RESEARCH ARTICLES
Cross-cultural adaptation of the end of life comfort questionnaire-patient to Brazilian Portuguese
Liana Amorim Corrêa TrotteI; Claudia Feio da Maia LimaII; Tamires Luciana do Nascimento PenaIII; Antônio Milton Oliveira FerreiraIV; Célia Pereira CaldasV
INurse. PhD in Nursing. Nurse at the National Cardiology Institute of Rio de Janeiro. Rio de Janeiro, Brazil. Email: lianacorrea@ymail.com
IINurse. Doing her PhD at Rio de Janeiro State University, School of Nursing, Graduate Studies Program in Nursing. Rio de Janeiro, Brazil. Email: claudiafeiolima@yahoo.com.br
IIINurse. Degree in Nursing from the Federal University of the State of Rio de Janeiro. Brazil. Email: tamirespenna@bol.com.br
IVNurse. Specialist in Gerontology from Rio de Janeiro State University. Brazil. Email: milton.enf@gmail.com
VNurse. PhD in Nursing. Associate Professor at Rio de Janeiro State University, School of Nursing. Department of Public Health. Rio de Janeiro, Brazil. Email: cepcaldas@gmail.com
ABSTRACT: The objective of this study was to validate the End of Life Comfort Questionnaire-patient in relation to Brazilian Portuguese. The validation consisted of the following steps: translation, synthesis, back-translation, review by a committee of experts, pre-testing and verification of the psychometric properties. Kendall’s W test was used for inter-rater comparison. The final adapted version with 28 statements was administered to heart failure patients receiving care at an outpatient clinic of a hospital specializing in cardiology. The number of Likert Scale items was adapted from six to five, and one word in item 24 was adjusted. There was a Kendall’s W score < 0.5 for one intra-rater reliability item and for five items in the test-retest. Sixty-seven patients were rated, ages 55±11 years; 60% were male. The average sum of correct answers was 96 (Kendall 0.99). In conclusion, the questionnaire was validated for use in Brazil.
Keywords: Heart failure; palliative care; validation studies; nursing.
INTRODUCTION
Heart Failure (HF) is a syndrome that affects 10 out of every 1,000 people over age 65 in the United States of America1. It is considered the definitive pathway for all heart diseases and that it will be the leading cause of death in the world by around 2025.
In 2007, cardiovascular diseases represented the third highest cause of hospitalization in the SUS (Unified Health System), with 1,156,136 admissions. HF is the most frequent cause of hospitalization for cardiovascular diseases2.
With HF, the course of the disease and death are characterized by difficulty in controlling symptoms and high levels of depression. Although progress has been made in treating HF, the disease continues to be one of leading causes of hospitalization in various countries and is associated with high health costs and, especially, poor quality of life3.
People with HF encounter impediments in caring for themselves, caused by progressive physical limitations, difficulties in obtaining social and emotional support, and other situations, due to the chronic nature of the disease.
Nursing is therefore confronted with a growing number of people with HF near the end of life, and there is a clearly a need to improve the control of symptoms and enhance the quality of life of such individuals, through the application of palliative care principles.
From this perspective, the purpose of this study was to validate, in relation to Brazilian Portuguese, the End of Life Comfort Questionnaire – patient (comfort questionnaire regarding end of life planning).
LITERATURE REVIEW
Palliative care is a care philosophy, whose measures seek to improve the overall living conditions of individuals coping with the end of life process4, where promoting comfort and relief from suffering is essential to holistic nursing care.
To promote comfort it is necessary to have a knowledge of basic human needs, in order to enhance relief, serenity and transcendence, based on four contexts of experience (physical, psycho-spiritual, social and environmental)5. Comfort is a specific result, susceptible to change over time. Any consistently applied holistic nursing intervention increases comfort over time. Total comfort is greater than the sum of its parts6.
An article from the literature review, on assessment of quality of life in the context of palliative care, underscored the importance of using standardized and validated scales for different cultures, in order to identify the demands and implement more adequate care in the field of palliative care7.
The use of rating instruments and questionnaires are important resources for research and use in clinical practice, since they allow the effects of the teaching and learning process and possible changes in attitudes of individuals to be measured8. These resources also provide a means to learn about their needs and the conditions for implementing a treatment process more in line with the reality of individuals affected by advanced HF.
METHODOLOGY
This is a cross-sectional instrument validation study, comprising part of the doctoral thesis of the author Liana Trotte. Dr. Katherine Kolcaba, Professor Emeritus of the School of Nursing of the University of Akron, in the United States, granted permission for the End of Life Comfort Questionnaire to be adapted, at the request of the above-mentioned researcher.
The questionnaire entails a comfort evaluation of end of life patients and contains 28 multiple-choice items, characterized by affirmative and negative questions, with no presentation of categories. The Likert scale, with a 1 to 6 range, was used as the rating measure.
