INTRODUCTION
Leprosy is a disease that carries with it the marks of fear and prejudice,
often associated with the idea of sin, which has excluded and segregated
sick individuals1. Inevitably, at present, social barriers
involving leprosy make it difficult to manage patients and including their
relatives in the health-disease process.
Therefore, understanding the life history of the family members of
ex-patients is relevant because they have received the stigma of leprosy
even though they had never carried the disease. Besides, this social
condition still permeates those who are currently affected by leprosy.
Establishing strategies developed by health professionals, especially
nurses, in the management of leprosy patients and their relatives in a
holistic and more humanized manner is crucial, especially considering the
social consequences that involve the disease, the patient and their
families.
Based on the assumption that people close to the patient were also
victimized by society in the past, the objective was to identify whether
family members of leprosy patients treated in asylum hospitals were
affected by prejudice, stigma and exclusion that permeated patients' lives.
LITERATURE REVIEW
Leprosy is a chronic, infectious-contagious disease caused by Mycobacterium leprae, which manifests itself through
dermatological and neurological signs and symptoms, especially in the
eyes, hands and feet. Neural impairment alters sensitivity and can lead
to physical disabilities, evolving into deformities, contributing to
prejudice towards the leprosy patient2.
The term Hansen's disease (most used in Brazil) honors the Norwegian
physician, the discoverer of the etiological agent, Gerard Amauer
Hansen, and was officially adopted by the Ministry of Health through
Decree 76.078 of August 4, 1975, ratified by Federal Law 9,010 of March
5, 1995 3
. Such a measure contributed to the construction of a new image of the
disease, since the denotation of leprosy, in Brazil, refers to an
incurable, disfiguring disease that affects impure people, which culminated
in the segregation of sick individuals by removing them from the social
environment and their families4.
Scientific evidence of the contagious character guided control measures
based on deprivation of liberty through policies of compulsory
internment in isolation institutions. Segregation has increased
attitudes of prejudice in society, rooting the socio-cultural
repercussions and negative myths surrounding the disease and the sick
ones 3.
In the State of Rio Grande do Norte (RN), these practices were carried out
at the São Francisco de Assis Asylum Hospital, located in the municipality
of Natal, which remained active for 65 years, from 1929 (year of
inauguration) to 1994 (when it was deactivated).
Compulsory isolation reflected negatively on the lives of leprosy patients
and their families. This prophylactic measure had a police character and
disregarded the social relations that patients had established throughout
their lives, resulting in the breaking of family ties5,
according to what happened with children taken from their parents and put
to live in special education institutions, such as the Oswaldo Cruz School,
built in Natal-RN.
Even in the face of the technical and scientific advent, with the emergence
of drug treatment and cure, the historical marks of leprosy and its
sociocultural repercussions are still present today, observed in practices
of exclusion and segregation of leprosy patients and their relatives in
defense of social welfare4.
When thinking about the stigmatizing and exclusionary burden that
accompanies the disease ancient times, it is understandable that the
history of leprosy has been reproduced in the present, influencing the
process of illness in leprosy by referring to the prejudice and beliefs of
the past, rooted in prejudiced ideas and myths consolidated in the common
sense imagination6.
Currently, leprosy has consisted of a worrying epidemic, establishing
itself as a serious public health problem in Brazil, mainly because of its
incapacitating power if not detected and treated early and adequately,
causing physical and social damages7. In addition, ex-patients
and their families have shown signs of social exclusion, prejudice and
stigma left by the disease when it had no cure and was treated in an asylum
environment 5.
Considering this reality, the performance of public management in the
organization of health services aimed at attention to the patient with
leprosy, as well as the engagement of health professionals, including
the nurse, is essential to provide care in a comprehensive manner,
involving the person carrier of leprosy, the family and their
acquaintances. Practitioner must clarify doubts about the disease in
order to combat stigma and to favor an adequate social living 8.
METHODOLOGY
This is a descriptive and qualitative study using thematic oral history
as a methodological framework, which involves a set of procedures
(project design, definition of the population segment and study
network, questionnaire elaboration, interview, transcription and
analysis) and allows the unveiling of a specific episode experienced by
the collaborator (study subject), who became an active part in the
construction of his/her story when narrating his/her experiences 9.
Following the assumptions of the thematic oral history, the study
population was composed of the 52 relatives of ex-leprosy patients who
were segregated in the São Francisco de Assis Asylum Hospital, from
both genders, aged from 34 to 85 years, enrolled in the Reintegration
Movement of People Affected by Leprosy in Rio Grande do Norte
(MORHAN-Potiguar).
