RESEARCH ARTICLES
Pressure ulcer risk assessment and preventive nursing care in the intensive care unit
Taís Pagliuco BarbosaI; Lúcia Marinilza BeccariaII; Nádia Antônia Aparecida PolettiIII
IIntensive Care Unit Nurse, Base Hospital – Faculty of Medicine of São José do Rio Preto. São Paulo, Brazil. Email: tais.pagliuco@hotmail.comABSTRACT: This is a cross-sectional, prospective study with the aim to identify patients at risk for developing pressure ulcers (PU) in the intensive care unit (ICU), by means of Braden Scale scores and to relate these scores to the nursing care delivered toward ulcer prevention. The study was carried out in three adult intensive care units from July to December 2010, with risk classification (low, moderate and high) and evaluation of the patient care through systematic observation of 190 patients/beds. There was a prevalence of patients with moderate risk and a mean age of 54.35 years. The relationship between risk assessment and preventive measures was not consistent with the scores found. The procedures that were less frequently observed were changing the position or posture of a patient and the use of pads. In conclusion, the Braden Scale is necessary and must support the nursing care in the prevention of pressure ulcers in the ICU.
Keywords: Pressure ulcer; care; nursing; intensive care unit.
INTRODUCTION
Pressure ulcers (PUs) are considered a serious health problem, representing a constant challenge for patients, professionals and institutions, both due to its high incidence and prevalence in certain populations, as well as to the consequences generated in relation to increased morbidity and mortality, in addition to the costs generated1. It is defined by the National Pressure Ulcer Advisory Panel (NPUAP) as a localized area of necrotic tissue that tends to develop when tissue is compressed between a bony prominence and an external surface for a prolonged period of time, being observed in four stages of development2.
The essence of the nursing care is not exclusively related to the environment or equipment, but to the decision-making process, based on the understanding of the physiological and psychological conditions of the patient3. In the intensive care units (ICU), patients are at high risk of developing PUs because they are considered critical, with instability and a risk of failure of one or more physiological systems4. They have serious medical conditions or need for more rigorous and frequent controls, associated with the increased complexity of the treatment, whether invasive or not.
Due to mechanical restrictions or pathological situations, such as paralysis, coma, pain, trauma and sedation, they have deficits in mobility that restrict them to bed, requiring constant care in the search for maintaining the integrity of the skin and underlying tissues5,6.
Given the aforementioned, the objective of this study was to identify patients at risk of developing pressure ulcers in the ICU, by using the Braden Scale and reporting on preventive measures carried out by the nursing staff.
LITERATURE REVIEW
Risk assessment for PU in critically ill patients is the first step of the prevention program, as it assists the nurses in identifying risks and establishing adequate preventive measures7.
Among the various methods for evaluating the risk of PU, the Braden Scale is the most widely used, having been subjected to several studies and reliability and validity tests in different populations8. It is composed of six sub-scales that assess the degree of sensory perception, humidity, physical activity, nutrition, mobility, friction and shear. All sub-scales are graded from 1-4, except for friction and shear, which vary from 1-3. The total score ranges from 6-23, with scores from 19-23 indicating patients without risk, 15-18 low risk, 13-14 moderate risk, 10-12 high risk and equal to or less than 9, very high risk9.
PUs are considered one of the major challenges to be faced in the complex care at ICUs, since they correspond to a complication, or even an iatrogenic injury, as they eventually become common in patients with short- or long-term hospitalization10. They elevate therapeutic costs, increase the workload of the care staff, increasing the need for human and material resources as well as the use of expensive equipment to solve the problem, also representing an increase in the physical and emotional suffering of the patients and their families11.
The relationship between the identification of patients hospitalized in the ICU at risk of developing PU, together with its prevention, is the focus of this study. Attention to these aspects can collaborate with care to prevent injury to patients12.