The research was conducted from October to December 2011 at the heart failure outpatient clinic of a large hospital specializing in cardiology, in the city of Rio de Janeiro/RJ, with approval from its Research Ethics Committee, Protocol No. 0348/29-08-2011.
The inclusion criteria for the study included: have chronic HF of any etiology in the NYHA functional classes II-IV; both sexes > age 18; be able to sign the Free and Informed Consent Form; with cognitive ability intact.
The study was conducted in two stages: implementation of the steps to determine conceptual, item and semantic equivalences and a assessment.
In the first stage of the study, within the universalist approach9, strategies were applied in order to find the conceptual, item and semantic equivalences10,11. During the evaluation of conceptual and item equivalence, discussions were held with nurses to assess whether the constructs of the original questionnaire were relevant and pertinent to the reality of the Brazilian population.
The original instrument was translated into Portuguese, in two separate translations, by two Brazilians fluent in both languages. The Portuguese translations were back-translated into English by two other independent professionals (one British and the other Brazilian), who had no access to the original instrument. The fifth rater, a Brazilian, formulated a synthesis translation, based on a comparison between the original interview, the translations and the back-translations, without having had any contact with the professionals from the previous steps. All the translators used were sworn translators in Brazil.
A group of nurses with extensive knowledge of HF, comfort theory and the English language examined the synthesis translation. The goal of this step was to better tailor the statements to the target population, without changing the overall meaning of each question from the instrument.
This synthesis translation was administered during a pre-test stage to 15 patients from the HF outpatient clinic of the aforementioned health institution. In the pilot study, a large amount of information was obtained about the patients' understanding of the items being addressed.
The statements in the questionnaire were discussed again with the group of experts, and a few changes were made, so they would be better understood by the target population.
Raosoft® software was used to calculate the sample. It was taken into account that the study population was approximately 300 individuals. It was considered that there would be a normal distribution in the sample and that 70% of this sample would have a good comfort level. An error margin of 10% and a confidence interval of 95% were chosen, resulting, therefore, in a total of 64 patients in order to achieve the goal of the study.
In the second stage of the research, the questionnaire was administered to 67 patients. Although the questionnaire could be filled out alone by the patients, it was decided to conduct face-to-face interviews due to the low educational level of the research subjects. The interval of time between the test and retest was one week, with a final acceptance of 34 patients.
To assess intra-rater reliability, a research assistant was trained, who became proficient in the standardization of the application, encoding and filling out of the responses. To examine this item, comparisons were performed between the questionnaires obtained by the main and assistant researchers.
In turn, test-retest reliability was performed by the main researcher, who used the questionnaire with a one week interval between applications.
The generated data was encoded and stored in a database. The analysis was done using the program Stata v.12 (StataCorp, College Station, Texas - USA / 2011). Descriptive statistics sought to characterize the sample, and to determine reliability, internal inter-rater consistency and test-retest were evaluated. Kendall's W (coefficient of correlation)12, which is a non-parametric statistical test, was used for statistical measurements. It is considered a normalization of the statistic of the Friedman test and can be used to assess agreement between raters. The variation of Kendall's W ranges from 0 (no agreement) to 1 (complete agreement).
The categorical variables were expressed as a percentage or absolute value; the continuous ones as a mean±standard deviation, or medians and 25 and 75 percentiles, according to whether it follows normal distribution or not.
RESULTS
It was necessary to adjust the number of response options in the original Likert Scale from 6 to 5, giving them a classification that would make it easier to understand their meanings. The other change that occurred was the adjustment of a word in the statement corresponding to item 24.
