RESEARCH ARTICLES
Analysis of the epidemiological profile of leprosy at Maricá, Rio de Janeiro: a contribution from nursing
João Carlos Fialho de OliveiraI; Ana Maria Machado LeãoII; Fernanda Vasconcelos Spitz BrittoIII
IGraduated in Nursing by the Nursing School from the State University of Rio de Janeiro. Brazil. E-mail: jo_ca_joca@hotmail.com.
IIMaster in Nursing. Assistant Professor in Nursing Department in Public Health from the Nursing School at the State University of Rio de Janeiro. Brazil. E-mail: ammleao@gmail.com.
IIIMaster in Nursing. Municipal Secretary of Health from Maricá. Rio de Janeiro, Brazil. E-mail: fespitz@gmail.com.
IV1st award in ENFCUIDAR. Nursing School of the State University of Rio de Janeiro. Brazil, 2014.
DOI: http://dx.doi.org/10.12957/reuerj.2014.13400
ABSTRACT: The study aimed at analyzing epidemiological profile of leprosy in the city of Maricá, Rio de Janeiro, Brazil, from 2000 to 2013. This is a retrospective epidemiological study with quantitative approach. Data collected of all leprosy cases from Notifiable Diseases Information System Database through the notification of patients with leprosy. The variables included were: new cases diagnosed within the 2000-2013 span; age; clinic forms; operational classification; degree of physical disability and system output. 191 patients were reported: 54% males, 96% are older than 15 years old, 34% were in the virchowian leprosy, tuberculoid (30%), dimorphic (19%) and indeterminate (13%), 63% multibacillary forms, 87.5% had had discharges after cure as main type of system output. Annual detection rate remained medium for those over 15. All those examined showed physical disability to a certain extent at diagnosis time. We concluded that the epidemiological knowledge of leprosy in the city must require stronger support for disease control.
Keywords: Leprosy; epidemiology; nursing; public health.
INTRODUCTION
Leprosy has been known since biblical times:
And it happened that, when I was in a certain city, a man full of leprosy: looking at Jesus fell on his face, and besought him, saying: Lord, if thou wilt, thou canst make me clean. And he put forth his hand and touched him, saying, I will; be thou clean. And immediately the leprosy left him1:72.
At that time, Hansen´s disease was also known as leprosy. Mutilations and ignorance generated fear, prejudiced attitudes of rejection and discrimination of its bearer. The history of leprosy is known and runs through to the present days in the minds of many people contributing to stigma and other adverse effects. Therefore, in 1995 the Brazilian government decided to change the term leprosy by Law 9.0102,3.
It is an infectious chronic disease caused by the bacterium Mycobacterium leprae, with the ability to infect a large number of individuals, however, fewer of them get sick. Therefore, the household is considered an important area of disease transmission2,4.
According to the epidemiological bulletin of the World Health Organization (WHO), the detection rate in the Americas was 4.18 cases every 100,000 inhabitants in 2011. In these regions the data were strongly influenced by Brazil with 33,955 cases - the second country with more cases in the world - with 16% of new cases (in 2011) recorded in Brazil, after India (58%) and followed by Indonesia (9%)5.
In Brazil, there is a high detection in some states of the North, Northeast and Midwest, but the trend of detection of new cases of leprosy is decreasing in the country. In addition to the epidemiological differences, the information presented allow viewing operational problems that reveal the need for greater involvement of states in the implementation of strategic actions provided in the Pact for Life, Green and Healthy Environments Program and the Growth Acceleration Program (PAC) – Mais Saúde, to improve integral care to people with leprosy or sequels of the disease6.
The new case detection indicator replaced the goal for leprosy elimination, based on the prevalence indicator. The Southeast Region and the State of Rio de Janeiro have decrease trend, statistically significant of detection rates. The metropolitan region of Rio de Janeiro concentrates 80% of new cases, suggesting a relationship between high detection rates, higher population density and more decentralized health facilities6,7.
It is expected this study contributing to the guidance of professionals, especially nurses working with health planning and policy management and then expanding access and care. Therefore, the objective of this study is to survey the situation of leprosy in the city of Maricá, from 2000 to 2013, aiming to analyze the epidemiology profile of leprosy in the city of Maricá, during these 14 years.
The city was chosen due to the professional experience of one of the authors of this study and her performance in Hansen’s disease program. The choice of the time delimitation from 2000 to 2013 is justified because of the programs in the Ministry of Health (MS), with the goal of this disease elimination.