METHODOLOGY
A cross-sectional, prospective study was conducted in a special-sized teaching hospital, with 780 beds, located in São José do Rio Preto, interior of the state of São Paulo, in three ICUs, namely: general care, health insurance plans, and emergency care, called ICU A, B and C, respectively. The total number of beds in these units is 63, used for the treatment of medical and surgical patients from the age of 13 years and up, of both genders. The shift of the daytime nursing staff is 6 hours, and 12 hours for the night shift.
ICU A is subdivided into a surgical unit, with 10 beds, where patients are admitted for intensive care arising from postoperative major surgery or with complications, and a clinical unit encompassing 13 beds, where patients are admitted with diagnoses related to neuropathology, gastrointestinal pathology, and polytrauma patients, among others. ICU B has 20 beds divided into an advanced hemodynamic support unit, a metabolic unit, a neurological and isolation unit; and ICU C is comprised of 20 beds, including both medical and surgical patients.
The study population consisted of all patients admitted to the ICUs, who were evaluated by means of the Braden Scale, completed daily by the nurses in each sector. A total of 190 patients/beds were observed, from July to December 2010. Exclusion criteria were patients not registered with the Braden Scale file due to discharge, death or those who had already developed PU.
A checklist was also used as a tool for data collection, completed by the researchers, three times a week, alternating shifts between morning, afternoon and night, through observation and checking at the bedside for good care practices in relation to PU prevention measures, such as: clean bed, clean and dry patient, changing positions, pyramidal mattress, use of cushions and skin hydration.
The research proposal was submitted to the Research Ethics Committee of the Faculty of Medicine of São José do Rio Preto, under protocol no. 3586/2009 and approved according to opinion no. 303/2009.
The results obtained were analyzed using descriptive statistics (frequency calculations, arithmetic mean, median, extreme standard deviation and confidence interval), by means of the Mann-Whitney Test, the Kruskal-Wallis Test and Dunn multiple comparison, as well as Pearson’s Correlation Coefficient Test.
RESULTS AND DISCUSSION
During the study period, 190 patients/beds were observed and good practices checked in three ICUs of the institution that possessed the classification of risk for development of PUs. The mean age found was 54.35 years ± 16.02, with a median of 57 years of age, minimum of 18 and maximum of 91, 107 (56.32%) were male.
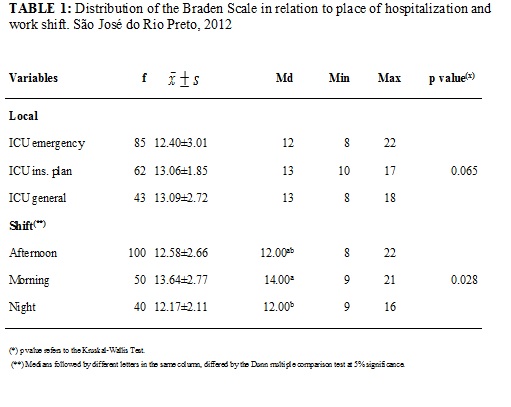
Most patients (56.32%) had polytrauma, pneumonia or neurological problems. Regarding the place of hospitalization, 85 (44.74%) were admitted to the emergency ICU; 62 (32.63%) to the health insurance plan ICU and 43 (22.63%) to the general ICU. Observations and verifications were carried out as follows: 50 (26.32%) in the morning, 100 (52.63%) in the afternoon and 40 (21.05%) during the night. See Table 1.
