RESEARCH ARTICLES
Profile of women crack cocaine users attending a Psychosocial Care Center
Érika Barbosa de Oliveira SilvaI, Adriana Lenho de Figueiredo PereiraII
I
Master in Nurisng by the Nursing school of the State University of Rio de Janeiro. Assistant Professor in the University of Grande Rio. Substitute
Professor in Anna Nery Nursing School. Rio de Janeiro, Brazil. E-mail: erikabos.enf@gmail.com
II
Associate Professor of the Maternal and Child Nursing Department and the Graduate Program in Nursing, State University of Rio de Janeiro. Brazil. E-mail: adrianalenho.uerj@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.13997
ABSTRACT
This exploratory, documentary study to describe the social and clinical profile of women users of cocaine and crack, and to characterize the psychosocial care provided to women at a psychosocial care center, was conducted at the only such center in Duque de Caxias, Rio de Janeiro State, in 2014. The medical records of 113 women treated at this public health service were examined, and the resulting data received descriptive statistical treatment. The cocaine and crack users were predominantly single with juvenile children, no paid employment, presented psychotic or mood disorders, and used other drugs besides cocaine and crack. Psychosocial care was directed to the women's psychic, social and clinical problems, but with the emphasis on individual actions, psychiatric treatment and strengthening the social support network. It is recommended that the therapeutic approach be made more sensitive to gender issues in this clientele.
Keywords: Women's health; gender and health; crack cocaine; mental health.
INTRODUCTION
Drug use affects all kind of people in society and causes various effects on health of populations. Despite the use of cocaine and its derivatives, such as crack and merla have decreased or remained stable in most South American countries, in Brazil there was an increased prevalence of the consumption of this substance, estimated at 1.75% of the population in 20111.
A Brazilian epidemiological survey shows that women are the minority users of cocaine and crack, representing about 40% of users. When considering the data regarding the use of crack and/or similar in 2012, there was a predominance of male users, with 78.7% of the total. This data refers to the consumption of these substances in public or open places to use it, such as "cracolandias", abandoned homes clinics and prison system, and not in private homes 2.
Due to this epidemiological profile, the female on cocaine and crack use has not been prominent in public policy and in health care. Studies of crack consumption in the gender perspective are still incipient3.
The link between gender and mental health is proposed by the National Policy for Integral Assistance to Women (PNAISM), considering that aspects of everyday life of women and overload of responsibilities assumed by them can harm the state of psychological well-being4. Female issues involved in the complexity of the drug use phenomenon, producing challenges for the care of cocaine and crack users.
Psychosocial Care Centers for Alcohol and Drugs (CAPS ad) are specialized services to care for demands arising from the use of such substances, and should provide care by a multidisciplinary team, seeking to understand the socio-cultural reality of these users to give effective answers to specific demands of female gender.
Given the specificities of female gender in addressing the problems related to the use of cocaine and crack, this study was proposed aimed to describe the social and clinical profile of female users of cocaine and crack and identify the characteristics of care provided to women in CAPS ad.
LITERATURE REVIEW
Women have vulnerabilities related to gender issues that expose them to suffering, disease and death in a different way than men. Therefore, the construction of comprehensive care to women´s health requires the establishment of a cross-communication between different areas of knowledge. Cross care covers the production of health and subjectivity, understanding complex phenomenon involving the subject in context of their lives4,5.
With the Psychiatric Reform, Brazilian health system organized support network focused on community care, emphasizing prevention of mental illness, psychosocial rehabilitation and social reintegration of individuals. In this context, the provision of care to people who consume alcohol and other drugs was prioritized in places out of the hospital and interconnected to the health service network6.
CAPS ad is daily care services seeking to promote the potential for the production of health through care focused on the needs of people7,8. This service has multidisciplinary health team, including nursing professionals. This team has the responsibility to prepare, together with the user and their families, a unique treatment plan and according to the daily context of individuals9.
In the construction of the treatment plan, it is recommended to consider the specifics of the female gender. As much as men and women share similar health-disease experiments, women experience them differently because of the distinctive socialization mediated by gender10.
The unique psychosocial care considers the individual and citizen within his life story, in his economic, social and cultural context, and psychological structure. Gender is a sociocultural construct4, so it is essential in the psychosocial approach. Thus, knowing the specifics of female gender among users of cocaine and crack, it contributes to the knowledge of the differences between men and women in addressing substance use and it is essential to establish a fair, comprehensive and effective care for women.
