RESEARCH ARTICLES
Patients’, families’, and staff’s opinion on smoking within a psychiatric infirmary
Edson Arthur SchererI; Zeyne Alves Pires SchererII
IPsychiatrist. PhD in Experimental Pathology. Psychiatry Assistant of the Neuroscience and Behavioral Science Department of the Clinics’ Hospital of the Medicine College of Ribeirão Preto from University of São Paulo. Leader of the Group of Interdisciplinar Studies on Violence. Ribeirão Preto, São Paulo, Brazil. E-mail: eascherer@CHRP.fmrp.usp.br.ABSTRACT: Quantitative descriptive study carried out at the psychiatric ward of the Hospital das Clínicas de Ribeirão Preto, Brazil. It aimed at assessing patients’, families’, and team’s opinion concerning smoking during psychiatric hospitalization as well as smokers’ dependence. Semi-structured interview and Fagerström’s questionnaire were used. Ninety-eight (98) subjects were interviewed from July to December, 2010: 25 patients; 25 families; and 48 professionals. Patients showed higher degrees of tobacco dependence. The majority agrees to restricted smoking areas; to no-smoking requirements to all public places, with no exceptions to the mentally ill people; and to mandatory use of nicotine adhesive strips in the studied unit. The non-smoking ones complained about restriction-free smoking while in hospital and believed that cigarette smoking generated conflicts and disinterest in the therapeutic activities. Conclusions suggest that professionals must approach tobacco-related issues investing in research, prevention, and promotion of smoker’s health awareness in the treatment.
Keywords: Smoking; mentally ill persons; hospitalization; psychiatry.
INTRODUCTION
Smoking prevalence in mentally ill patients is higher than in the general population with higher levels of tolerance and dependence1-6. Smoking can give relief sensation from side effects of some medications and some symptoms of the disease4. The hopelessness sensation about the recovery and the need of control tend to take the patient to seek relief while smoking3. Difficulty in recognizing that smoking is an addiction, in perceiving medical complications and limited knowledge about the association between smoking and psychiatric disorders have made the impact of smoking in this population to be neglected3.5-7.
This study intent is to provide subsidies that facilitate a better oriented dialogue about smoking by mentally ill patients, especially in the hospitalization environment. It also seeks to be a basis to help health professionals in the implementation of programs of prevention and awareness of smokers on seeking treatment.
Therefore, the objective of this study was to know the opinion of hospitalized people, their families and members of the care team about the use of tobacco in the hospital environment and the degree of dependence of smokers’.
LITERATURE REVIEW
Research results of Israeli psychiatric hospitals showed high index of smokers in health professionals (48.1%) and in hospitalized patients (76.0%)8. A hospitalized person in these circumstances is extremely exposed to pro-smoke atmosphere and the consequences of smoke in his health.
Laziness, common in psychiatric institutions, makes the patient to smoke. The professionals have divergent opinions regarding cessation of smoking policy during hospitalization. Some of them argue that the mentally ill patient have a right to smoke even indoors. The cigarette can be used as bargaining, delivered to the patient as a reward to his good behavior3,4,7. Smoking can be seen as an instrument that appeases and facilitates social interaction of patients4,9. The team tends to believe that smoking bans increase patients’ aggressiveness6. The institution of treatments for nicotine dependence may suffer negative interference of smokers, patients and/or professionals, motivated by distrust in the efficacy of these therapies3.
The family of smokers with mental disorder may feel uncomfortable or show concern for this dependency. Swedish study with relatives of mentally ill patients10 performed after three years they had left the psychiatric hospital and moved to a sheltered home, showed that they coexist with sorrow, anguish and constant worry. They worry about grow-up children who spend time in bed, increasing weight, developing dental problems, smoking and drinking a lot of coffee.
METHODOLOGY
Descriptive and comparative research with quantitative approach11, performed in the Psychiatric Ward (PSYW) of the Clinics’ Hospital of the Medicine College of Ribeirão Preto from University of São Paulo (CHRP). In the period of July to December 2010, 98 subjects were interviewed and they signed the Free and Informed Consent Term. The total of the participants were all the 25 hospitalized patients, 25 representative of familiar or responsible of them and 48 team components (40 staff members and 8 trainee).
