuals 60 to 69 years old and 75% for those over 70, identified as a priority on the national health agenda1.
Although it was a recommendation of the authors, few studies evaluate the distribution of fat in the brachial region as a risk factor for hypertension. Given the gaps in the literature, it was proposed to conduct this study to examine the associations between blood pressure (BP), the measurement of the arm circumference (AC) and wrist circumference (WC) in adults with hypertension.
LITERATURE REVIEW
SAH is considered a multi-factorial clinical condition characterized by high blood pressure and its prevalence is related to obesity, among other factor1,2.
Obesity is characterized by the accumulation of localized or generalized fatty tissue due to nutritional imbalance, with or without the inherent factors of the person3,4.
The localized fat measurements provide an estimate of central adiposity and have been advocated as one of the risk factors and complications for cardiovascular diseases3-5.
The relationship between body fat distribution and blood pressure (BP) has been widely discussed, and research results suggest that the distribution of body fat can modulate the correlation between body mass index (BMI) and BP6- 8.
Therefore, circumferences of the arm, neck and wrist have been used to estimate BMI more accurately9. However, the measurement of the AC has been adopted in the studies primarily as a parameter for determining the width of the cuff for blood pressure measurement9,10. This measure is part of the protocol recommended by scientific societies for measurement of arterial pressure, and the proper cuff must be used, that with the inflatable chamber (cuff) adjustable to the width of the individual´s arm.
AC is the midpoint between the distance from the olecranon and the acromion and by this measurement, the cuff corresponding to at least 40% of the arm length and the length of at least 80% of the circumference must be chosen1.
The incorrect circumference assessment can influence the values of BP, causing inaccurate results11.
Study on BP control concluded that the discrepancy between the cuff size and arm circumference might result in misdiagnosis and inadequate treatment10. This was found in a study developed with adolescent workers. They found that in women, blood pressure values were consistently lower than those observed in men, with a statistical difference in the two cuff widths used. Although several anthropometric measurements have been used as the AC and WC, the most significant were BMI and WC, regardless of age and gender. Experts suggest the need to conduct similar studies to try to clarify these findings12. A study conducted with people 10-18 years old to identify the association between anthropometric variables and blood pressure levels found an association between circumferences and waist skin folds and blood pressure levels increased in the subjects of the sample13.
METHODOLOGY
This is a descriptive, cross-sectional study with a quantitative approach carried out from June 2013 to March 2014. A cross-sectional study is a static X-ray of what occurs at a given time. It is recommended to estimate the frequency with which a particular event is manifested in a particular population at a particular time14.
The study population consisted of people enrolled in a family health strategy unit (FHSU) of the city of Minas Gerais, with 2599 people, including 1207 men and 1392 women. Of this total, 1,956 were 18 years old and above, with 1066 women and 890 men, of whom 512 (26.1%) had a diagnosis of hypertension, with 210 men and 302 women, which was the target of interest for the development of this study.
Of the 512 people with hypertension, 443 were randomly selected for the study, using the OpenEpi, version 2. Of the 443 people, 46 did not participate for different reasons: Eight died, 12 changed address, two did not have cognitive conditions to participate, 14 were not found at the addresses and 10 refused to participate in the study. Thus, the study sample was composed by 397. People who had conditions that would hinder their participation in the day of the interview, such as hospitalization, cognitive changes and/or not being able to provide information were excluded.
According to the legal provisions of the National Health Council, the study was approved by the Ethics Committee of the University of São Paulo Nursing School under the CAAE number: 02313012.4.0000.5393.
Data were collected by a student of the 7th period Nursing Graduation and by nurses. Training was conducted by the researchers responsible for the study for the uniformity of technical and procedural conduct (assessment measures), conducting interviews and questionnaire. Data were collected at the pre-scheduled home visit, through a semi-structured questionnaire validated with questions related to socio-demographic characteristics, cultural and clinic, including spaces for the records of the measures of AC, WC, and BP.
The AC measure was performed with an inelastic tape measure and taking as reference the midpoint between the olecranon and the acromion, supported at heart level (fourth intercostal space) with the patient seated and the arm flexed at 90º15. An adult cuff was used to measure AC to 31 cm, while for values equal or above 32 cm a large adult cuff size was used16. In special situations such as arterial catheterization or presence plaster cast, the measurement was performed only in one arm11.
