RESEARCH ARTICLES
Quality of life of caregivers of the Alzheimer's Disease patient
Bruna Mantovani BagneI; Renata Cristina GasparinoII
INurse of the University Hospital, Faculty of Medicine of Jundiaí. Post-Graduation Student in Nursing Intensive Care by the Faculty of Medicine of Jundiaí, São Paulo, Brazil. E-mail: brunabagne@yahoo.com.br.ABSTRACT: The purpose of the study was to evaluate the quality of life of the caregiver of the Alzheimer patient and his relationship with the level of functional independence of the patient. The quantitative study was performed with 66 caregivers, at the Support Center for Aged People in Jundiaí between the months of May and August 2011, and the instruments that were utilized for the data gathering, were the Quality of Life – Bref developed by the World Health Organization, and the Measure of Functional Independence. The quality of life resulted in an average of 65.2 points for the physical domain; 57.1 for the psychological one; 62.6 for social relations; 54.6 for environment; 65 for the general issue of the life quality and 58.7 for the general evaluation of the health. No significant correlation was found out among the instruments. The evaluation of the quality of life can contribute to the diminution of the process by which the caregiver becomes sick, doing it by means of the development of strategies by the professionals.
Keywords: Quality; caregivers; Alzheimer disease; dependent aged person.
INTRODUCTION
The concept of the elderly faces two focus, biological and instrumental. The biological concept involves the aging process, characterized by the population aged over 60 years old. The instrumental concept are facing the social focus, associated with family situation, the labor market and other aspects1.2.
According to the Brazilian Institute of Geography and Statistics (IBGE), Brazil's population is aging. The population aged 60 years old and over are 8.6% of the total population and this number may exceed 30 million over the next 25 years1.
This increase in life expectancy has contributed to the rising cost of chronic diseases such as hypertension, vascular disorders, cancer and Alzheimer's disease (AD)2.
Considering the increasing number of elderly in Brazil and the world, the development of chronic diseases and the consequent increase in the number of caregivers highlighted the importance of identifying the aspects of quality of life of caregivers suffering most changes in order to develop actions that minimize these factors, whether the objectives as they relate to problems arising in everyday life, such as financial difficulties, health problems and neighborhood or as subjective feelings of overload, resentment and exclusion3.
The present study aimed to evaluate the quality of life of caregivers of patients with Alzheimer's disease and their relationship to the level of functional independence of the carrier.
LITERATURE REVIEW
AD is the most prevalent form of dementia in Brazil and can be conceptualized as a degenerative, progressive, irreversible disease and that results from the loss of brain cells that impairs mental behavior of the patient, affecting their physical, mental and social integrity and independence, and if necessary, in more advanced stages, increasingly complex care4.
AD is a disease prevalent in people over the age of 60 years old. When it reaches this age, it is called senile, characterized by their slow evolution. However, dementia may arise after 40 years old, called pre-senile characterized by an aggressive, rapid and intense evolution4.
Diagnosis is based on history, clinical, laboratory and imaging evaluation. Besides them, information tests as the mini-mental state examination Folstein, clock drawing test and verbal function can be used. All these tests are intended to rule out other pathologies, since none of them is conclusive for the diagnosis of AD5.
A recent memory is most affected by the disease, and preserved the old memory. The act of driving, handling equipment and remembering usual places may be affected at the onset of dementia and is at this time that the treatment appears to be more effective, however, as this phase is often confused with normal aging, treatment, often turns out to not start at the right time5.
The patient with AD can cross three stages of the disease: the first is characterized by cognitive impairment with mild forms of forgetfulness, memory loss, neglect of appearance, difficulty performing daily activities, disorientation in time and space, and emotional changes functional changes such as difficulty performing activities of daily life, requiring the supervision of a caregiver5.
The second stage is characterized by an enhancement of cognitive impairments, such as severe memory loss disturbance (difficulty in recognizing individuals, loss of past memories, decreased logical reasoning), emotional changes such as aggression, impaired of self-judgment and accentuation of functional change. At this stage, the patient longer requires the assistance of a caregiver5.
The third stage is characterized by weight loss, delusions and hallucinations, mutism and extreme irritability. It is the stage on which the holder of dementia is totally dependent on a caregiver5.
The concept of caregiver is still being discussed and therefore there is no consensus on its definition. Thus, some authors define as the caregiver responsible for managing the resources the patient needs4.