The previous goal, established by WHO to eliminate leprosy as a public health problem was the reduction of prevalence to less than 1 case every 10,000 inhabitants by the end of 2005, and then by the end of 2010, a criteria not met in Brazil8. Therefore, there was extension of the deadline until 20159.
LITERATURE REVIEW
In 2002, MS released guidelines for health professionals in order to improve measures to integration and effectiveness of disease control actions in primary health network, such as a differential diagnosis of leprosy; understand the epidemiological aspects related to the etiological agent and the way of transmission; as its clinical aspects such as dermatological and neurological signs and symptoms. They also feature the most important and updated knowledge to patient´s care, then setting a relevant tool for adequately resolving assistance2.
In this context, the control of leprosy in Brazil requires partnerships, large social mobilization, political managers’ disposition, commitment and motivation of technical and social control6. Being a disease with inherent aggravating as a socio-economic and cultural disease, it is also marked by the psychological impact generated by the possible deformities and disabilities resulting from the disease process. These deformities and disabilities are one of the causes of stigma and isolation of the individual in society10.
Among health professionals, nurses have a fundamental role in controlling the disease, because they are in direct contact with the community, in primary care programs and centers of care to patients with leprosy. Therefore, they facilitate treatment to improve the quality of life of the affected patient11.
METHODOLOGY
The population of the city of Maricá, State of Rio de Janeiro was studied, with 139,552 inhabitants in 2013, in an area of 362.57 km², with a population density of 351.55 inhabitants/km² 12.
This is a retrospective epidemiological study with quantitative and analytical approach, carried out with data from the Notifiable Diseases Information System (SINAN) to identify the epidemiological profile of leprosy in Maricá, from 2000 to 2013.
Inclusion criteria were patients´ reports diagnosed with leprosy in the city of Maricá, registered in SINAN in the chosen period. Exclusion criteria were dubious, incomplete notifications, with different registration period and variables not selected for this study.
SINAN was used as a source of information, related to Municipal Health Department data of Maricá (SMSM). To meet the objective of the study the following variables were selected: number of reported cases from 2000 to 2013; age (younger and older than 15 years); gender; clinical forms of the disease based on Madrid classification from 195313; operational classification paucibacillary (PB) or multibacillary (MB); physical disability degree (GIF); and the type of output system.
The study sample was people who got sick of leprosy in that period. Data collection was carried out in stages, including variables shown in SINAN, incorporated into Microsoft Excel 2007 spreadsheet. For statistical analysis, data were presented in absolute and relative percentage rate, presented in tables.
Based on Ordinance Number 3,125, of October 7, 2010, approving the guidelines for surveillance, care and leprosy control14, the epidemiological profile was created.
SINAN has reporting and investigation of diseases and disorders cases, which appear on the national list of notifiable diseases, including leprosy, where each index case should be informed in epidemiological week of occurrence, by surveillance professionals, using an specific record, in the three levels of health care14.
This study is a documentary and electronic research. Therefore, the approval by the Ethics Committee in Research was not necessary. Authorization to SMSM was asked through official letter number 624/2014, for the municipal data collection in SINAN.
After approval/acceptance of the research, data collection began into the system in May 2014.
RESULTS AND DISCUSSION
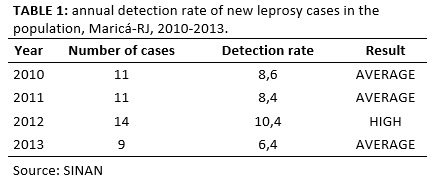
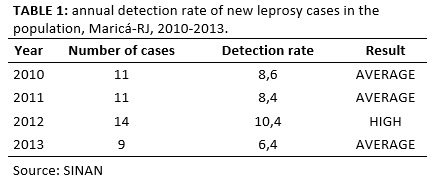
From 2000 to 2013, 191 patients of Maricá were notified in SINAN. The detection rate from 2000 to 2009 was not calculated due to lack of registration of the population by the Brazilian Institute of Geography and Statistics (IBGE). It is known that in the period from 2010 to 2013, the detection rate classification ranged in average from 2 to 9.99 cases/100,000 inhabitants and high from 10 to 19.99 cases/100,000 inhabitants as shown in Table 1.
The age analysis of the cases reveals that most of them - 183 (96%) - were 15 years old or more and in 8 (4%) cases investigated they were below 15 years old. The relationship between age and gender showed the disease more in men from 60 to 69 years old and women from 20 to 29 years old and 30 to 39 years old. A study showed that leprosy affected people from 30 to 49 years old predominantly15. These results are in part the age profile of this research population.