WC measurement was performed using an inelastic tape positioned at the midpoint between the last rib and upper iliac crest17,18. The cutoff points for WC noted the degree of risk for cardiovascular disease: increased risk for women (WC> 88 cm) and men (WC> 102 cm)1 . For BP measurement, the protocol of the VI Brazilian Guidelines on Hypertension using the automatic digital OMRON HEM - 742, was adopted, validated by the Association for the Advancement of Medical Instrumentation and British Hypertension Society for International research19, cuffs in adult sizes, and large adult, according to the measure of AC15. BP was measured three times consecutively in each patient with a minimum interval of one minute between the measured by reference to the arm in which the BP was higher. The mean BP was obtained considering the last two higher measurements in every person with hypertension. People who had BP less than 140/90 mmHg were considered normotensive2.
Data were organized in tables and stored through the Microsoft Excel computer program and expressed in absolute and percentage values. For statistical analysis, the chi-square test and Fisher exact test were used. The significance level was 0.05.
RESULTS AND DISCUSSION
The socio-demographic and cultural characteristics of the participants showed the predominance of women- 241 (61.5%) with mean age of 64.1 years old (SD = 12.4), aged 19-94 years old, married or stable (57.4%), with level of primary school education incomplete 210 (53.0%), with an average household income of 1765.92, ranging from 250.00 to 10,000.00, and 105 (26.4 %) played remunerated activities, and 260 (65.5) lived with an average of three people. The prevalence of hypertension in women aged over 60 years old is in line with results found in other studies15,16 , justified by the greater concern of women to health and self-care, being a reason for seeking the health service. On the other hand, these findings point to the need to prioritize men in health care to early diagnosis of SAH2.
Studies have shown that the worldwide prevalence of hypertension between men and women is similar, although it is higher in men up to 50 years old and from the 5th decade this relationship becomes reverse 2.
Concerning marital status, similar results were found in a study that evaluated the lifestyle of people with SAH20.
There was an inverse linear association between the prevalence of SAH and education, and people with up to four years of education had a rate of prevalence of hypertension approximately 1.6 times higher when compared to those with eight or more years of study21. The literature suggests that the socioeconomic status of a group of people can be reflected in the context of health, especially cardiovascular disease (CVD) with hypertension as one of the main risk factors21-29. In this regard, a study that followed more than 10,000 French and Irish men for five years showed that the onset of coronary artery disease was associated with low material resources, unemployment, and low education. However, when adjusted for other major risk factors such as smoking, hypertension and BMI and those related to economic status, they lost their value23.
Regarding the occupation, there was predominance in participants mentioning not perform paid work. This finding can be attributed to the fact that the majority of respondents are female, aged over 60 years old and exercise home activities.
Regarding blood pressure, it was found that in 205 (51.6%) participants, the BP values was less than 140/90 mmHg, while in 192 (48.4%) the blood pressure values were equal or over 140/90 mmHg.
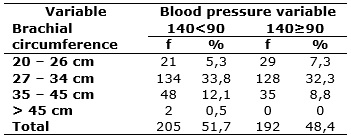
The AC measure of 27-34 cm predominated among the 262 (66.1%) participants. By associating the values of blood pressure measured with the AC, it was found that 41.1% of participants who had a measure of AC less than 27 cm, the BP values were greater or equal to 140/90 mmHg. It was shown that there was no statistically significant difference (p=0.1675) in the association between the extent of AC and pressure levels, as shown in Table 1.
TABLE 1: Association between blood pressure values and gill circumference among people with systemic arterial hypertension attended at a family health strategy unit. Minas Gerais, 2014. (N = 397) (**)
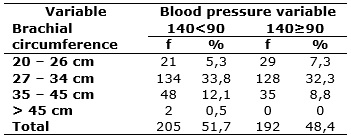
(*) P-Value Fisher's Exact Test = 0.1675.
(**) We considered N: 395 for this analysis, considering that in 2 questionnaires the data concerning abdominal circumference were not filled.
Studies with analysis of these variables are scarce. One of these analyses held in Turkey to investigate the association of different anthropometric measures and blood pressure levels revealed an association between the extent of arm circumference and blood pressure levels. They stressed that this was the first study on this topic12. However, it is not possible to compare the results obtained in this study since it was done with adolescents.
For waist circumference, it was found that 275 (69.6%) participants showed highly increased risk, which is consistent with the results of different studies24-26.
By associating the measure of WC and BP, it was found that among those with increased and very increased risk for the measurement of WC, which corresponds to 38.6%, BP was equal to or greater than 140/90 mm Hg, as shown in Table 2.