The caregiver plays a vital role in the daily lives of patients with AD, engaging in all methods of care and acquiring additional responsibilities during the course of the disease. During the development of dementia, it is necessary that the caregiver assists the patient in basic daily living activities such as hygiene care, feeding, medication administration and financial administration6.
Caring for a person with AD is not an easy job as it requires time, energy and patience. Caregivers are exposed to overloads that can cause social, physical and psychological problems. Impaired quality of life of caregivers is quite common and can be evidenced by the presence of depression and exhaustion due to progressive wear6.7.
Quality of life can be defined as the individual's perception of their life, including their culture, expectations and value systems. Therefore, the quality of life is linked to self-esteem and personal well being, among various aspects such as socioeconomic status, emotional state, family support, ethical cultural, health conditions, among others5.
METHODOLOGY
The quantitative, descriptive, cross-sectional study was conducted at the Reference Center for Elderly of Jundiaí (CRIJU), inaugurated in 2008 with the aim to converge to a single location all services and actions aimed at the elderly, reaching quality improvement life thereof, complementing the social safety net of the city of Jundiaí.
123 charts of patients with AD and 66 (53.7%) were analyzed comprised the sample for meeting the following inclusion criteria: patient's caregiver, having more than 18 years old, accepting to participate and sign the Consent free Informed Consent Form (TCLE).
For data collection, the days of consultations of patients with dementia in the clinic were found in the Municipal Information System. On these dates, the researcher went to that place, searched for their caregivers, explained the objectives of the study and those who met the inclusion criteria were included in the sample.
Participants were interviewed in the waiting room, before or after the consultation. The researcher due to the difficulty of reading some participants completed the instruments. Data collection lasted four months, starting in May and ending in August 2011.
Data were collected only after the assent of the Faculty of Medicine of Jundiaí Research Ethics Committee (Protocol 90/2011) and authorization of the responsible for the CRIJU.
For data collection were used: Record sample characterization, the Functional Independence Measure instrument and the World Health Organization (WHO) to assess quality of life World Health Organization Quality of Life Bref (WHOQOL-Bref).
The record of characterization prepared by the researchers, addressed patient characteristics (sex, age and time of diagnosis) and caregivers (such as gender, age, marital status, kinship, income, occupation, participation in support groups, time spent with care and average time as a caregiver).
The Functional Independence Measure (FIM) was developed in North America in the 1980s. Brazilian version of the FIM was developed in 2000, through the adaptation and cultural validation process8. The instrument consists of 18 items grouped into six dimensions: self-care, sphincter control, mobility, locomotion, communication and social cognition9.
The dimension of self-care is composed of six items (A, B, C, D, E and F), namely, eating, hygiene, bathing, dressing, above the waist, to wear below the waist and using toilet9.
The dimension of the sphincter control consists of two items (G and H), namely, control urine and stool control. The mobility dimension consists of three items (I, J and K), namely, transferring from bed to chair, chair to toilet and shower to chair9.
The dimension locomotion is composed of two items (L and M), namely, ability to walk and climb stairs. The communication dimension is also composed of two items (N and O), namely, understanding and expression and social cognition scale consists of three items (P, Q and R), namely, social interaction, problem solving and memory9.
Items are assessed by a Likert Scale ranging from one to seven points, and one is the total dependence and seven, full independence. Therefore, the higher the score the higher the independence of the carrier of the disease. The total score is achieved by summing the scores for each dimension and can vary between 18 and 126 points9.
For the classification of dependence, patients who present a score of 18 will be classified as completely dependent. Scores between 19 and 60, classified a modified dependence on the carrier, i.e., 50% require assistance in performing the tasks. The patient who obtains a score between 61 and 103 points will also be classified as modified dependence, however, requiring only 25% of care in performing the tasks and scores above 104 points ranks as the bearer fully independent9.
c) The WHOQOL-BREF is an abbreviated version of the WHOQOL-100, both developed by the Group Quality of Life Division of Mental Health, WHO, and international use with availability in 20 languages. This instrument was developed because of the need for short and quick application instrument for assessing quality of life. The Portuguese version was adapted for Brazil in the WHOQOL Centre, Department of Psychiatry and Forensic Medicine, Faculty of Medicine, Federal University of Rio Grande do Sul. It is composed of 26 questions, two general questions and the remaining 24 facets are grouped in four areas: (1) Physical, (2) Psychology (3) Social Relations and (4) Environment10.
The physical domain consists of seven items (3, 4, 10, 15, 16, 17 and 18), addresses concepts such as pain and discomfort, energy and fatigue, sleep and rest, mobility, activities of daily living, dependence on medication or treatments and ability to work10.