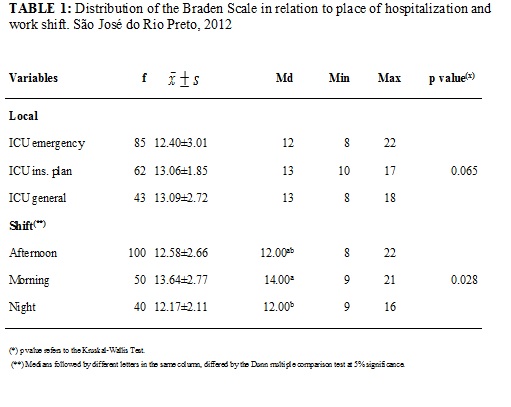
As regards preventive measures associated with good healthcare practices, 179 (94.21%) beds were clean and 178 (93.68%) patients were clean and dry. Furthermore, 78 (41.05%) had their position changed every 2 hours, and, in 153 (80.53%) the pyramidal mattress was used. The use of cushions was observed only in 58 (30.53%), whereas skin hydration was performed in 124 (65.26%). See Table 2.
There were no statistically significant differences between the scores of the Braden Scale when compared with the place of patient hospitalization, since the p value found (p=0.065) was higher than the significance level of the test (p=0.05).
It was observed that there are significant differences between the scores of the Braden Scale when compared to the work shift, since the p value (p=0.028) was less than 0.05. The Dunn multiple comparison test showed discrepancy between the morning and the night shifts, where the night shift had lower scores, indicating greater risk for developing PU when compared to the morning shift.
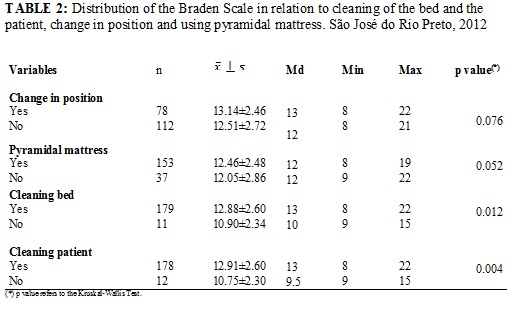
Patients who did not have their beds sanitized (5.79%), had lower scores (10) in the Braden Scale, compared with those who did (13). The p value (p=0.012) was below the significance level for the test. This fact shows that cleaning the bed is a factor that influences the increased risk in the development of PU. The hygiene of the patient is also essential for reducing the risk, since the p value (p=0.004) was less than 0.05.
The data obtained showed no significant differences in the Braden Scale scores in relation to changing position, since the p value (p=0.076) was higher than the level of significance for the test. Despite presenting no discrepancies, patients undergoing a change in position every 2 hours (41.05%) had higher scores (13) in relation to those who did not undergo this change (12). Regarding the use of the pyramidal mattress, there was no significant difference in scores of the patients who used them or not, since the mean score was 12, which represents a moderate risk. See Table 3.
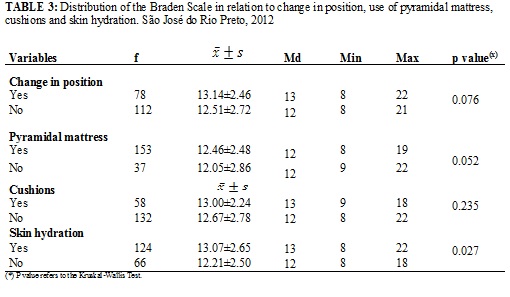
Regarding the Braden Scale scores, when compared to the use of cushions, there was no significant evidence between the patients who used them and those who did not use cushions on bony prominences, since the p value (p=0.235) was higher than the level of significance (p=0.05). However, patients who did not use cushions showed lower scores (12), increasing the risk of developing PU.
Hydration of the patient's skin is a preventive measure to be employed so that the risk of developing PU is minimized, since patients undergoing hydration showed higher scores (13) than those who did not (12). The p value obtained regarding the comparison test was 0.027, less than the value of significance (p=0.05).
Most patients were male (56.32%), confirming the findings of a study in a public hospital in São Paulo that characterized the profile of patients at risk of developing PU, most of whom were also male (57.7%)13. On the other hand, a study on the risk factors for developing PU in institutionalized older patients found a predominance of female patients (62.8%); although the incidence rate was higher among men. Despite the differences, there was no relationship found between gender and the development of PU14.