TABLE 2: Distribution of abdominal circumference and pressure levels among people with systemic arterial hypertension treated in a family health strategy unit. Minas Gerais, 2014 (N = 395) (**)

(*) P-Value Chi-square test = 0.125.
(**) N = 395 was considered for this analysis, considering that in 2 questionnaires the data on abdominal circumference were not filled.
This is a fact of great importance that should be emphasized in health care since the excess fat has been considered one of the main factors associated to SAH21,27, although it was not statistically significant (p=0.125).
These findings corroborate other studies as conducted in Cuiaba on the association between WC and SAH that points to the need for further research in the Brazilian population to verify the true associations between anthropometric indicators and various outcomes, also studying the best cutoff points for these indicators21.
Most published studies on associations between obesity and mortality in the population have focused only BMI28-30. However, it is known that lean subjects may have an increased risk of CVD and metabolic disorders that arise due to the accumulation of fat in the abdominal region27.
One of the major challenges facing health systems is to find effective strategies to encourage and motivate people with hypertension to change their lifestyle, making them proactive in their treatment31. In this respect, it appears as essential adequately trained for health professionals, given the complexity of this process and its potential in the construction of autonomous subjects and aware of their importance in therapy32.
This study is not out of limitations that while not compromising the results, they should be reported. It should be pointed out that the BP measurement was obtained at a single time and measuring the WC and AC were carried out only by a technique using a single cut point for each measure. Prospective studies are suggested.
CONCLUSION
According to the findings of this study, it is concluded that while measures of AC and WC have not presented statistical significance when associated with blood pressure levels, they must be important criteria for evaluation not only of hypertension but risk factors for other cardiovascular conditions.
The data pointed to the need for further research in the association between these anthropometric indicators and hypertension, and the cutoff points of these indicators for the Brazilian adult population since studies on the subject are different. The study has important contributions to health professionals as fill knowledge gaps given the lack of studies on the association between these variables, especially the measure of AC among Brazilians.
REFERENCES
1.Ministry of Health (Br). Department of Health Care. Department of Primary Care. Strategies for the person's care with chronic disease: hypertension in 2013. Brasília (DF): Ministry of Health; 2013. [cited on April 10 2015]. Available on: http://bvsms.saude.gov.br/bvs/publicacoes/estrategias_cuidado_pessoa_doenca_cronica.pdf
2. Brazilian Society of Cardiology/Brazilian Society of Hypertension/Brazilian Society of Nephrology. VI Brazilian Guidelines on Hypertension. Arq Bras Cardiol. 2010; 95:1-51.
3. Duarte SFP, Reis LAR. Obesity: a multidisciplinary view. Curitiba: CRV; 2012.
4.Henry SL, Barzel B, Wood-Bradley RJ, Burke SL, Cabeça GA, Armitage JA. Developmental origins of obesity-related hypertension. Clin Exp Pharmacol Physiol. 2012; 39:799-06.
5.Direk K, Cecelja M, Astle W, Chowienczyk P, Spector TD, Falchi M, et al. The relationship between DXA-based and anthropometric measures of visceral fat and morbidity in women. BMC Cardiovasc Disord. 2013; 13:13-25.
6.Jordan J, Yumuk V, Schlaich M, Nilsson PM, Zahorska-Markiewicz B, Grassi G, et al. Joint statement of the European Association for the Study of Obesity and the European Society of Hypertension: obesity and difficult to treat arterial hypertension. J Hypertens. 2012; 30:1047-55.
7.Mendes WAA, Carmin SEM, Pinho PM, Silva ACM, Machado LMM, Souza AM. Relationship of anthropometric variables with blood pressure and lipid profiles in adults with chronic diseases. Rev Bras Cardiol. 2012; 25:200-9.
8.Zhang X, Yao S, Sun G, S Yu, Sun Z, Zheng L, C Xu, Li J, Sun Y. Total and abdominal obesity among rural Chinese women and the association with hypertension. Nutrition (London). 2012; 28:46–52.
9.Marshall A, Haboubi N, Jones S. Body mass index estimation from waist, neck and mid-arm circumference. Gastroint Nurs. 2011; 9:37-40.
10.Freitas CCQ, Pantarotto RFR, Costa LRLG. Relationship of arm circumference and cuff size used in Basic Health Units in a city in São Paulo. J Health Sci Inst. 2013; 31:48-52.
11.Veiga EV, Arcuri EAM, Cloutier L, Santos JLF. Blood pressure measurement: arm circumference and cuff size availability. Rev Latino-Am Enfermagem. 2009; 17:455-61.