The psychological domain, consisting of six items (5, 6, 7, 11 and 26), deals with the concepts of positive feelings, thinking, learning, memory and concentration, body image and appearance, negative feelings and spirituality, religion and personal beliefs10.
The domain social relation, consists of three items (20, 21, 22), deals with the concepts of personal relationships, social support and sexual activity and the environment domain, composed of eight items (8, 9, 12, 13, 14, 23, 24 and 25), deals with the concepts of physical security and protection, home environment, financial, health and social care10.
The questions are evaluated by a Likert type scale, ranging from one to five points, i,e,, the higher the score, the better the perception of quality of life, with the exception of the three, four and 26 items that have opposite score10. The final score of general quality of life, satisfaction with health and domains is obtained by the sum of the subjects' responses to each item.
Data were tabulated in Excel® and analyzed by a professional statistician using the Statistical Analysis Software (SAS) version 9.2. Descriptive statistics were used for categorical variables and position measurements of continuous variables. The calculation of domains of quality of life WHOQOL-Bref was performed according to the indications of validation9.10.
To study the domains of nominal variables with two categories, the Mann-Whitney test was used and for variables with three or more categories, the Kruskal-Wallis test. The correlation between FIM and single issues of the domains of quality of life was assessed using the Spearman correlation coefficient.
The reliability of the total items was assessed through internal consistency by calculating the Cronbach's alpha coefficient, which is considered as acceptable lower limit value of 0.6011. The significance level was 5%, that is, p-value <0.05.
RESULTS AND DISCUSSION
Most patients with AD were female - 46 (69.7%) with a mean age of 80.2 years OLD dp ± 7.3) and mean time to diagnosis of disease 3.1 years (dp ± 2.5).
One of the risk factors for AD is age, a fact that justifies the high average age of the patients. Every years, from 65, it doubles the risk of developing dementia2.
For the implementation of the Functional Independence Measure, 7 (10.6%) patients were classified as completely independent, 42 (63.6%) as modified dependence, requiring 25% of aid in their daily tasks, followed by 12 (18.2%) patients who required 50% of aid in the daily tasks and 5 (7.6%) were classified as completely dependent.
Most patients with AD was classified as modified dependence, requiring 25% of assistance in the tasks to be performed. It can be inferred that patients with AD at early stages have a lower dependence on the patients, so the more severe the later stages of the stage will be the largest patient hours devoted to caring for them.
The sample was comprised of 66 caregivers of patients with AD, mean age 54.6 years old (dp ± 12.3) and mean time as caretaker of 4.1 years (dp ± 5.4). When comparing the average time as a caregiver with the time of diagnosis of dementia client, it is observed that the caregiver already did care even before the diagnosis of the disease, because the AD is not easy to diagnose, since the first signs clinical dementia are mistaken for the aging process and there are no adequate screening tests, biological markers and specific tests for diagnosis5.
As the disease progresses, the need for care by the carrier, grows daily, requiring the caregiver to devote himself fully, which hinders the participation of them in social activities12.
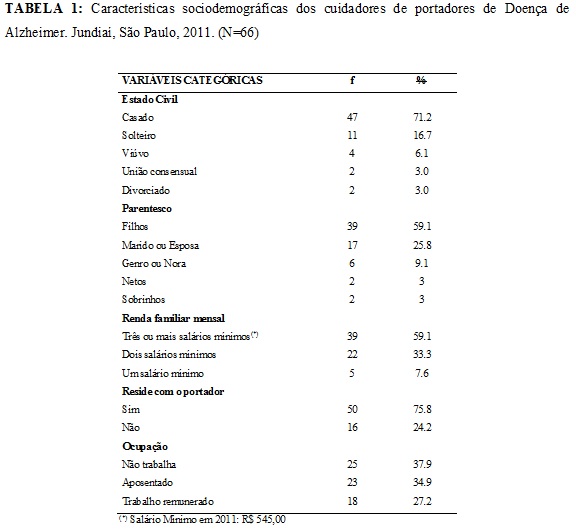
Most were female - 53 (80.3%), married - 47 (71.2%), was the son of the patients - 39 (59.1%) had a monthly income of three or more minimum wages - 39 (59.1%), lived with the patient of dementia - 50 (75.8%), not working - 25 (37.9%) did not participate in groups for the caregivers 62 (93.9%) and reported be without any family support in the provision of care - 42 (63.6%). These data are shown in Table 1.