Patients could smoke in PSYW following determinations related to place and time. In June 2009, smoking was banned in CHRP, by the state Law No. 13,541/2009. To hospitalized smokers it is offered the nicotine patches as nicotine replacement therapy (NRT) to reduce discomfort, maximizing the effectiveness of anti-smoking policy and minimizing undesirable adrenergic effects of abstinence5.12.
Semi-structured interviews with issues for the characterization of participants, opinion about smoking and a question that selected smokers who answered the Fagerström questionnaire (assessing the degree of tobacco dependence)13 was used. Subjects were interviewed in a private room and combined schedules without compromising their activities.
The findings were compiled in a database in Excel software and compiled by the Statistical Package for Social Sciences(SPSS) version 18. The results are presented in a descriptive way, complemented with excerpts from responses showing the subjects' opinions.
The study was approved by the Ethics Committee of the CHRP (CHRP process Number 3504/2009). In the results, to ensure anonymity, the subjects were identified by letters representing each respondent group: P (patient), F (family), T (team); followed by the identification number of each one in his group.
RESULTS
Data were submitted to descriptive analysis and to verify the desired associations, the Fisher exact test was proposed. No significant associations were found. The small sample size was a limitation of the study. The severity condition of the people hospitalized in PSYW tends to prolong the time of hospitalization. In 2010, the average time of stay was 87 days with bed occupancy rate of 75%.
The group of 25 patients was 16 to 78 years old (average: 42.4, median: 36). Family members were 23 to 69 years old (average: 50.2, median: 51). The 40 team members were 24 to 57 years old (average: 38.5, median: 36.5). The 8 trainees were 24 to 29 years old (average: 26.2, median: 26). From the 98 subjects, 58 (59.2%) were female; 47 (47.9%) married or with consensual marriage and 42 (42.8%) single; and 70 (71%) were Catholics. Patients and their families had less education than professionals and had occupations related to this limitation.
The prevalent diagnoses were mood disorder and schizophrenia, with 11 (44%) and 7 (28%) patients respectively. The time of disease, of the current hospitalization and number of hospitalizations were: 13 (52%) with 10 or more years of evolution, 8 (32%) with 1 to 9 years and 4 (16%) less than a year; the time of hospitalization ranged from 3 to 240 days (average: 46.3, median: 30); and 16 (64%) with a history of one to five hospitalizations and nine (36%) had 6 or more.
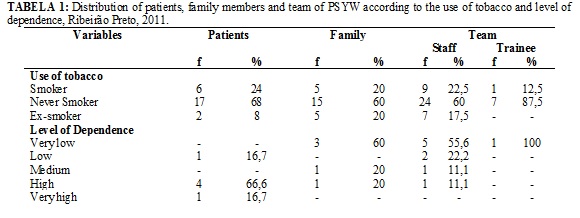
From the 98 subjects, 21 (21.4%) were smokers, 14 (14.3%) were ex-smokers and 63 (64.3%) never smokers, as shown in Table 1. Regarding the sex of the smokers, 14 (66.7%) were women and 7 (33.3%) men. From women, 5 (35.7%) were staff members, 4 (28.6%) patients, 4 (28.6%) family and 1 (7.1%) was a trainee. From men, 4 (57.1%) were team members, 2 (28.6%) patients and 1 (14.3%) was family.
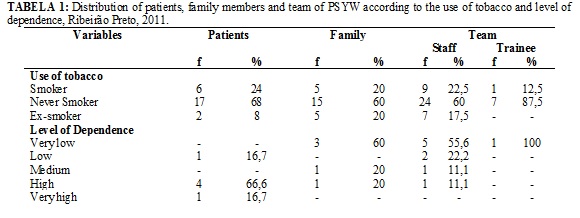
In regard to the level of tobacco dependence we found: 5 (83.4%) of patients with high or very high level; 4 (80%) family members with very low or medium level; and 9 (90%) of the team members with very low, low or medium levels, as shown in Table 1.