For structuring of the network, researchers considered the kinship
relations by consanguinity of first and second degrees, between the
collaborator and the former patient of leprosy; men and women over the
age of 40; living in Natal-RN, during the period of data collection;
and who agreed to collaborate voluntarily with the study. Exclusion
criteria were: non-preserved mental faculties; and individuals with
communication barriers that could jeopardize the effectiveness of the
interview.
The zero point that started the establishment of the network was a
coordinator of MORHAN-Potiguar, who is son and grandson of a former
leprosy patient and, therefore, someone with a broad knowledge of the
topic addressed in this study and aware of the components of the
population. From the zero point, other participants that composed the
network were recruited, totaling 10 collaborators.
Before data collection, the collaborators were invited to participate
in the survey through telephone contact. The interviews were carried
out at a date and place chosen by the collaborator, making use of a
socioeconomic identification tool, as well as of comprehensive
questions that directed their memories to experiences of the period
when their relative was hospitalized in the asylum hospital, according
to the purpose of the study. The interviews were recorded by audio
recorder, transcribed, contextualized, transcreated and authenticated
by the collaborators with the signing of concession letters9
. The collection and verification of the narratives took place in
Natal-RN during the months of June and July of 2014.
The narrated stories are related to collaborators' experiences as
relatives of former leprosy patients, experienced in their childhood
after the diagnosis of the disease and consequent segregation of the
family member in the São Francisco de Assis Asylum Hospital.
After verifying the transcribed material, the texts were submitted to
the thematic content analysis10, enabling the identification
of thematic axes, which were discussed with the scientific literature.
The accomplishment of this research was approved by the Ethics Research
Committee of the Federal University of Rio Grande do Norte, under
opinion No. 650.654/2014 and
Certificate of Presentation for Ethical Appreciation
No. 25922214.3.0000.5537. Before signing the Free and Informed Consent
Form, collaborators were informed about their participation in the
study. Subjects are presented with color names, preserving their
anonymity.
RESULTS AND DISCUSSION
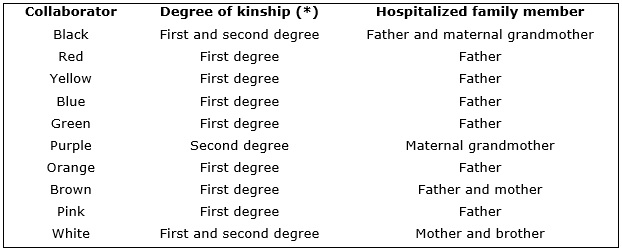
Ten collaborators were interviewed: six men and four women, aged from
44 to 76 years. Regarding the level of education, four of the subjects
have completed the primary education, three studied until the high
school and three referred to have a higher education. The degree of
kinship between the study collaborator and the relative hospitalized in
the São Francisco de Assis Hospital are described in Figure 1.
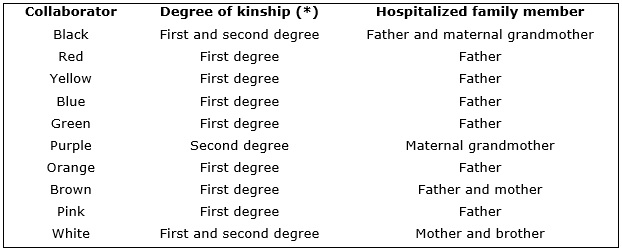
Figure 1 –
Characterization of the degree of kinship existing between the collaborator
and his/her relative who was hospitalized in the São Francisco de Assis
Asylum Hospital. Natal, 2014
* Consanguineous relatives, as established in the Brazilian Civil Code.
Based on the analysis of the thematic oral histories narrated by the
study collaborators, two thematic axes were identified: Stigma and
prejudice and; Social Exclusion.
Stigma and Prejudice
Stigma is defined as a deeply derogatory attribute, a social provision that
promotes disqualification of individuals or groups, making them unfit for
social interaction. The attribute considered socially disqualified can
refer to certain physical characteristics, behavioral and moral deviation
or those transmitted to descendants, such as the tribal stigmas of race,
nation and religion11.
In the midst of studies aimed at stigmatized groups, the one constituted by
leprosy patients, victimized by prejudice and exclusion, stands out.
Throughout history, leprosy has been associated with the socio-cultural
image that disparaged its carriers, leading them to difficulties in
establishing social relations12.
The term leprosy, Brazil, is pejorative and the disease used to stigmatize
not only the patients, but also their relatives 13. Such reality
is observed in the statements of the study collaborators, in which they
confirm the feeling of stigma experienced by the presence of a family
member with leprosy, as shown below.