The rate in children under 15 years old, reached a high level (5.0 to 9.99/100,000 inhabitants.) during the 14 years evaluated in this study. It indicates the possibility of the disease spread and the recent transmission intensity of the endemic14. This data is important because the reduction of cases in children under 15 years old is a priority of the National Leprosy Control Plan, as an indicator of leprosy elimination in PAC – Mais Saúde6.
This study is similar to other studies showing the involvement of leprosy in older people. This high frequency in adults is due to the long period of incubation bacilli, ranging from 2 to 7 years. Moreover, leprosy affects economically active people, and it brings economic and social losses, interfering with the ability to perform daily activities of affected individuals, regardless GIF they present15-17.
The big increase in notifications in Maricá in 2005 is a result of large nationally advertising campaign from the government launched in 2004 to fight against leprosy in the country, including its elimination in Brazil until the end of 2005.
To increase notifications from 2000 to 2013, there were implementation of control policies, the organization of the health system and mandatory reporting of leprosy, which were structured around the country, through research mandatory in all health care levels. The diagnosed cases must be officially communicated, using the specific record of notification and investigation of SINAN14. Other factors influenced, as the actual existence of transmitters cases and the diagnostic agility in the health system, operational changes in the epidemiological surveillance system, some known other unknown and its decentralization of the health care system18.
The variations of cases observed were mainly caused by fluctuations of the transmission of leprosy and operational programs changes19. Paradoxically, there is a decreasing in cases in Brazil - especially in Maricá, as the diagnosis and treatment of patients were performed by the decentralization strategies, assistance supported by MS protocols19.
In gender analysis, most of the cases - 103 (53.6%) – were in men, except in 2001, 2010 and 2012, when most were represented by women with 9 (64.2%), 6 (54.5%) and 11 (73.3%) cases, respectively, according to Table 2.
TABLE 2: Profile of diagnosed and notified patients in Notifiable Diseases Information System, Maricá-RJ, 2000-2013.

Source:
SINAN
Legend: TNE-Transfer unspecified; TM-city transfer; TE-state transfer
Also in another study conducted in Maranhão, most cases were from male. This indicates that man is the most affected. However, in the same study, it is reported an increase number of cases in women16.
Considering the clinical forms, there was a predominance of virchowian in 34.2% of cases, followed by tuberculoid (30%), undetermined (13.4%), borderline (18.7%) and unclassified forms (3.7 %) as seen in Table 2. This study showed a greater incidence of multibacillary (MB - patient over five skin lesions). They are at risk for transmission, while the paucibacillary (PB patients with up to five lesions) have lower risk of transmission to individuals who are in close contact20.
Other research also showed similar results17, although other studies stated that PB is not transmissible due to low production of bacilli21. As more MB cases, there is an increasing endemic, when the most susceptible individuals are affected and with an inefficient primary and epidemiological service system that allows the perpetuation of the transmission focus22.
At the same time, patient groups studied with PB leprosy showed little decrease in quality of life. This leads to the conclusion that as earlier diagnosis and treatment, the lower quality of life impairment23.
There is disagreement in MB records (virchowian and borderline forms) and PB (tuberculoid and undetermined) because 180 people got sick according to clinical forms. This could be due to the loss of some information during the system updates for notification. It is worth mentioning that the total PB recorded highlights 71 patients, therefore, the sum of 25 cases - undetermined - with 56 cases - tuberculoid type - recorded was different; this also occurred in the total of 64 cases in virchowian and 35 cases in the borderline form, being 99 MB patients, probably due to errors in classification or records.
Thus, in the studied population, MB was predominant with 62.5%. There was an error in records and values not matching the clinical forms. From this reality – from the difficulty of confirming the clinical forms, as established by Madrid classification13 - MS operational classification (PB and MB)2 simplifies and facilitates this procedure in order to effect treatment of the patient, because treatment will start with the case definition.
Observing the clinical forms in the population, there was an increase from 2000 to 2005 and a significant decrease from 2006, with a stabilization trend. The predominant clinical presentation was virchowian with 64 cases (34%) added to 120 MB cases (62.5%) found. The sum of virchowian and borderline leads to the prevalence of contagious forms, late identified. Thus, there would be bacillus transmitters without early diagnosis without professional judgment able to do a complete physical examination. However, from 2007 to 2011, it can be seen more PB forms (due to tuberculoid type) than MB, since tuberculoid affects resistant individuals, while the borderline and virchowian imply the perpetuation of the transmission, with significant disabling power24 .