The age of patients ranged from 18 to 91, with a mean of 57 years of age. In the age group of 60 years or older, there was an increased risk, consistent with the literature, which indicates a higher rate of incidence of PU in this age group13. This is considered a risk factor, because the skin of older adults undergoes several changes, such as atrophy of the dermis and decreased barrier function, which increases the risk of injury, reducing the capacity of sensory receptors, thus making the perception of traumatic stimuli more difficult. It also becomes drier due to decreased activity of the sebaceous glands, with decreased tissue vascularity occurring. Because of these changes, older adults are more vulnerable to mechanical trauma and the development of PU14.
Most patients (56.32%) had a diagnosis of polytrauma, pneumonia or neurological problems. Considering the case severity, every person admitted to the ICU had the risk of developing PU due to changes in level of consciousness, immobility, nutritional state and their actual general state of health itself, as well as other factors15.
Comparing the preventive measures related to good healthcare practices, 94.21% had clean beds and 93.68% were clean and dry. As for changing positions, only 41.05% of patients underwent this care and 80.53% had a pyramidal mattress. As for the use of cushions on bony prominences, only 30.53% used these and 65.26% had their skin hydrated.
In a pilot study, researchers also compared the quality of care in patients at risk of developing PU, with the participation of 25 hospitals in five European countries, to identify whether interventions aimed at preventing PU was appropriate, and it was found that about 20% of patients at “low risk” did not receive a pyramidal mattress for pressure redistribution, about 70% did not have the use of cushions for pressure relief and more than 60% were not repositioned regularly by the nursing staff. Moreover, those who were not at risk received pressure redistributing mattresses, made use of cushions and were repositioned regularly. The authors stressed that preventive measures used in patients without risk represent an unnecessary expense and should be used on those who really need it16.
In another study, there was a failure in the execution of some preventive measures, such as: errors in the documentation of medical records on risk assessment and reassessments, lack of standardization of schedules for repositioning the patient and they emphasized that this result is probably related to a lack of knowledge on the subject. The authors concluded that nurses in the study did not promote efficient care for the prevention of PU and they highlighted that nursing care in hospitals is considered the singular most important factor for its prevention5.
Corroborating this thought, other researchers reported that the Braden Scale allows for the standardization of assessment and the documentation of risk for PU, with common language and, therefore, it must be shared by professionals for the identification of risk factors and, consequently, for the prescription of preventive measures17.
The correct use of the Braden Scale reduces the variation of risk assessment among nurses, however, initial and then periodic training with nursing professionals is necessary, aiming to avoid and correct differences, errors and disagreements in the choice of scores. Therefore, it is necessary that nurses have a clear understanding of the meaning of the descriptions of sub-scales8.
In this context, it is worth emphasizing the importance of nursing care being embedded in clinical guidelines, in protocols of prevention, based on the risk level of each patient, so that the preventive measures used are appropriate and effective18. Nursing professionals should be aware of these aspects, so that there is an improvement in care, thus avoiding unnecessary spending19. Therefore, the use of the Braden Scale by nurses should support nursing care in preventing PU.
CONCLUSION
The identification of patients at risk of developing PU was elevated in the three studied ICUs, showing that nursing professionals performed some of the care procedures more frequently, such as cleaning the bed and the patient, using a pyramidal mattress and skin hydration; whereas others were less observed, such as the change of position and the use of cushions on bony prominences, and differences between work shifts, with night shifts being revealed as having greater risk for developing PU, when compared to the morning shift.
One limitation of the study was the use of the Braden Scale for several nurses in the ICUs, understanding that each professional interprets the items and marks the scores according to their knowledge and routine of their work unit. Another important shortcoming was the lack of information on nursing prescriptions as regards prohibiting the change in position of some patients and specific situations.