In the opinion of 87 (88.8%) of respondents, specific areas should be reserved for smokers. They agreed with smoking banning in places where there is concentration of people such as: airports - 18 (85.7%) of smokers and 58 (92.1%) of non-smokers; churches - 18 (85.7%) of smokers and 58 (92.1%) of non-smokers; public transport - 18 (85.7%) of smokers and 59 (93.7%) of non-smokers; shopping centers - 17 (81%) of smokers and 58 (92.1%) of non-smokers; and hospitals - 17 (81%) of smokers and 59 (93.7%) of non-smokers.
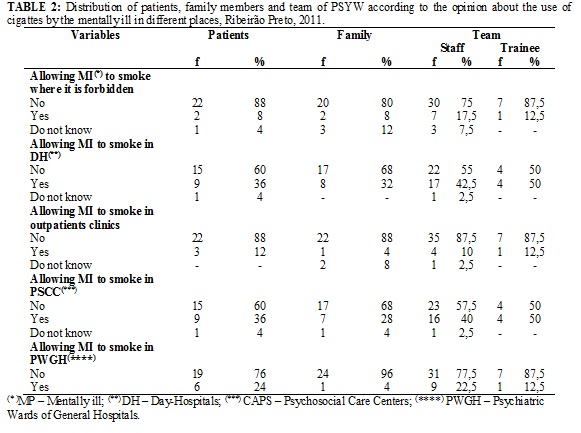
From the total subjects studied, 79 (80.6%), of whom 14 (66.6%) smokers and 65 (84.4%) non-smokers, agreed not to allow mental patients to smoke in public places where it is forbidden, according to Table 2.
The following excerpts exemplify the justifications.
It is part of treatment be without cigarettes. (P25)
Forbidden means forbidden for everyone, no exceptions. (F18)
The psychiatry patient is unable to control the use, he abuses. (T32)
Rule is to be followed. We should not treat the mental patient differently. (T48)
The 12 (12.2%) subjects, 5 (23.8%) smokers and 7 (9%) non-smokers, favorable to release mentally ill to smoke where it is prohibited, according to Table 2, presented the justifications below.
Each one does what he wants. (P6)
The cigarette relieves anxiety. (P21)
We have to separate those who smoke. Mentally ill patients sometimes do not understand rules. (F11)
The mentally ill smoke on impulse or for lack of what to do, it is not dependence. (T23)
If ban, we have risk of aggression, agitation and anxiety. (T10)
About the releasing smoking for mentally ill in specialized care services, most were against: outpatients clinics 86 (87.8%), psychiatric wards of General Hospitals (PWGH) 81 (82.7%), psychosocial care centers (PSCC) 59 (60.2%) and day hospitals (DH) 58 (59.2%), as shown in Table 2. Most non-smokers agreed to not allow patients’ smoke in: DH 50 (64.9%), PSCC 52 (67.5%), outpatients clinics 68 (88.3%) and PWGH 67 (87%). Among smokers, while 18 (85.7%) would not release patients to smoke in outpatient clinics and 14 (66.7%) in wards, 13 (61.9%) would allow smoking in DH and PSCC, as shown in Table 2.
Asked whether they found any difficulties or felt any discomfort due to smoke by patients in PSYW when was allowed to smoke, 66 (67.3%) of respondents, 5 (23.8%) smokers and 61 (79.2%) non-smokers, responded affirmatively. In the following excerpts, the justifications presented.
Because it is very bad, the smell bothers. (P9)
I have smoke allergy. (F9)
I feel headache, nausea. (F20)
Smoking is another stressor. When they could smoke, insisted all the time, it was difficult to control and to follow the routine. (T21)
Smoking was their main activity, diverting the interest of service’s activities. (T31)
The arguments of the 31 (31.6%) subjects, 16 (76.2%) of whom smokers and 15 (19.5%) non-smokers who reported no discomfort with smoke in PSYW, when it was allowed, were:
No, because I smoke and I am used to the smell. (P21)
As a smoker, I do not care about the smell. (F5)
No, because I'm a smoker and they smoked at the given place. (T17)
When asked if they would agreed with banning patients’ smoking in PSYW, the majority, 62 (63.3%), 8 (38%) smokers and 54 (70.1%) non-smokers answered affirmatively.