There were 157 patients exanimated (85.8%) of the 183 enrolled, and 51 (27.9%) had some GIF (1 or 2). There were no cases with GIF 2 from 2000 to 2002, 2007 and 2008; and the proportion of leprosy cases with GIF 2, at diagnosis, were considered medium (5 to 9.9%) for the period from 2004 to 2006; from 2009 to 2013 was high (greater or equal to 10%). In this study, there were 157 (85.8%) patients evaluated for GIF in all years studied, showing that all of them had some GIF (1 or 2). The estimated number of 85.8% with disability is considered unsatisfactory, being less than the amount evaluated in the State of Rio de Janeiro from 2001 to 2008, where it reached 88.4% in the period cited6.
There were 106 (67.5%) patients without disability (grade - zero) and 33 (21%) with GIF - 1 and 18 (11.46%) with GIF - 2, in Maricá. The predominance of GIF - zero is reported in other studies22,25. The percentages of cases with GIF- 2, at diagnosis, were low in 2003 and then, predominantly medium and high, corroborating the findings of the State of Rio de Janeiro from 2001 to 20086. In Brazil, 23.3% of the new cases are related to GIF - 1 and GIF - 210.
GIF, related to disease duration, is an indicator that allows an indirect assessment of the effectiveness of early detection activities and appropriate treatment of cases26.
The predominant MB and low percentage of GIF - 2 show the delay in diagnosis in the area, therefore, evidence allows supposing the lack of preparation for the recognition of the complications of this mycobacteriosis, being able to question the epidemiology of the disease control in the locality27.
GIF is the evaluation indicating the existence of loss of protective sensation and/or visible deformities as result of nerve damage10.
GIF – 2 is: in the eyes, the presence of any signs and/or symptoms such as lagophthalmos and/or ectropion, trichiasis, central corneal opacity and even blindness; in the hands, trophic lesions and/or traumatic injuries, claws, resorption and fallen hand; and in the feet, ulcerations and/or traumatic injuries, claws, resorption, drop foot and ankle contracture10:109.
These lesions are caused by disorders of the peripheral nerves and their sensory, motor and autonomic fibers, and the facial nerve (cranial nerve VII), trigeminal nerve (cranial nerve V), ulnar nerve, median nerve, radial nerve, common peroneal nerve and most frequently nerve involved in tibial10.
During the study period, 184 cases were notified with registration about the leaving type of patients in the information system, according to year of diagnosis. There were 161 patients (87.5%) who were discharged after cure, there were 7 (3.8%) deaths and abandonment, 3 (1.63%) had diagnostic error, 3 (1.63) transfers not specified, 2 (1.09%) transfers to another city and 1 (0.54%) transfer to another federal unit. It is worth noting that most of the registered patients had a cure, by completing treatment.
The abandonment leaving should be informed when the patient that has not yet completed the treatment did not attend the health service in the last 12 months, both in PB as the MB cases14. Undesirable situation confirms the lack of the patient's situation by the health unit.
These findings show that the outcome of the disease is interesting: most patients were committed to the treatment and accepted the use of multi-chemotherapy (PQT) as a tool to achieve a cure. It is noteworthy that the cure and treatment of the person are time consuming, through the administration of PQT treatment regimens with compliance with established deadlines: from 6 to 9 months for PB cases and from 12 to 18 months for MB cases2.
Data from another study show that abandonment cases are due to weakness in the credibility of the patient, the medical diagnosis and not accepting the use of PQT, needing attention by the health services to be emphasized in the orientation of bearers, having the awareness that treatment adherence objectively and continuously will take them to disease cure28.
As the leprosy has ignorance or old and preconceived ideas related to social, cultural and emotional issues and due to disease characteristics, nursing professionals, to receive leprosy patients should pay attention to the ethio-legal issues related to prejudice and discrimination in their consultations. Furthermore, nurses can contribute to communities, helping to reduce the spread of the disease and increase the early diagnosis of demand; working with their knowledge and experiences, favoring to face their own stigmas; and helping to positively cope these individuals with the disease, strengthening protective factors, seeking to detect risk factors at work together with the family and support networks and guiding about self-care to prevent disability and maintain positive self-image29-32.
CONCLUSION
MS has the leprosy elimination commitment by 2015, that is, to achieve less than 1 case every 10,000 population. This study found that, in the city of Marica, the magnitude of morbidity had average parameter (6.4 cases/100,000 population) in 2013. Thus, this city is in the right way to control the disease, following the integrated plan of strategic actions from government, since there was a reduction in the number of diagnosed cases and a large number of discharges.