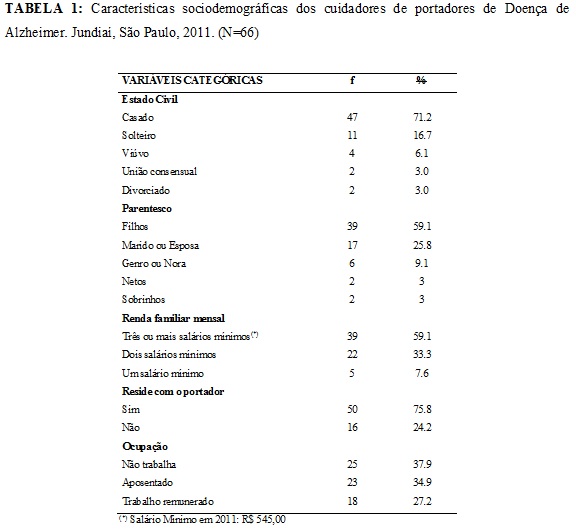
As in other studies, the presence of females were predominant because culturally women are the caregivers and therefore the role of caregiver is expected to society charge13,14.
Surveys show that most elderly people live with their spouse and/or children. The fact that caregivers hold the degree of kinship children can be explained by consideration of the care received in the past, which is a determining factor for the caregiver dedicated entirely to the patient throughout the course of the disease15.
Studies corroborate the data found in this study, with regard to the occupation. Caregivers did not have an occupation outside the home, as were dedicated to caring for those with dementia13,16.
By analyzing the time spent on care, 30 (45.5%) of caregivers were designed 12 or more hours of care to patients, 13 (19.7%) of six to ten and 23 (34.9%) were spending less than five hours daily with care.
The fact that the majority of caregivers living with dementia and the patient of a long exercise workload of care for the elderly can contribute to a worsening of the quality of life of them17-19.
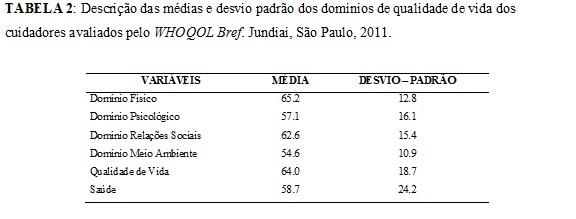
As regards the quality of life, the means found for the domains are shown in Table 2.
In assessing the domains, we observed that the social relationships domain was found significant difference with the variable receiving support from other people in care for patients. Those who relied on this support, achieved higher averages, indicating better quality of life in this area (p=0.0153).
When comparing the quality of life of caregivers in this research, the different domains of the WHOQOL-Bref, with another study with caregivers of dependent patients perceive that the results were very similar9.
Results confirm those of other authors with regard to the relationship between the social relationships domain and support received by the caregiver. It is extremely important that the caregiver receive support from their families, since the overhead due to the implementation of the tasks, added to financial difficulties, management with the holder of dementia, physical and mental fatigue contribute to the onset of stress and consequent worsening of quality of life4,18.
Regarding the environment domain was a significant difference with the variable monthly family income. Families with higher incomes had higher averages, indicating better quality of life (p=0.0365).
In the environment domain was observed relative to family income and other studies suggest that income represents another stressful for the caregiver factor because most do not exercise activity paid for to devote himself to the care of the patient and therefore needs to compose resources to meet the financial needs of family9.
As for the psychological domain significant difference was observed with the variable time spent with care. Caregivers who spent less than five hours per day with care to the patient of dementia had higher averages in the instrument of evaluation of quality of life (p = 0.0391).
With regard to general quality of life, once again, it was noted the importance of time spent with care, where those who dispensed more time to patients had lower averages, i.e., had poorer quality of life (p = 0, 0211).
No significant differences between the domains of WHOQOL-Bref and MIF were found.
Although no significant differences were found between the instrument that assesses the quality of life and what measures the functional independence of the patiene, we found significant results on the time spent on care in the psychological domain and the general issue of quality of life. As the development of dementia, the patient presents difficulties in developing the activities of daily life. Thus, the greater the dependence largest carrier will be the demand for care, which contributes to a psychological burden and patient quality of life of the caregiver12,18,19.
The Cronbach alpha achieved for the domains of the WHOQOL-Bref was satisfactory: 0.67 for the physical domain; 0.64 for the psychological; 0.72 for the social relationships domain; 0.62 for the environment; 0.73 for the general issue of quality of life and 0.68 for satisfaction with health. The reliability for the total items was 0.73.