Non-smoker receives the greatest burden. (P12)
The hospitalization is a good time to remove the cigarette. (F6)
Yes, because patients accepted well. Before the law I would answer no, because I believed that they would have much resistance in not smoking. (T18)
The arguments of the 31 (31.6%) respondents, 11 (52.4%) smokers and 20 (25.9%) non-smokers, contrary to prohibit smoking in PSYW are shown below.
The smoker gets more nervous if he does not smoke. (P2)
Who is addicted do not stop, gets worse for his head. (F18)
It is not in 2 or 3 months he can stop. (T10)
The decision should be personal. (T14)
The majority, 81 (82.7%), 15 (71.4%) of which smokers and 66 (85.7%) non-smokers, agreed with the conduct of offering the use of nicotine patches (NRT) to smokers hospitalized in PSYW as smoking ban policy.
I'm using it, I don’t feel like smoking. (P7)
Nobody wants to be near the smoker. (F13)
With the adhesive shall not affect the non-smoker. (F15)
Since that you have the patient’s consent. (T1)
The use reduces abstinence symptoms. (T43)
The 10 (10.2%) participants, 3 (14.3%) smokers and 7 (9%) non-smokers, who did not agree with NRT with nicotine patch presented justifications as:
I believe that the adhesive doesn’t work, doesn’t solve. (P2)
I think it doesn’t solve, it would be better a medicine that disgusts. (F11)
I know the patch, know that it doesn’t work. (T14)
DISCUSSION
Findings of the Surveillance System of Protection and Risk Factors for Chronic no Transmitted Diseases by Telephone Survey (VIGITEL), implemented by the Ministry of Health in Brazil, indicated a percentage of 12.1% of smokers in Brazil in 201214. In this study the smokers quota was 98 (21.4%) subjects, result greater than that of the previous study. With regard to sex, the population research concluded that this habit was more disseminated among men (15.5%) than among women (9.2%). In this research there was a predominance of female smokers (66.7%).
The literature shows that hospitalized patients tend to have higher prevalence rates of smoking1,15. Research in a university General Hospital of São Paulo, identified 58 (21%) smokers, of the total of 275 patients, in different hospitalization units16. Studies in psychiatric inpatient services showed higher rates. In Spain were found 21 (52%) smokers among 40 hospitalized in PWGH17. In Porto Alegre, from 103 patients of a PWGH, 48 (46.6%) were smokers18. In the present findings, 6 (24%) of the 25 patients were smokers, a result close to that of the São Paulo study. The observed differences between our study and others may be related to samples’ size and to factors such as cultural differences of the sites surveyed.
For most smokers patients (83.3%) the tobacco addiction assessment (Fagerström’s questionnaire) was considered high (score ≥ 6). Family members and professionals, mostly (80% and 90%, respectively) have showed medium to low levels of dependence (score ≤ 5). This finding corroborates literature data that suggests that psychiatric patients exhibit more intense dependence4,17,18.
The opinion of the respondents about smoking in different environments is comparable to results from the literature. In relation to smoking in public places, the present findings (88.8%) were similar to those of surveys conducted in Italy and Ireland, where, respectively, 90.0% and 83.0% of the population were in favor of public areas free of tobacco19.20. Despite agreeing with smoking bans in places where there are people concentration, the responses of smokers were in smaller percentages. The smokers tend to disagree with rules that interfere with their right to smoke in enclosed public places such as hospitals and other health services21.
Most respondents agreed with not allowing mental patients to smoke in public places where it is prohibited. They justified with the knowledge about the dangers of cigarette, the injury to treatment, the nuisance and disrespect with the non-smokers. They believe that mentally ill have difficulty in controlling the use of cigarettes and allowing them to smoke could stimulate stigma against the disease. Smoking causes damage to physical and psychological integrity of the individual. Nicotine is dependence inductor and individual, social and environmental factors are important for the development of this addition22,23. Literature review article on schizophrenia and tobacco dependence concluded that smoking might interfere with drug therapy, worsen the symptoms, increasing the number of psychotic episodes, precipitating tardive dyskinesia and increase vulnerability to chronic diseases4.