We could not live with outsiders because they were afraid of leprosy. I
did not have the disease, but my grandmother had. (Purple)
I did not like to hear people say that I was the son of a leper,
although I have heard it many times.
There was this latent prejudice.
(Blue)
In high school, there was a boy that studied with me and he was
forbidden by the older brother to talk to me because I was the son of a
leper. (Orange)
Society has always sought to establish standards to categorize individuals
according to their peculiarities, whether they are common or differentiated
from the population, that is, when introduced to a stranger, one can
recognize the stranger's attributes, which allows predicting the class to
which that person belongs, categorizing him/her in some group or tribe 11.
Specifically with regard to leprosy, stigmatization is related to the body
marks resulting from infection by Microbacterium leprae and to the
exclusion experienced by the disease carrier, physically marked by
deformities in the body14. Unfortunately, the stigma also
affected people who did not have the disease, such as the healthy children
of leprosy patients4. The collaborators who were interviewed
showed that, although they did not have any physical illness, they carried
with them the brand of stigma for being a leper's child.
The defects in my father's body were easily seen, [and by extension]
they marked all of us in the family, so people also had prejudice
against us. (Black)
Our fathers had body defects! That is why there was prejudice and
people were afraid to approach us. (Yellow)
People had prejudice because my mother and my brothers had the disease
[...] And they always criticized me saying that I was the leper's son.
(White)
The stigma of this disease is also associated with the religious tradition,
since it restricts the social role of the individual by associating leprosy
with beliefs about divine punishment and sin. Consequently, many of those
people were socially segregated and victims of prejudices that have
persisted in the present15.
The association between stigma and prejudice was characterized as an
important factor for social exclusion and limitations in several dimensions
of life16. Changes in social relations caused by prejudice and
stigma could be perceived in the reports of the collaborators.
I was raised in a regime of prohibitions and restrictions, both in the
visit to my father in the asylum and in the social living with my
neighbors because prejudice was constant in the neighborhood; people
used to point at us. (Black)
There was so much discrimination and prejudice against us that the day
the school principal announced the names of the first places he told
the people to be careful because we were daughters of lepers. (Pink)
Among the problems in social relationships experienced by the
collaborators, they mentioned prejudice at work, which made life difficult
for those affected by the stigma of leprosy, such as those reported below:
At work, I experienced a lot of prejudice. If I said I came from the
special school, they would probably send me away so as not to lose the
students (Red).
Everyone knew that I had lived in that special school and people were
prejudiced. It was difficult from them to accept me at work at first
(Orange).
Discrimination against stigmatized subjects raises prejudice, culminating
in the rejection of something that is not known about what it really is 12. Individuals marked by stigma are constantly subjected to the
condemnatory meaning of the term; they are seen by society in a distorted
manner, which leads them to social exclusion, as if it were guilty in being
carriers of characteristics considered derogatory to society17.
The marks left on each of the collaborators transcend the scars carried by
their relatives, and the consequences generated by the social and familiar
displacement experienced in the past remains in their memories. These marks
of stigma and prejudice still permeate the reality of today's leprosy
patients due to misinformation.
Prejudice against individuals affected by leprosy is associated with the
lack of knowledge of the disease-related elements, such as its mode of
transmission, existence of treatment and cure. The history of stigma and
prejudice and the lack of information incite fear in uninformed people,
leading to social exclusion of the patient12.
Social exclusion
Given the complexity of the aspects involving social exclusion, it is worth
noting that it is conceived as a heterogeneous phenomenon, which can arise
from different economic, social, cultural or pathological factors 18. The exclusion mechanisms provoked by leprosy are associated
with the disabilities and physical deformities that generate prejudice.
This exclusion has reinforced the segregation structure adopted through the
compulsory isolation of leprosy patients, thus controlling such individuals
that disturbed and haunted society14.
Social exclusion that permeated leprosy was beyond the exclusion
experienced by the sick individual, and also affected their relatives. The
analysis of the narratives allowed observing that the reports related to
social exclusion episodes experienced by the study collaborators were
frequent. The interference imposed in the way of relating to others came
from the presence of a family member with leprosy.
Collaborators who were separated from their sick parents and grandparents,
segregated in a reclusive life in the Oswaldo Cruz School, experienced in
their daily life moments of exclusion materialized in the frustrated
attempt of interacting with individuals of outside the special school to
which they were sent.