CONCLUSION
The quality of life of caregivers of patients with AD was assessed using the WHOQOL Bref and resulted in the physical domain to an average of 65.2; 57.1 for the psychological domain; 62.6 to 54.6 social relations and the environment. In general issue of quality of life achieved average was 64 points and for general health assessment 58.7. No significant relationship between the instrument that assesses the quality of life of the caregiver and the instrument that measures the extent of the functional independence of the patient was found.
This research contributes to assist health professionals to develop a more individualized caregiver assistance, developing strategies that can allow them to receive support from others in care for patients and to seek benefits and social assistance. Thus, improving the quality of life of the caregiver can help to reduce their own process of illness and exhaustion.
REFERENCES
1. Ministério da Saúde (Br). Estatuto do idoso. 2ª ed. Brasília (DF): Editora MS; 2009.
2. Freitas ICC, Paula KCC, Soares JL, Parente ACM. Convivendo com o portador de Alzheimer: perspectivas do familiar cuidador.Rev Bras Enferm. 2008; 61:508-13.
3. Lemos ND, Gazzola JM, Ramos LR. Cuidando do paciente com Alzheimer: o impacto da doença no cuidador.Saude soc. 2006; 15:170-9.
4. Luzardo AR, Gorini MIPC, Silva APSS. Características de idosos com doença de Alzheimer e seus cuidadores: uma série de casos em um serviço de neurogeriatria.Texto contexto - enferm. 2006; 15:587-94.
5. Cruz MN, Hamdan AC. O impacto da doença de Alzheimer no cuidador.Psicol estud. 2008; 13:223-9.
6. Garrido R, Almeida OP. Distúrbios de comportamento em pacientes com demência: impacto sobre a vida do cuidador.Arq Neuro-Psiquiatr. 1999; 57:427-34.
7. Paula JA, Roque FP, Araujo FS. Qualidade de vida em cuidadores de idosos portadores de demência de Alzheimer.J bras psiquiatr. 2008; 57:283-7.
8. Ribeiro M, Miyazaki MH, Jucá SSH, Sakamoto H, Potiguarra P, Pinto N, et al. Validação da versão brasileira da medida de independência funcional. Acta Fisiatr. 2004; 11:72-6.
9. Amendola F, Oliveira MAC, Alvarenga MRM. Qualidade de vida de cuidadores de pacientes dependentes no programa de saúde da família. Texto contexto - enferm. 2008; 17:266-72.
10. Fleck MPA, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. Aplicação da versão em português do instrumento abreviado de avaliação da qualidade de vida WHOQOL-Bref. Rev Saude Publica 2000; 34:178-83.
11. Hair Jr JF, Anderson RE, Tatham RL, Black WC. Análise multivariada de dados. 5a ed. Porto Alegre (RS): Bookman; 2005.
12. Caldeira APS, Ribeiro RCHM. O enfrentamento do cuidador do idoso com Alzheirmer. Arq Ciênc Saúde 2004; 11(2):X-X.
13. Karsch UM. Idosos dependentes: famílias e cuidadores. Cad Saúde Pública 2003; 19:861-6.
14. Martins JJ, Silva RM, Nascimento ERP, Coelho FL, Schweitzer G, Silva RDM, Erdmann AL. Idosos com necessidades de cuidado domiciliar. Rev enferm UERJ. 2008; 16:319-25.
15. Mazza MMPR, Lefèvre F.Cuidar em família: análise da representação social do cuidador familiar com idoso. Rev Bras crescimento desenvolv hum. 2005; 15:1-10.
16.Inouye K, Pedrazzani ES, Pavarini SCI. Implicações da doença de Alzheimer na qualidade de vida do cuidador: um estudo comparativo. Cad Saúde Pública. 2010; 26:891-9.
17. Pinto MF, Barbosa DA, Ferreti CEL, Souza LF, Fram DS, Belasco AGS. Qualidade de vida de cuidadores de idosos com doença de Alzheimer.Acta Paul Enferm. 2009; 22:652-7.
18. Aguiar ESS, Gomes IP, Fernando MGM, Silva AO. Representações do cuidar de idosos para cuidadores: revisão de literatura. Ver enferm UERJ. 2011; 19:485-90.
19. Day CB, Paskulin L. Benefícios da atenção domiciliar ao idoso portador de dano crônico: revisão sistemática da literatura. Rev enferm UERJ. 2013; 21: 384-90.