12.Mazicioglu M, Yalcin B, Ozturk A, Ustunbas H, Kurtoglu S. Anthropometric risk factors for elevated blood pressure in adolescents in Turkey aged 11–17. Pediatr Nephrol. 2010; 25:2327-34.
13.Schommer VA, Barbiero SM, Cesa CC, Oliveira R, Silva AD, Pellanda, LC. Overweight, anthropometric variables and blood pressure in school students 10-18 years old. Arq Bras Cardiol. 2014; 102:312-318.
14.Bastos JLD, Duquia RP. One of the designs more used in epidemiology: a cross-sectional study.Sci Med. 2007; 17: 229-32.
15.Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993; 88:2460-70.
16.Ministry of Health (Br). Department of Health Care. Department of Primary Care. Strategies for the care of people with chronic disease: hypertension in 2006. Brasília (DF): Ministry of Health; 2006. [cited on April 02 2015]. Available on: http://bvsms.saude.gov.br/bvs/publicacoes/estrategias_cuidado_pessoa_doenca_cronica.pdf
17.Janssen I, Mark AE. Separate and combined influence of body mass index and waist circumference on arthritis and knee osteoarthritis. Int J Obes. (London). 2006; 30: 1223-8.
18.Chacur EP, Silva LOe, Luz GCP, Kaminice FD, Cheik NC. Anthropometric and quadriceps angle evaluation in knee osteoarthritis in obese women. Fisioter Pesqui. 2010; 17:220-4.
19.Coleman A, Freeman P, Steel S, Shennan A. Validation of the Omron MX3 Plus oscillometric blood pressure monitoring device according to the European Society of Hypertension International Protocol. Blood Press Monit. 2005; 10:165-8.
20.Silva AM, Silva FD, Mesquita DGG, Veiga EV, Silva PC. Evaluation of depression and lifestyle of elderly hypertensive patients. Rev Eletr Enf [Internet] 2013 [cited on February 24 2015]. 15:368-74. Available on: http://www.revistas.ufg.br/index.php/fen/article/view/17034
21.Barbosa LS, Scala LCN, Ferreira MG. Association between anthropometric markers of body adiposity and hypertension in an adult population of Cuiabá, Mato Grosso. Rev Bras Epidemiol. 2009; 12:237-47.
22.Taveira LF, Pierin AMG. May socioeconomic status influence the characteristics of a group of hypertensive patients? Rev Latino Am-Enfermagem. 2007; 15:929-35.
23.Yarnell J, Yu S, McCrum E, Arveiler D, Hass B, Dallongeville J, et al. Education, socioeconomic and lifestyle factors, and risk of coronary heart disease: the PRIME Study. Int J Epidemiol. 2005; 34(2):268-75.
24.Peixoto MRG, Benício MHDA, Latorre MRDO, Jardim PCBV. Waist circumference and body mass index as predictors of hypertension. Arq Bras Cardiol. 2006; 87:462-70.
25. Figueiredo RC, Franco LJ, Andrade RCG, Foss-Freitas MC, Pace AE, Dal Fabbro AL et al. Obesity and its relationship with risk factors for cardiovascular disease in a Japanese-Brazilian population. Arq Bras Endocrinol Metab [Internet] 2008 [cited on July 04 2016]. 52(9):1474-81. Available on: http://dx.doi.org/10.1590/S0004-27302008000900011
26.Lima PV, Duarte, SFP. Prevalence of obesity in the elderly and its relationship with hypertension and diabetes. InterScientia. 2013; 1: 80-92.
27.Bevilacqua MR, Gimeno SGA. Abdominal obesity in Japanese-Brazilians: which measure is best for predicting all-cause and cardiovascular mortality? Cad Saude Publica. 2011; 27:1986-96.
28.Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008; 359: 2105-20.
29.Massimino FC, Gimeno SGA, Ferreira SRG. All-cause mortality among Japanese-Brazilians according to nutritional characteristics. Cad Saude Publica. 2007; 23: 2145-56.
30.Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009; 373: 1083-96.
31.Cavalari E, Nogueira MS, Hayashida M, Cesarino CB, Alves LMM, Fava SMCL. Factors related to the blood pressure of hypertensive outpatients. Rev Eletr Enf [Internet] 2012 [cited on September 2012]. 14: 603-09. Available on: http://www.fen.ufg.br/revista/v14/n3/v14n3a17htm
32.Felipe GF, Silveira LC, Moreira TMM, Freitas MC. Presence involved and nurse reserve in health education to people with hypertension. Rev enferm UERJ. 2012; 20: 45-9.