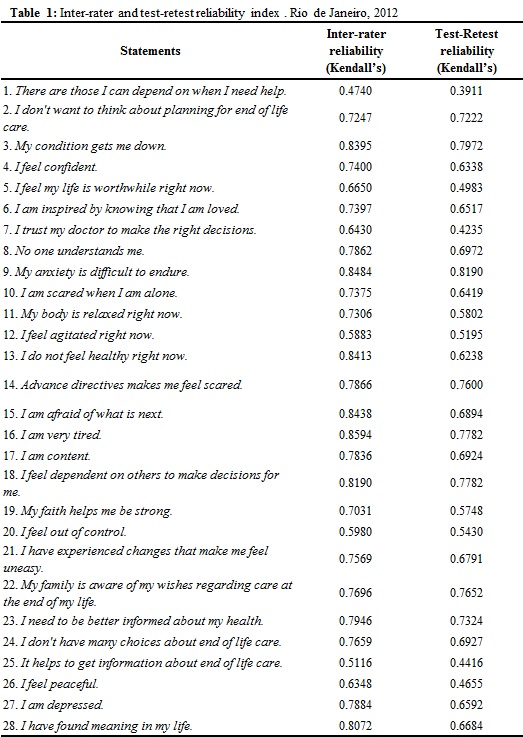
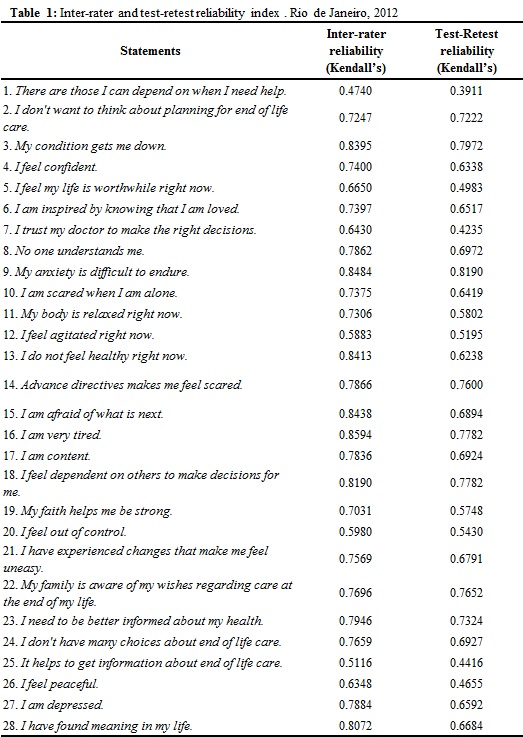
In regards to intra-rater reliability, a Kendall value <0.5 (0.4740) was only noted in item 1, according to Table 1. In the test-retest, there were five items where the Kendall value < 0.5 (item 1: 0.3911; item 5: 0.4983; item 7: 0.4235; item 25: 0.4416; item 26: 0.4655).
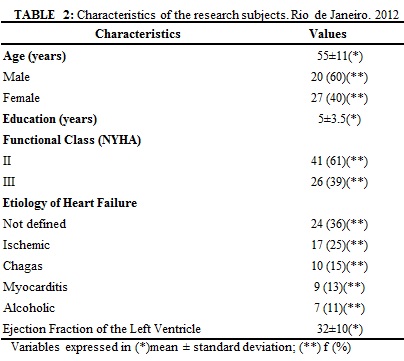
The instrument was administered to a mostly male sample of 67 patients, whose mean age was 55±11. At the time of the interview, 61% were in functional class II of the New York Heart Association (NYHA). Other characteristics can be seen in Table 2.
According to the author of the questionnaire, the higher the sum of the responses, the greater the state of comfort. There are positive and negative statements; for calculation purposes, the values of the negative statements were inverted. In terms of the Brazilian version of the questionnaire, with 28 statements and a Likert scale of 1-5, as response options, the greatest comfort achievable would be 140 and the lowest 28. In the questionnaires administered, the sum of responses obtained varied from 60 to 121, with a mean of 96, according to Table 3.
The reliability among the response patterns of the subjects was evaluated, which yielded a Kendall's W of 0.99, when comparing the sums between the main and assistant rater; whereas, it was 0.9452 between the main rater and retest.
DISCUSSION
After the questionnaire was administered in the pre-test stage, it was only necessary to modify statement 24 to adjust the meaning of the phrase in Portuguese. One of the words in Portuguese was adjusted (Não tenho muitas opções sobre cuidados no fim da vida), with sobre cuidados being replaced by de cuidados.
With respect to the measurement scale used, there was a change in the number of choice options (6 to 5), to make it clearer for the research subjects and to facilitate the description of each option (1- I totally disagree; 2- I disagree; 3- I neither agree nor disagree; 4- I agree, 5- I fully agree).
The instrument used in this study was derived from the version found on Katherine Kolcaba's website (www.thecomfortline.com). The author stated, by email, that this version stemmed from a more complete model that had been tested by four specialists13, and that, to date, there has been no new version.
In terms of intra-rater reliability, it was noted when comparing the average of the sums of the questionnaires administered that the Kendall's W was 0.99, which shows a high level of agreement between them. In evaluating the statements separately, there was only one item (1) that had a Kendall's W <0.5 (0.4740). Therefore, given the high level of agreement, this figure was not deemed to be significant.
With respect to test-retest reliability, the Kendall's W for the sum of the instruments administered was 0.9452. When checking the statements in five items (1, 5, 7, 25 and 26), it was found that the agreement rates were < 0.5 (0.3911; 0.4983; 0.4235; 0.4416; 0.4655), respectively. However, the figures were not considered important, since it is known that the state of comfort related to specific items is variable, based on the individuality and subjectivity of each subject. Since the average sum of the questionnaire items in the retest was similar to the initial application (96.3823±10.0635 x 95.5077±11.5409), it is believed that the values did not affect the validation of the instrument.