On the other hand, those who are favorable that the mentally ill smoke in public places used as arguments the patient's free will, their difficulty in understanding and following rules and the notion that smoking relieves anxiety. They believe that the patient smokes not for dependence but for impulse and idleness, and in prohibition case, he has risk of getting agitated and aggressive. Smoking can function as an emotional buffer. Smokers tend to believe that smoking can control their anxiety, anger and sadness4.22. Smoking contributes to the development of anxiety disorders as consequence of the presumed anxiogenic effects of nicotine and its cessation is followed by reduction of anxiety after 4 weeks of abstinence24. Research with schizophrenic chronic smokers patients’ hospitalized undergoing behavioral group’s orientation approach to reduce smoke showed a decreased number of cigarettes used without worsening of symptoms or behaviors of patients1. The right to smoke was not addressed in our study for being controversial and getting away from objectives.
The issue concerning the release of patients to smoke in care services showed divergent results. The different opinions regarding outpatient clinics, DH and PSCC can be explained by the fact that patients stay for shorter period in them. Moreover, the larger and open physical space of DH and PSCC allow having areas for smoking. Allowing smoking in DH and PSCC can be backed in a study conducted on a PSCC-ad (alcohol and drugs PSCC), in which patients, before attending treatment, did not consider cigarette as a drug25. They believed that they could smoke and that smoking does not cause damage to health, which is corroborated in a study on the perception of the risks of smoking among smokers with and without schizophrenia, where patients tended to less emphasize the dangers of smoking26. There were also found differences of opinion with respect to the prohibition of smoking in PWGH and PSYW. What can justify these differences is that the PSYW had certain, until the implementation of the anti-smoking law, patients’ pro-smoking culture.
In favor of banning smoking in PSYW, patients and family members mentioned the harm of cigarette to smokers and non-smokers and that this ban may encourage smoking cessation. Professionals showed surprise at the favorable reactions of patients and families with the change after anti-smoking law. In the practice of this study PSYW, while professionals and supervisors of students and trainees perceived concern of colleagues with smoke. They recognized that interfered with response to treatment and patients relationships. They mentioned relief at no longer need to manage patients’ cigarettes. Before they took care of obtain, distribution, control and observation of the patient while smoking to prevent complications such as the risk of burning objects or unit furniture. So now, they no longer need to divert part of their time to care for patients to manage their smoking5.
Those against smoking prohibition in the PSYW mentioned the difficulty of dependent to be without smoking and the effects of the ban on his emotional state. They considered time in hospitalization insufficient to change the habit and that the will to stop ought to be from the smoker. However, one study found that schizophrenics are more likely to quit smoking in response to social pressure or some reward26. Hospitalization’s moment is conducive to offer patients guidance about the benefits of smoking cessation. Moreover, the insertion of oriented treatment programs to decrease smoking does not cause deterioration by reducing the use of cigarettes1.
Most non-smokers reported difficulties or uncomfortable when smoking was allowed in PSYW as: passive smoking; tolerance of conviviality; cigarette’s smell; tobacco’s allergy; nausea, headache, nasal and eye irritation. They believed that smoking was a cause of quarrels and stress generator to patients, making difficult the control and the routines’ maintenance. They realized that smoking might be cause to divert the interest of the patient for therapeutic activities. Most smokers denied any difficulty or discomfort and suggested to reserve a smoking area in the ward.
Most participants agreed with the PSYW’s conduct of using NRT. They mentioned the positive effects of the adhesive and the improvement in the inclusion of patients in the group. They had stand out the need for their use to be with the consent of the smoker. Among the justifications of the 10 (10.2%) participants against the use of NRT were found the disbelief in its efectiveness3 and discomfort with this conduct.