In relation to preventive measures, the treatment was not performed in accordance with the classification of the Braden Scale, i.e., the nursing prescription contained similar actions, regardless of the risk presented by the patient (low, moderate and high). In conclusion, the use of the Braden Scale is necessary, and must be shared by nurses in different work shifts to support the nursing prescription in the prevention of PU in the ICU.
BIBLIOGRAPHY
1.Vangilder C, Macfarlane GD, Meyer S. Results of nine international pressure ulcer prevalence surveys: 1989 to 2005. Ostomy Wound Manage, 2008; 54 (2): 40-54.
2. National Pressure Ulcer Advsory Panel. Pressure ulcer definition and stages. USA:NPUAP; 2007.
3. Ciampone JT, Gonçalves LA, Maia FOM, Padilha, KG. Necessidades de cuidado de enfermagem e intervenções terapêuticas em unidade de terapia intensiva: estudo comparativo entre pacientes idosos e não idosos. Acta Paul Enferm. 2006; 19: 28-35.
4. Ozdemir H, Karadag A. Prevention of pressure ulcers: a descriptive study in 3 intensive care units in Turkey. J. Wound Ostomy Continence Nurs. 2008; 35 : 293-300.
5. Kottner J, Dassen T. An interrater reability study of the Braden Scale in two nursing homes. Int J Nurs Stud. 2008; 45: 1501-11.
6. Magnan MA, Maklebust J. The effect of web-based Braden Scale training on the reliability and precision of Braden Scale pressure ulcer risk assessments. J Wound Ostomy Continence Nurs. 2008; 35:199-208.
7. Ayello EA, Lyder CH. A new era of pressure ulcer countability in acute care. Adv Skin Wound Care. 2008; 21 (3): 134-40.
8. Araújo CRD, Lucena STM, Santos IBC, Soares MJGO. A enfermagem e a utilização da Escala de Braden em úlcera por pressão. Rev enferm UERJ. 2010; 18:359-64.
9. Braden BJ, Maklebust J. Preventing pressure ulcers with the Braden scale. Am J Nurs. 2005; 105 (6): 70-2.
10. Araújo TM, Moreira MP, Caetano JA. Avaliação de risco de úlcera por pressão em paciente críticos. Rev enferm UERJ. 2011. 19:58-63.
11. Cavalcante CS, Araújo TM, Araújo MFM, Junior GMB, Caetano JA. Acurácia de duas escalas de avaliação de risco para úlcera por pressão em pacientes críticos. Rev enferm UERJ. 2011; 19:381-5.
12. Alves N, Deana NF. O açúcar refinado no tratamento da infecção por pseudomonas sp em úlcera por pressão. Rev enferm UERJ. 2009; 17: 194-7.
13. Blanes L, Duarte IS, Calil JA, Ferreira LM. Avaliação clínica e epidemiológica das úlceras por pressão em pacientes internados no Hospital São Paulo. Rev Assoc Med Brás. 2004; 50: 182-7.
14. Souza DMS, Santos VLCG. Fatores de risco para o desenvolvimento de úlceras por pressão em idosos institucionalizados. Rev Latino-Am Enferm. 2007; 15:71-9.
15. Shahin ESM, Dassen T, Halfens RJG. Pressure ulcer prevalence and incidence in intensive care patients: a literature review. Nurs Crit Care. 2008; 13:71-8.
16. Vanderwee K, Clark M, Dealey C, Gunningberg L, Defloor T. Pressure ulcer prevalence in Europe: a pilot study. J Evaluation Clin Practice. 2007; 13:227-35.
17. Brown SJ. The Braden Scale: a review of the research evidence. Orthop Nurs. 2004; 23(1):30-8.
18. Magnan MA, Maklebust J. The nursing process and pressure ulcer prevention: making the connection. Adv Skin Would Care. 2009; 22(2): 83-92.
19. Duff LA, Kitson AL, Seers K, Humphris D. Clinical guidelines: an introduction to their development and implementation. J Adv Nurs. 2007; 23:887-95.