METHODOLOGY
This is an exploratory and documental study in the only CAPS ad in the municipality of Duque de Caxias, located in the Baixada Fluminense, metropolitan region of the State of Rio de Janeiro. This city has an estimated population of 873,921 residents in 2013, and has medium human development index (0.753) 11.
From the total of records of active clients in the service, women´s medical records were highlighted in drug addiction situation and later the records of crack and cocaine women users were selected. Therefore, recorded data of the users of these substances and that they were in regular treatment were included in this study, excluding inactive records, treatment abandonment records treatment or referral to another health service.
The study variables were the social data of women (age, marital status, education level, housing situation, children, type of occupation, income source and involvement with justice); clinical data (admission to the service, participation of the family in the treatment; health problem related to drug use, type of the first substance used and currently consumed, initial age of substance use and crack/cocaine initial age use) and psychosocial care data (social problems, psychological disorders, coping with addiction and women´s health).
Data collection was carried out in May 2014 and a script structured of document analysis was used. The data were collected in a computerized database in Microsoft Excel OfficeÒ2003. Later, the data were tabulated and submitted to descriptive statistics. The analysis considered the absolute frequencies and percentages, confronted with the scientific literature on the subject investigated.
The study observed the ethical principles and obtained a favorable opinion of the Ethics Committee in Research of the State University of Rio de Janeiro (COEP / UERJ) No 628 205.
RESULTS AND DISCUSSION
Among 361 records of active clients in the service, it was found that 158 records were from women treated at CAPS ad. From all these, 113 (100%) records belonged to cocaine and crack women users assisted in the institution.
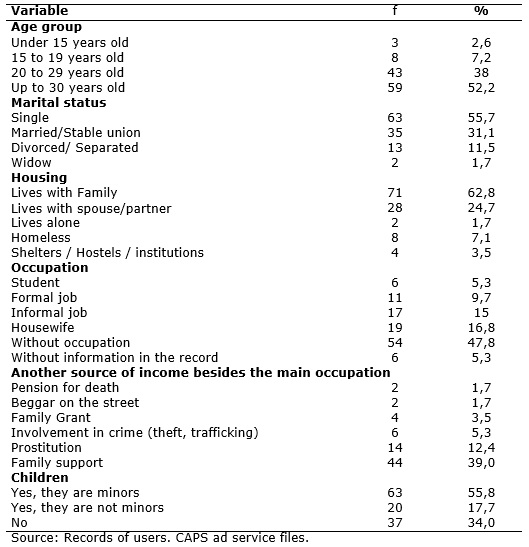
From the analysis of the medical records of those users, the predominance of adult women over 30 years old (52.2%) was identified, followed by those aged 20-29 years old (38%). Most of them are single (55.7%) with minor children (55.8%) who lives with the family (62.4%). Those without paid job were highlighted (47.8%) and dependent on the family income for their support (39%), as shown in Table 1.
TABLE 1:
Socio-demographic profile of crack and cocaine users in treatment at CAPS ad. Municipality of Duque de Caxias, Rio de Janeiro, May, 2014. (N=113)
Men are the primary users of cocaine and crack consumption in public spaces in Brazil, with the proportion of 78.7%, as well as the most clients assisted in CAPS ad2. A research of this type of service in southern Brazil found the percentage of 82.1% for male users12. Women on treatment in CAPS ad where this study was developed, represent 43.8% of the total of clients. Considering only users of cocaine and crack, this group was 31.3% of the 361 active records in the service. This greater female representation may denote a specificity of gender distribution of the population of cocaine and crack users in the municipality of Duque de Caxias, as well as raising that the issues related to gender are involved.
The gender variable does not only reveals epidemiological data, but suggests that gender relations in mental health need to be considered in therapeutic projects. Gender is structuring of power relations and determines the health-disease process4. Therefore, it is necessary to understand the social reality of the care´s individual in the gender perspective.
The increasing indicators of the use of psychoactive drugs among women was found in Brazilian studies, being a challenge to public health and specialized services13. The construction of therapeutic projects must consider the needs of these women, who are single, mothers, in fertile age without labor occupation, with own income and sometimes may be involved in situations of violence and prostitution as an access to the drug use. Therefore, therapeutic strategies should include access to qualifying for the labor market, the acquisition of own income, care maintenance and custody of the minor children, among others.