To know the association between smoking and mental illness is necessary to plan strategies to combat smoking in this population. Recognizing the stigma and their own opinions about the mentally ill smokers facilitates the approach of professionals. Interventions should offer to patients the opportunity to reflect on smoking in their life and their willingness to stop4. In the present study, it was perceived the lack of knowledge of professionals about mentally ill smokers, consistent with the literature3-7. There are studies on the neurobiological aspects related to cigarettes, but few address the therapeutic interventions and their implications, especially in Brazil. Researches has also shown that people have knowledge about the effects of smoking on health and show openness to discussions on the topic, but have low recognition of the content of educational campaigns27.28. Therefore, it is necessary to invest in researches on prevention and health promotion that address the issue of smoking.
CONCLUSION
The mentally ill smokers showed higher levels of tobacco dependence as found in the literature. The pinion of most subjects was favorable to prohibit mentally ill to smoke in treatment settings and in public places. They agreed with the reserve of areas for smoking and the use of NRT in PSYW. The non-smokers reported uncomfortable when smoking was allowed in the hospitalization and believed that cigarettes generated conflicts and lack of interest in therapeutic activities. These findings may support discussions on smoking and mental illness and assist in programming interventions aimed at the cessation of smoking in this people.
Despite the limited sample, which does not allow generalization of the findings, the proposed objectives were achieved, because the issue of smoking among the mentally ill patients was analyzed.
To provide an environment free of tobacco in health services may be the beginning of a therapeutic process to encourage smoking cessation. Therefore, it is necessary that professionals have knowledge about the relationship between smoking and mental illness. However, it seems to be little knowledge about this relationship. It is expected that professionals address the issue of smoking in its entirety, investing in research, prevention and health promotion, educating smokers to seek anti-smoking treatment.
REFERENCES
1. Gelkopf M, Noam S, Rudinski D, Lerner A, Behrbalk P, Bleich A, Melamed Y. Nonmedication smoking reduction program for inpatients with chronic schizophrenia: a randomized control design study. J Nerv Ment Dis. 2012;200:142-6.
2. Kreinin A, Novitski D, Rabinowitz D, Weizman A, Grinshpoon A. Association between tobacco smoking and bipolar affective disorder: clinical, epidemiological, cross-sectional, retrospective study in outpatients. Compr Psychiatry. 2012;53:269-74.
3. Lawn S, Pols R. Smoking bans in psychiatric inpatient settings? A review of the research. Aust N Z J Psychiatry. 2005;39:866–85.
4. Oliveira RM, Furegato ARF. Esquizofrenia e dependência de tabaco: uma revisão integrativa. Enferm Glob. 2012;25:404-25.
5. Prochaska JJ, Gill P, Hall SM. Treatment of tobacco use in an inpatient psychiatric setting. Psychiatr Serv. 2004;55:1265–70.
6. Reilly P, Murphy L, Alderton D. Challenging the smoking culture within a mental health service supportively. Int J Ment Health Nurs. 2006;15:272–8.
7. Perondi AML, Colombo M, Rondina RC. O impacto da internação em hospital psiquiátrico no comportamento do fumante de tabaco: algumas considerações. Revista Cient Eletr de Psicol. [periódico na internet]. 2006 [citado em 25 julho 2013];IV(6):[11 screens]. Available at: http://faef.revista.inf.br/site/e/psicologia-6-edicao-maio-de-2006.html#tab448
8. Willemsen MC, Görts CA, Van Soelen P, Jonkers R, Hilberink SR. Exposure to environmental tobacco smoke (ETS) and determinants of support for complete smoking bans in psychiatric settings. Tob Control. 2004;13:180–5.
9. Lawn S. Cigarette smoking in psychiatric settings: occupational health, safety, welfare and legal concerns. Aust N Z J Psychiatry. 2005;39:886–91.
10. Pejlert A. Being a parent of an adult son or daughter with severe mental illness receiving professional care: parents’ narratives. Health Soc Care Community. 2001;9:194–204.
11.Triviños ANS. Introdução à pesquisa em ciências sociais: a pesquisa qualitativa em educação. São Paulo: Atlas, 2010.