The detection rate - leprosy transmission indicator - decreased over the last four years of the study. Nevertheless, there is bacilli circulation in the city.
Males and people over 15 years old were the most affected. There was a higher number of notifications of virchowian, contributing to most cases of MB and GIF -2 diagnosis. It indicates the delay in detection and early treatment and possible psychological implications, perpetuation of stigma and continuous transmission of the bacilli by sick people.
However, it is important to emphasize the quantitative significant that completed treatment, corresponding to the discharge by cure in the output system. Most of them relied on treatment, medication and health professionals acting because few patients abandoned the treatment.
It is worth mentioning the need to intensify and strengthen surveillance in leprosy, as it subsidizes recommendations, promotion and analysis of the effectiveness of interventions, determining that the records of cases diagnosed and under treatment to be updated continuously. It is essential to disclosing information acquired as a source of planning and evaluation of managers to be triggered.
This study found some limitations such as lack of fulfillment of certain data in the SINAN notification records, hindering a complete and true diagnostic evaluation to the city's reality. Another fact is that all information collected is secondary and depends on the data entry in the information system by a professional, who is not always in the health area.
This research contributes to the guidance of professionals, especially nurses acting in health planning and policy management and prevention and control of transmissible diseases.
REFERENCES
1.Bíblia Sagrada. Antigo e novo testamento. Traduzido em português por João Ferreira de Almeida. 31ª ed. Rio de Janeiro: Editora Contexto 1990. p.72.
2.Ministério da Saúde (Br). Secretaria de Políticas de Saúde. Departamento de Atenção Básica. Guia para o Controle da hanseníase. 3ª ed. Brasília (DF): Ministério da Saúde; 2002.
3.Brasil. Lei 9.010 de 29 de março de 1995. Dispõe sobre a terminologia oficial relativa à hanseníase e dá outras providências. [citado em 15 jun 2014] Disponível em: http://www.planalto.gov.br/ccivil_03/leis/L9010.htm. Acesso em 02 de fevereiro de 2014.
4.Opromolla PA, Laurenti R. Controle da hanseníase no Estado de São Paulo: análise histórica. Rev Saúde Pública. 2011; 45(1):196.
5.Organização Mundial da Saúde. Situação global da hanseníase. Boletim epidemiológico semanal. [Internet]. 2012 ago [citado em 01 fev 2014]; 87:317-28. Disponível em: http://www.who.int/wer/2012/wer8734.pdf?ua=1.
6.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Hanseníase no Brasil dados e indicadores selecionados. Brasília (DF): Ministério da Saúde; 2009.
7.Valle CLP. Situação da hanseníase no estado do Rio de Janeiro no período de 2001 a 2009. Rev Hospital Universitário Pedro Ernesto. 2011;10(1):11-8.
8.Secretaria de Estado de Saúde do Distrito Federal (Br). Governo do Distrito Federal. Hanseníase: Protocolo de Atendimento. Brasília (DF): Subsecretaria de Vigilância à Saúde; 2007.
9.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde.Plano integrado de ações estratégicas de eliminação da hanseníase ... Plano de ação 2011-2015. Brasília (DF): Editora MS; 2012.
10.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Manual de prevenção de incapacidades. Cadernos de prevenção e reabilitação em hanseníase. Brasília (DF); Editora MS; 2008.
11.Silva JMM, Moreira MPS, Silva TMV. O papel do enfermeiro no tratamento da hanseníase. Revista Universo da Enfermagem. 2014; 3(1):57-61.
12.Instituto Brasileiro de Geografia e Estatística. Assistência Médica Sanitária 2009 [Internet]. Rio de Janeiro: IBGE; 2010 [citado em 08 mai 2014]. Disponível em: http://cidades.ibge.gov.br/xtras/perfil.php?codmun=330270.
13.Montenegro RMN, Zandonade E, Molina MDC, Diniz LM. Reactional state and nutritional profile among leprosy patients in the primary health care system, Greater Vitória, Espírito Santo State, Brazil. Cad Saúde Pública. 2012; 28:31-8.
14.ANVISA (Br) Portaria nº 3.125, de 7 de outubro de 2010. Aprova as Diretrizes para Vigilância, Atenção e Controle da hanseníase. [citado em 02 jun 2014]. Disponível em: http://www.anvisa.gov.br/hotsite/talidomida/legis/portaria_n_3125_hanseniase_2010.pdf.