The prevalence of single women with low education level, between the 4th and the 8th grade of elementary school are features observed in the profile of users of these substances in the country2, which hinders access to work and acquire income. In this study, we could not identify this figure because of its absence in 52.2% of the analyzed records.
Considering the occupation and income, studies have found that the crack and similar users present unemployment situation and come from broken and low-income families3. This economic status was also observed in the results presented here, since 69.9 % of the records of cocaine and crack women users were without paid employment.
Substance use by women is related to cultural, social, family and individual context, involving risk factors such as body use for drugs, prostitution and sexually transmitted diseases13. In the records analyzed, 12.4% women were involved in prostitution and 5.3% with crime. However, the high percentage of women without their own income and depending on family income raises the need to understand how these women use drugs and what implications causes on their lives. Investigating ways of drug acquisition is important for the preservation of health and psychosocial integrity, since studies have found that a considerable portion of users have involvement with robbery practices, thefts, assaults, homelessness, prostitution and exchanging sex for drugs2,13.
In the analysis of clinical characteristics of cocaine and crack users, it was found that women´s access to treatment in CAPS ad was mainly by reference by other health service - 42 (37.2%) and indication friend or family member - 22 (17.7%). It should be noted that this data was absent in 22 (19.5%) of researched records.
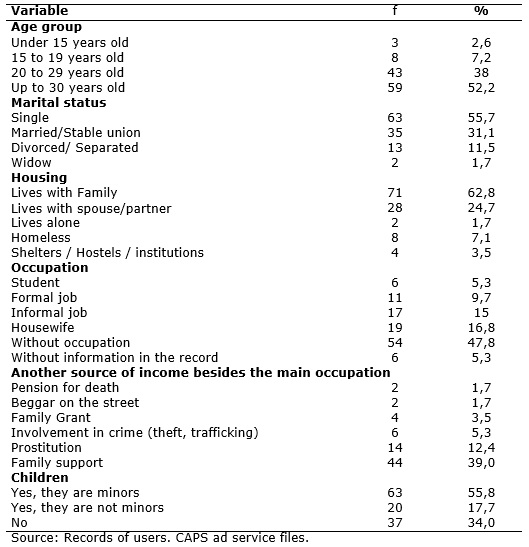
As for family participation in treatment, there were 86 (76%) records with positive family support in the therapeutic process. In 82 (75.6%) records, there was other health problems related to the use of cocaine and crack, especially for psychotic disorders - 48 (42.5%) and mood - 23 (20.3%).
On other mental disorders associated with substance use, there were 6 to 8% of the population involved14. In addition to increasing the potential of depressive symptoms, anxiety and other comorbidities, crack also causes less motivation to change and lower adherence to treatment 13.
In almost all records - 111 (98.3%) – there was consumption of other drugs together with the use of cocaine and crack with tobacco prevalence (77%), cannabis (63%) and alcohol (45.1 %). The use of multiple drugs in a short period and, simultaneously, in the current pattern of compulsive substance use, gradually replacing the exclusive use15. Nicotine, alcohol and marijuana are more associated drugs to cocaine and crack in the country 12.
The multiuse of substances begins in young people under 19 years old, revealing the importance of preventive measures in adolescence. The first experiences with drugs occur mostly in this phase of life, at which individuals are most vulnerable, requiring the identification of socio-cultural and psychological factors predisposing to substance abuse16.
Searching their role within their social circle, the adolescent may be exposed to drug addiction, whether by stimulation of colleagues, family, advertising appeal, or even curiosity17. Nevertheless, during the adolescent training some factors can be protective for the use of substances, such as strengthening emotional bonds within the family, involvement in school activities, and access to information about drug use, among others13.
Considering the age and type of first drug use, the period of adolescence is the time to start the use of psychoactive substances, with a predominance of the age groups under 15-49 years old (43.4%) and between 15 and 19 years old - 34 (30%). Marijuana was the main drug involved in the first consumer with 41 (36.3%), followed by alcohol with 21 (18.6%). This period of life was also one in which most women began to cocaine and crack, as can be seen in Table 2.