12. Focchi GR, Braun IM. Tratamento farmacológico do tabagismo. Rev psiq clín. 2005;32:259-66.
13. Meneses-Gaya IC, Zuardi AW, Loureiro SR, Crippa JAS. As propriedades psicométricas do teste de Fagerström para dependência de nicotina. J bras pneumol. 2009;35:73-82.
14. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Departamento de Vigilância de Doenças e Agravos não Transmissíveis e Promoção de Saúde. Vigitel Brasil 2012: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico/Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Vigilância de Doenças e Agravos não Transmissíveis e Promoção de Saúde. – Brasília: Ministério da Saúde, 2013.
15. Willaing I, Jørgensen T, Iversen L. How does individual smoking behaviour among hospital staff influence their knowledge of the health consequences of smoking? Scand J Public Health. 2003;31:149–55.
16. Figlie NB, Pillon SC, Dunn J, Laranjeira R. The frequency of smoking and problem drinking among general hospital inpatients in Brazil - using the AUDIT and Fagerström questionnaires. Sao Paulo Med J. 2000;118:139-43.
17. García CI, Villa MJA, Quirós JCB, Suárez EB, Gonzalo JC, Del Valle RG, et al. Modificación del patrón de consumo de tabaco en una unidad de psiquiatría de hospital general. Nure Inv [periódico na internet]. 2009 [citado em 22 jun 2013];6(38): [7 screens]. Available at: http://www.fuden.es/FICHEROS_ADMINISTRADOR/ORIGINAL/modpat_original_38.pdf
18. De Boni R, Pechansky F. Prevalência de tabagismo em uma unidade de internação psiquiátrica de Porto Alegre. Rev psiquiatr Rio Gd Sul. 2003;25:475-8.
19. Fong GT, Hyland A, Borland R, Hammond D, Hastings G, Mcneill A, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: Findings from the ITC Ireland/UK Survey. Tob Control. 2006;15 Suppl 3: 51-8.
20. Gallus S, Zuccaro P, Colombo P, Apolone G, Pacifici R, Garattini S, et al. Effects of new smoking regulations in Italy. Ann Oncol. 2006;17: 346-7.
21. Gokirmak M, Ozturk O, Bircan A, Akkaya A. The attitude toward tobacco dependence and barriers to discussing smoking cessation: a survey among Turkish general practitioners. Int J Public Health. 2010; 55:177–83.
22. Consuegra RVG, Zago MMF. Creencias en fumadores pertenecientes a un programa de salud cardiovascular. Rev Latino-Am Enfermagem. 2004;12:412-9.
23. Sawicki WC, Rolim MA. Graduandos de enfermagem e sua relação com o tabagismo. Rev esc enferm USP. 2004; 38: 181-9.
24. Johnson JG, Cohen P, Pine DS, Klein DF, Kasen S, Brook JS. Association between cigarette smoking and anxiety disorders during adolescence and early adulthood.JAMA. 2000;284:2348-51.
25. Vieira JKS, Carvalho RN, Azevedo EB, Silva PMC, Ferreira Filha MO. Concepção sobre drogas: relatos dos usuários do CAPS-ad, de Campina Grande, PB. SMAD, Rev Eletr Saúde Mental Álcool Drog [internet]. 2010 [citado em: 4 fev 2014]; 6:274-95. Available at: http://www2.eerp.usp.br/resmad/artigos/SMADv6n2a4.pdf
26. Kelly DL, Raley HG, Lo S, Wright K, Liu F, McMahon RP, Moolchan ET, Feldman S, Richardson CM, Wehring HJ, Heishman SJ. Perception of smoking risks and motivation to quit among nontreatment-seeking smokers with and without schizophrenia. Schizophr Bull. 2012;38:543–51.
27. David HMSL, Matos HS, Silva TS, Dias MG. Tabagismo e saúde da mulher: uma discussão sobre as campanhas de controle do tabaco. Rev enferm UERJ. 2006;14:412-7.
28. Lopes GT, Belchior PC, Felipe ICV, Bernardes MM, Casanova EG, Pinheiro APL. Dinâmicas de criatividade e sensibilidade na abordagem de álcool e fumo com adolescentes. Rev enferm UERJ. 2012;20:33-8.