In a recent literature review study on instruments that rated the quality of life in the context of palliative care7, there were 13 that evaluated this issue. None were specific to nursing, since the construct is not something for exclusive evaluation of nurses. The need to validate or create instruments for the Brazilian reality was also identified.
The choice of the authors to validate this instrument supports the idea that to establish nursing and promote science it is necessary to make the language used by the profession direct and to institute it in the culture. Nursing theories (theoretical constructs) can play this role through fundamental elements that seek to define, characterize, understand and explain, in an interrelated manner, the phenomena of interest to the profession.
Theories exist to challenge existing practices, generate new approaches to professional practice and reorganize the structure of rules and principles. Furthermore, theories serve to enhance the academic and care practice of nursing14. They potentially determine innovations, developments and/or revolutions in the knowledge and practice of nursing15, in a creative and reflective way, and break with the traditional performance of tasks in the medical process.
Since, until the present, there have been few instruments that seek to evaluate processes in the realm of palliative care, this questionnaire is an important element for the nursing practice, because it stems from a nursing theory and supports the praxis of the profession.
It is considered to be a limitation of this study that the validation was conducted among a specific population in only one setting. It is known that the greater the number of persons involved in similar processes, the greater the likelihood that the instrument will be generalized in large proportions. Another limitation is the fact that although the instrument could be filled out by the subject alone, it was administered in face-to-face interviews, due to the low educational level of the sample surveyed.
CONCLUSION
It can be concluded that the End of Life Comfort Questionnaire - Patient was adapted and validated for Brazilian Portuguese, indicating that it is an appropriate tool for use in the population studied. It is suggested that it be replicated among other groups of patients, in other regions of Brazil, in order to better tailor it to the reality of the country.
REFERENCES
1.Lloyd Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics-2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009; 119:e21-e81.
2.Bocchi EA, Marcondes-Braga FG, Ayub-Ferreira SM, Rohde LE, Oliveira WA, Almeida DR, e cols. Sociedade Brasileira de Cardiologia. III Diretriz Brasileira de Insuficiência Cardíaca Crônica. Arq Bras Cardiol. 2009; 93(1 supl.1):1-71.
3.Barretto ACP, Del Carlo CH, Cardoso JN, Morgado PC, Munhoz RT, Eid M O, et al . Re-hospitalizações e morte por insuficiência cardíaca: índices ainda alarmantes. Arq Bras Cardiol. [periódico na Internet] 2008 [cited on Apr 10, 2013]. 91(5):335-41. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0066-782X2008001700009&lng=pt. http://dx.doi.org/10.1590/S0066-782X2008001700009.
4.World Health Organization. National Cancer Control Programmes: Policies and Managerial Guidelines. 2nd ed. Geneva (SZ): World Health Organization; 2002.
5.Kolcaba K. Evolution of the Mid Range Theory of Comfort for Outcomes Research. Nurs Outlook. 2001; 49(2):86-92.
6.Kolcaba K. Comfort Theory and practice: a vision for holistic care and research. New York: Springer Publishing Company; 2003.
7.Correia FR, De Carlo MMR. Avaliação de qualidade de vida no contexto dos cuidados paliativos: revisão integrativa de literatura. Rev Latino-Am Enfermagem. [periódico na Internet] 2012 [cited on Apr 10, 2014]. 20:401-10. Available at: http://www.scielo.br/scielo.php?pid=S0104-11692012000200025&script=sci_arttext&tlng=pt
8.Torres HC, Virginia AH, Schall VT. Validação dos questionários de conhecimento (DKN-A) e atitude (ATT-19) de Diabetes Mellitus. Rev. Saúde Pública [online]. 2005; 39:906-11.
9.Herdman M, Fox-Rushby J, Badia X. A model of equivalence in the cultural adaptation of HRQoL instruments: the universalist approach. Qual Life Res. 1998; 7:323-35.
10.Lima DA, Lourenço RA. Adaptação para o Português da seção A do Cambridge Examination for Mental Disorders of the Elderly - Revised Version (CAMDEX-R) para o diagnóstico de demência. Cad Saúde Pública. 2010; 26:1345-54.
11.Sanchez MAS, Lourenço RA. Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): adaptação transcultural para uso no Brasil. Cad Saúde Pública. 2009; 25:1455-65.
12.Conover WJ. Practical nonparametric statistics. New York: John Wiley & Sons; 1971.
13.Novak B, Kolcaba K, Steiner R, Dowd T. Measuring comfort in caregivers and patients during late end-of-life care. Am J Hosp Palliat Care. 2001; 18:170-80.
14.Garcia TR, Nóbrega MML. Contribuição das teorias de enfermagem para a construção do conhecimento da área. Rev Bras Enferm. 2004; 57:228-32.
15.Barbro W, Carlsson M. Nursing theory views on how to support the process of ageing. J Adv Nur. 2003; 42:118-24.