TABLE 2:
Clinical profile of crack and cocaine users in treatment in CAPS ad. Municipality of Duque de Caxias, Rio de Janeiro, May de 2014. (N=113)
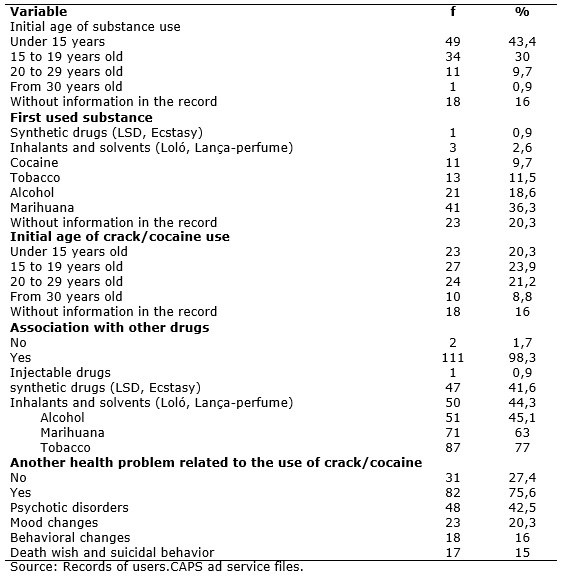
In the care described in the medical records, the individual consultations with health professionals were the most important in the therapeutic plan of users, highlighting the actions to mental health problems, as monitoring of psychiatric - 112 (99.1%); social, as monitoring of social worker - 94 (83.2%); and clinicians, as monitoring for neurologist - 16 (14.2%), as shown in Table 3. Other care strategies have also been adopted, such as strengthening the social support network (69%), the prescription of psychotropic drugs (69%) for mental disorders and to a lesser extent and participation in women group (44.3%).
TABLE 3:
Care described in the individual treatment plan of crack/cocaine women users at CAPS ad. In themunicipalityof Duque de Caxias, Rio de Janeiro, May, 2014.
(N=113)
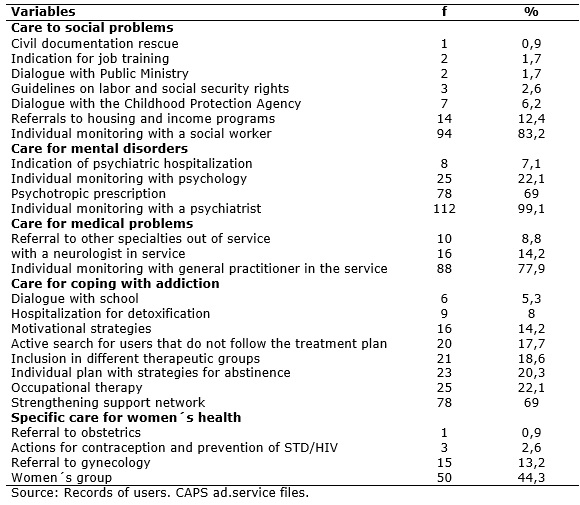
During the documentary review, it was found that care plans or therapeutic projects were not explicitly described in the medical records. Records aimed at solving social problems, recovery of citizenship and strengthening social support network for each user were found. Registered care also denote the primacy of the individual actions, rather than a collective and multidisciplinary construction. Despite the multidisciplinary care not exclude care and individual consultations, it needs to be built collectively to expand the knowledge of the person being cared, the socio-cultural context and relationship with the drug.
The assistance offered by CAPS ad should include individual consultation, group care, therapeutic workshops, home visits, nursing and outpatient detoxification, and companionship spaces7. Therefore, psychic, emotional, socio-cultural and family dimensions of the person being cared must be addressed.
Therapeutic groups are important care strategies, but only 18.6% of the records analyzed showed the participation of these women in various therapeutic groups and 44.3% in women group. The therapeutic groups can be educational, reflection and support, and allow the individual to awareness as a social and subject co-participant of the therapeutic process18. Therefore, the low frequency of these care strategies can involve adversely the quality and effectiveness of psychosocial care provided to female clients in CAPS ad investigated.
CONCLUSION
Cocaine and crack women users of CAPS ad are predominantly single and mothers with minor children who do not have paid job and living with the family. They also have psychotic or mood changes, use other drugs together with the use of these substances and demonstrate social and clinical profile similar to national studies on this population group.
The psychosocial care provided in CAPS ad is directed to mental health, social and clinical problems of women, with an emphasis on individual actions in psychiatric treatment and strengthening social support network for coping with addiction.
Despite the limitations of a documentary study, the results also indicate the need to improve the annotations of professionals in the medical records, because of underreporting of important data for the therapeutic project.
It is necessary further research on women involved in the abuse use of cocaine and crack, the care provided by nursing and the adoption of the gender approach in psychosocial care due to the singularities of those female clients.