I used to run away from the special school to play soccer with the kids
outside. At first nobody knew I was from that school, but after they
discovered it, they did not want me to play and I was soon excluded
from the team. (Purple)
They advised other not to associate with us because we were from the
special school and because my father had leprosy. (Blue)
The outsiders did not like us because we were the leper's children; and
the boys did not want to marry us. (Green)
The segregation of the leprosy patients was explained by the fear of
contagion and by all the mythical imaginary surrounding the disease and the
patient, whereas the exclusion of healthy children who, in addition, lived
in areas far from the sick parents, could be explained by the social
contagion of the disease marks. Consequently, these children used to be
excluded after revealing their origin. It was up to such individuals to
hide their situation in order to establish social relations on an equal
footing4.
The social data of collaborators show they have a low level of education,
with a predominance of the complete primary education. This fact may be
related to the difficulty of interacting with the healthy population, since
even though participants did not have the disease, they were excluded, just
like their relatives with leprosy. This exclusion was perpetuated in the
school context, hampering access to education, as explained in the reports.
At the special school we finished primary school and we could not
continue studying because it would have to be in a school outside, and
we could not leave because we were the son of a leper. (Red)
At the special school, we could only study until the fourth grade and
we could not study abroad because we were considered as the patient
himself and outsiders were afraid of us. (Pink)
We were excluded and had a hard time trying to continue studying after
we finished primary school. It was difficult because people had a lot
of prejudice and we did not like to go outside. (Green)
Collaborators who had access to education outside the special school,
because they did not live in it or because they somehow managed to get a
place in an external school, reported moments of exclusion experienced in
the school environment.
When I went to school they isolated me in a corner of the classroom and
I was separated from those who were healthy [...] I was excluded in the
classroom and they always criticized me. (White)
Often they did not want us to stay close and they would not let us play
soccer with them [...] And when it was time to do work with a partner,
nobody wanted to do it with me. (Orange)
Knowledge of the historical trajectory of leprosy exclusion prevails by
referring to the isolation of patients in the past, leading to the fear of
separation of loved ones. This fear rests on some leprosy patients, who
choose not to reveal the disease and often exclude themselves from
community life so as not to infect loved ones with the disease12
. The reports obtained in the research show the choice of study
collaborators to remain incarcerated for fear of exclusion and, in adopting
this practice, they ended up excluding themselves from experiences and
interactions with the outside world, according to the statements above.
This was a very tough life, with a lot of discrimination, so we were
not aware of the outside world. We could not go by bus because people
were afraid of us, so we used to walk, only. (Pink)
This principal did not want me to go to the army so that I could stay
providing free service in the special school and also because I was the
son of leprosy patients and this was a very heavy burden. (Blue)
I was so afraid of leaving there that I spent six years engaged until I
get married and could live outside the special school. I was very
afraid of the things in the world, afraid of what the people could say
about us because they were both children of lepers. (Green)
We were forbidden to leave; we could not go to parties or to the beach.
We could only stay in the special school and we were excluded from life
outside of it. (Brown)
The mention of the term leprosy is associated with isolation and
segregation suffered in the past by those who had the disease so that
leprosy currently refers to the social memory of exclusion 6.
The exclusion experienced by the leprosy patient spread and affected their
relatives who, even in the face of not having the disease, received the
negative impacts of their relatives. Currently, misinformation about
leprosy demonstrated by the patient and the family influences the
health-disease process, and it is up to both groups to engage in a mutual
involvement in the treatment in order to clarify doubts about leprosy,
which will provide an adequate social interaction.
Health practitioners, especially the nurse, must carry out educational
activities in order to disseminate information about the epidemiological
chain and treatment of leprosy, thus reducing the prejudice against those
with the disease. The adoption of such measures leads to clarification of
the population, favoring social integration, family life and adherence of
the patient to therapeutic measures7.
CONCLUSION
Results of this study point to the obstacles in the social relations
experienced by the relatives of ex-leprosy patients treated in the asylum
environment. Dysfunction in relationships was closely linked to the
presence of a person with leprosy in the family, marking their closest
members who, although healthy, were victims of social exclusion, stigma and
prejudice.
Difficulties in establishing cordial relations with society changed the
living condition of the collaborators of this study, as presented in the
thematic axes. Although there are new forms of treatment and cure, the lack
of adequate knowledge about leprosy influences the social interaction of
the patient and his/her relatives by carrying with them the scars of
prejudice experienced by leprosy patients in the past.