15.Duarte MTC, Ayres JA, Simonett IJP. Perfil socioeconômico e demográfico de portadores de hanseníase atendidos em consulta de enfermagem. Rev Latino-Am Enfermagem [online]. 2007; 15 (spe): 774-9.
16.Corrêa RGCF, Aquino DMC, Caldas AJ, Amaral DKCR, França FS, Mesquita, ERRBPL. Epidemiological, clinical, and operational aspects of leprosy patients assisted at a referral service in
the state of Maranhão, Brazil. Revista da Sociedade Brasileira de Medicina Tropical. 2012; 45(1):89-94.
17.Batista AMN. Avaliação da incapacidade e limitação de atividades em Pacientes afetados pela hanseníase: uma análise do escore Salsa [monografia]. Bauru (SP). Secretaria de Estado da Saúde; 2010.
18.Penna MLF, Oliveira MLW, Carmo EH, Penna GO, Temporão JG. Influência do aumento do acesso à atenção básica no comportamento da taxa de detecção de hanseníase de 1980 a 2006. Revista da Sociedade Brasileira de Medicina Tropical. 2008; 41(supl 2):6-10.
19.Silva Sobrinho RA, Mathias TAF. Perspectivas de eliminação da hanseníase como problema de saúde pública no Estado do Paraná, Brasil. Cad Saúde Pública. 2008; 24:303-14.
20.Murto C, Ariza L, Alencar CH, Chichava AO, Oliveira AR, Kaplan C, Silva LF, Heukelbach J.C Migration among individuals with leprosy: a population-based study in Central Brazil. Cad Saúde Pública. 2014; 30:487-501.
21.Macedo CP, Cerqueira MFF, Poveda VB. Avaliação do perfil epidemiológico da hanseníase em um município do interior paulista nos anos de 2000 à 2006. Revista REENVAP. 2014; 4:13
22.Melão S, Blanco LFO, Mounzer N, Veronezi CCD, Simões PWTA. Perfil epidemiológico dos pacientes com hanseníase no extremo sul de Santa Catarina, no período de 2001 a 2007. Revista da Sociedade Brasileira de Medicina Tropical. 2011; 44:79-84.
23.Bottene IMC, Reis VMS. Quality of life of patients with paucibacillary leprosy. An Bras Dermatol. 2012; 87:408-11.
24.Crespo MJI, Gonçalves A, Padovani CR. Hanseníase: pauci e multibacilares estão sendo diferentes? Medicina (Ribeirão Preto) 2014; 47:43-50.
25.Freitas RM, Oliveira EL. Hanseníase: avaliação diagnóstica a partir dos dados do SINAN em Itaperuna-RJ. In: Anais XVI Encontro Nacional de Estudos Populacionais. Encontro Nacional de Estudos Populacionais. 2008. Caxambu(MG): set-out 29-03; Rio de Janeiro: Associação Brasileira de Estudos Nacionais; 2008. p. 1-21.
26.Alves CJM, Barreto JA, Fogagnolo L, Contin LA, Nassif PW. Avaliação do grau de incapacidade dos pacientes com diagnóstico de hanseníase em Serviço de Dermatologia do Estado de São Paulo. Revista da Sociedade Brasileira de Medicina Tropical. 2010;43:460-1.
27.Carneiro M, Possuelo LG, Valim ARM. Neuropatia por hanseníase: atraso no diagnóstico ou um diagnóstico difícil? Cad Saúde Pública. 2011;27:2069-70.
28.Luna IT, Beserra EP, Alves MDS, Pinheiro PNC. Adesão ao tratamento da Hanseníase: dificuldades inerentes aos portadores. Rev Bras Enferm. 2010; 63:983-90.
29.Sangi KCC, Miranda LF, Spindola T, Leão AMM. Hanseníase e estado reacional: história de vida de pessoas acometidas. Rev enferm UERJ. 2009; 17:209-14.
30.Santos DAS, Gonçalves RELM, Nascimento AMN, Neto LRC. Hanseníase: diagnóstico precoce é a solução. Revista ParticipAção. 2013. 23/24: 133-41.
31.Bittencourt LP, Carmo AC, Leão AMM, Clos AC. Estigma: percepções sociais reveladas por pessoas acometidas por hanseníase. Rev enferm UERJ. 2010; 18:185-90.
32.Fernandes C, Beltrão BA, Chaves DBR, Leandro TA, Silva VM, Lopes MVO. Avaliação do grau de resiliência de adolescentes com hanseníase. Rev enferm UERJ. 2013; 21:496-501.