REFERENCES
1.Organização das Nações Unidas. Escritório das Nações Unidas Sobre Drogas e Crimes. Relatório Mundial sobre Drogas, 2013. NovaYork: ONU; 2013.
2.Bastos FI, Bertoni N, organizadores. Pesquisa Nacional sobre o Uso de Crack: quem são os usuários de crack e/ou similares do Brasil? Quantos são nas capitais brasileiras? Rio de Janeiro: ICICT/FIOCRUZ; 2014.
3.Souza RF, Padovani RC, Tucci AM. Consumo de crack a partir das perspectivas de gênero e vulnerabilidade: uma revisão sobre o fenômeno. Saúde debate. 2014; 38:379-92.
4.Ministério da Saúde (Br). Política Nacional de Atenção Integral à Saúde da Mulher: princípios e diretrizes. Brasília (DF): Editora MS; 2011.
5.Pedroso RT, Vieira MEM. Humanização das práticas de saúde: transversalizar em defesa da vida. Interface (Botucatu).2009; 13:695-700.
6.Ministério da Saúde (Br). A Política do Ministério da Saúde para a Atenção Integral a Usuários de Álcool e outras Drogas. 2ªed. Brasília (DF): Editora MS; 2004.
7.Ministério da Saúde (Br).Portaria GM nº 336 de 19 de Fevereiro de 2002. Brasília (DF): Gabinete Ministerial; 2002.
8.Ministério da Saúde (Br). Portaria GM nº 130 de 26 de Janeiro de 2012. Brasília: 2012.
9.Boccardo ACS, Zane FC, Rodrigues S, Mângia EF. O projeto terapêutico singular como estratégia de organização do cuidado nos serviços de saúde mental. Rev Ter Ocup Univ São Paulo. 2011; 22(1):85-92.
10.Lima HP, Braga VAB, Gubert FA. Interface entre gênero e saúde mental no discurso de alcoolistas: estudo qualitativo. Online Braz J Nurs [Internet]. 2010 [citado em 25 nov 2014];9(2). Disponível em: http://www.objnursing.uff.br/index.php/nursing/article/view/j.1676-4285.2010.2907/665
11.Serviço Brasileiro de Apoio a Micro e Pequenas Empresas. Informações socioeconômicas do Município de Duque de Caxias [site de Internet]. Rio de Janeiro: Sebrae; 2011. [citado em 27 nov 2014]. Disponível em: http://201.2.114.147/bds/bds.nsf/3C0F2AE4C6B74D7B83257950005F787B/$File/Duque%20de%20Caxias.pdf
12.Horta RL, Horta BL, Rosset AP, Horta Cl. Perfil dos usuários de crack que buscam atendimento em Centros de Atenção Psicossocial. Cad Saúde Pública. 2011; 27: 2263-70.
13.Lima HP, Macedo JQ, Braga VAB, Lemos AM, Silva Júnior IA. Caracterização de drogaditas atendidas em Centro de Atenção Psicossocial álcool e outras drogas: estudo documental. Online braz j nurs [Internet]. 2011 [citado em 24 nov 2014]; 10 (2). Disponível em: http://www.objnursing.uff.br/index.php/nursing/article/view/3257. v.10. n.2, abr.-ago., 2011.
14.Ministério da Saúde (Br). Saúde Mental e Atenção Básica: o vínculo e o diálogo necessários. Brasília (DF): Ministério da Saúde; 2007.
15.Costa LLS, Navas ALGP, Oliveira CCC, Ratto LRC, Carvalho KHP, Silva HR et al. Avaliação da memória operacional fonológica e impulsividade de usuários de drogas atendidos em um centro de atenção integrada à saúde mental. Rev CEFAC. 2012;14: 438-47.
16.Monteiro CFS, Araújo TME, Sousa CMM, Martins MCC, Silva LLL. Adolescentes e o uso de drogas ilícitas: um estudo transversal. Rev enferm UERJ. 2012; 20: 344-8.
17.Brusamarello T. Maftum MA, Mazza VA, Silva AG, Silva TL, Oliveira VC. Papel da família e da escola na prevenção do uso de drogas. Cienc Cuid Saude. 2010; 9:766-73.
18.Bourguignon LN, Guimarães ES, Siqueira MM. A atuação do enfermeiro nos grupos terapêuticos dos Caps ad do Estado do Espírito Santo. Cogitare Enferm. 2010;15: 467-73.