Knowing the repercussions of leprosy on family life, after a family member
is diagnosed, and given the social impact caused by leprosy nowadays, in
relation to the patient and his/her family, entails the responsibility of
health practitioners, especially nurses, to provide a comprehensive care to
patients, their families and the community, in order to reduce stigma and
increase adherence to treatment.
Because this is a qualitative research, with a small number of
participants, the results limit comparisons and prevent generalizations.
However, the relevance of this work is enhanced in that it broadens the
discussion on the theme, with a view to the development of complementary
studies.
REFERENCES
1.
Aquino CMF, Rocha EPAA, Guerra MCG, Coriolano MWL, Vasconcelos EMR,
Alencar EN. Peregrinação (Via Crucis) até o diagnóstico da hanseníase.
Rev enferm UERJ. 2015;23(2):185-90.
2.Pinheiro MGC, Miranda FAN, Simpson CA, Vitor AF, Lira ANBC. Limitações e
incapacidades físicas no pós-alta em hanseníase: uma revisão integrativa.
Rev baiana enferm. 2016;30(2):1-11.
3.Monte RS, Pereira MLD. Hanseníase: representações sociais de pessoas
acometidas. Rev RENE. 2015;16(6):863-71.
4. Videres ARN, Simpson CA, Mendes FRP, Oliveira RCC, Adário KDO, Pimenta
EF et al. Manifestations of stigma and prejudice informed by treated
lepers. Int Arch Med. 2016;9(47):1-10.
5.Schweickardt JC, Xerez LM. A hanseníase no Amazonas: política e
institucionalização de uma doença. Hist Cienc Saúde Manguinhos.
2015;22(4):1141-56.
6.Faria L, Santos LAC. A hanseníase e sua história no Brasil: a história de
um "flagelo nacional". Hist Cienc Saúde Manguinhos. 2015;22(4):1491-95.
7.Queiroz TA, Carvalho FPB, Simpson CA, Fernandes ACL, Figueirêdo DLA,
Knackfuss MI. Perfil clínico e epidemiológico de pacientes em reação
hansênica. Rev Gaúcha de Enferm. 2015;36(esp):185-91.
8. Lopes FN, Lana FCF. Participação popular no controle da hanseníase: um
desafio para o serviço
de saúde. Rev enferm UERJ. 2015; 23(2):235-40.
9.Meihy JCSB. Manual de História oral. 4ª ed. São Paulo: Edições Loyola;
2002.
10.
Bardin L. Análise de conteúdo. São Paulo: Edições 70/Livraria Martins
Fontes; 1979.
11.
Goffman E. Estigma: notas sobre a manipulação da identidade deteriorada. 4ª
ed. Rio de Janeiro: Editora Guanabara; 1988.
12.Silva RCC, Vieira MCA, Mistura C, Lira MOSC, Sarmento SS. Estigma e
preconceito: realidade de portadores de hanseníase em unidades prisionais. Rev pesqui cuid fundam. [Internet] 2014 [cited in mar 20 2016]; 6(2):493-506. Available at: http://www.seer.unirio.br/index.php/cuidadofundamental/article/view/2879/pdf_1231.
13.Leite SCC, Sampaio CA, Caldeira AP. "Como ferrugem em lata velha": o
discurso
do estigma de pacientes institucionalizados em decorrência da hanseníase.
Physis Rev Saúde Coletiva. 2015;25(1):121-38.
14. Garbin CAS, Garbin AJI, Carloni MEOG, Rovida TAS, MRJ. The stigma and
prejudice of leprosy: influence on the human condition. Rev Soc Bras Med
Trop. 2015;48( 2 ): 194-201.
15. Leite SCC, Caldeira AP. Oficinas terapêuticas para a reabilitação
psíquica de pacientes institucionalizados em decorrência da hanseníase.
Ciênc saúde coletiva. 2015;20(6):1835-42.
16. Santos KS, Fortuna CM, Santana FR, Gonçalves MFC, Marciano FM, Matumoto
S. Significado da hanseníase para pessoas que viveram o tratamento no
período sulfônico e da poliquimioterapia. Rev Latino-Am Enfermagem.
2015;23(4):620-7.
17. Araújo KL, Pena PGL, Freitas MCS. Sofrimento e preconceito: trajetórias
percorridas por nutricionistas obesas em busca do emagrecimento. Ciênc
saúde coletiva. 2015;20(9):2787-96.
18.Alcntara SC, Abreu DP, Farias AA. Pessoas em situação de rua: das
trajetórias de exclusão social aos processos emancipatórios de formação de
consciência, identidade e sentimento de pertença. Rev Colomb Psicol.
2015;24(1):129-43.