Note: (*) UM – Unit of meaning; (**)RU – Registration unit
RESEARCH ARTICLES
Nurses' symbolic construction of treatment for people living with HIV/AIDS
Denize Cristina de OliveiraI; Thelma SpindolaII; Antonio Marcos Tosoli GomesIII; Sergio Correa MarquesIV; Glaucia Alexandre FormozoV; Letícia de Araújo CamposVI
I
PhD in Nursing. Titular Professor at the Department of Nursing Fundamentals of the Faculty of Nursing at the State University of Rio de Janeiro. Brazil.
E-mail: dcouerj@gmail.com
II
PhD in Nursing. Associate Professor at the Department of Nursing Fundamentals of the Faculty of Nursing at the State University of Rio de Janeiro. Brazil.
E-mail: tspindola.uerj@gmail.com
III
PhD in Nursing. Titular Professor at the Department of Medical-Surgical Nursing of the Faculty of Nursing at the State University of Rio de Janeiro.
Brazil. E-mail: mtosoli@gmail.com
IV
PhD in Nursing. Adjunct Professor at the Department of Nursing Fundamentals of Faculty of Nursing at the State University of Rio de Janeiro. Brazil.
E-mail: scmarques@uol.com.br
V
PhD in Social Psychology. Adjunct Professor at the School of Nursing - Campus Macaé of the Federal University of Rio de Janeiro. Macaé, Rio de Janeiro,
Brazil. E-mail: glaucinhaenf@yahoo.com.br
VI
Masters in Nursing by the Faculty of Nursing at the State University of Rio de Janeiro. First Lieutenant of the Navy of Brazil. Rio de Janeiro, Brazil.
E-mail: leticiauffenf@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.13191
ABSTRACT
AIDS is present in different population groups in Brazil, determining socio-cognitive constructions as regards treatment. This qualitative study analyzed nurses' social representations of treatment for people living with HIV/AIDS by semi-structured interview of 20 nurses at a public university hospital in 2010 in Rio de Janeiro, and analysis of the transcripts for thematic content. There was a network of representations among the nurses in which treatment for people living with HIV/AIDS was recognized in its physical, psychosocial and relational dimensions, on the basis of categories that do not reduce to drug therapy, but include clinical and physical care, feelings, and social, relational and psychological aspects of treatment. Social representations of treatment play an important role in the care setting: they encompass the actions recognized by nurses to control AIDS, and thus participate in determining the care practices applied.
Keywords: Treatment; HIV/AIDS; social representation; nurse.
INTRODUCTION
The Human Immunodeficiency Virus (HIV) and Acquired Immune Deficiency Syndrome (AIDS) are widespread in all population groups in Brazil, with some social groups recognized as more socially vulnerable. The epidemiological profile indicates the occurrence of heterosexualization, feminization, rejuvenation and pauperization of the epidemic, with an increase of cases among groups with low education, women, young and black people1. However, all groups are vulnerable to HIV infection and susceptibility depends on social context and increases with higher sociocultural and economic exclusion levels2.
From its beginning until 2014, AIDS epidemic had 734,000 cases registered in Brazil what represents a prevalence rate of 0.4% of the general population. The highest concentration of cases lies among individuals between 25-39 years old of both sexes; 54.0% of cases among men and 50.3% among women. The detection rate in the country has shown stabilization in the past decade, with an average of 20.5 cases per 100,000 inhabitants, with the highest decreasing trend found in the Southeast (28.1%), passing from 26.0 to 18.7 cases per 100,000 inhabitants. Mortality rate passed from 6.1 deaths per 100,000 inhabitants in 2004 to 5.7 in 2013, representing a decrease of 6.6% in the Southeast and South. The states of Rio de Janeiro and Amazonas hold the 2nd and 3rd largest mortality rates in the country. Among all deaths by AIDS, 71.3% were men and 28.6% were women. There is an increase in survival associated with early1diagnosis of infection1,3.
The introduction of antiretroviral therapy (ART) reduced the mortality associated with HIV/AIDS, lowering the number of hospitalizations and occurrence of opportunistic infections, this way placing AIDS among chronical diseases1.
One of the results of the impact of ART in increasing expectancy and quality of life of people living with HIV/AIDS (PLWHA) was the establishment of a predominant clinical and medical focus of treatment, with actions aimed at the diagnosis, laboratory control of viral loads based solely on drugs and control of the transmission. Although the importance of these actions to reduce the epidemic is irrefutable, the social and psychological impact of the disease and the virus and actions for solving them were not prioritized in public policies combating the disease.
Technologies that make up the treatment of people living with HIV/AIDS are considered to be a modality of health care, configured as object of representations, since they are present in everyday conversations, triggering different positions of professionals and customers in face of it.
Faced with the problem of different conceptions of the treatment for PLWHA, the purpose of this article is to describe and analyze the social representations of the actions comprising the treatment of people living with HIV/AIDS among nurses.
THEORETICAL BACKGROUND
Care is essential in actions aimed at the promotion, maintenance and recovery of health, the core technology that nursing uses to fully assist the client. Clinical, psychological and social technologies guided by the expertise of the multidisciplinary team and supported by the organization of services and allocation of resources must be used in order to meet the needs of PLWHA4. While providing assistance to PLWHA, the nurse faces challenges of political, social, cultural, economic nature, as well as symbolic constructions involving the professional group, his origin group, the client and the family.
Caring for a PLWHA requires an integral view of the human being, which has specific demands, is fragile and deserves respect and attention. This care must be rescued in everyday relationships and in the thinking and doing nursing, with the use of technology and sensibility in personal and professional relations5.
Taking care of PLWHA is a challenge for health professionals due to the discriminatory and stigmatizing nature of the disease still present today, and the difficulties associated with the health system structure and working relations in this sector6.
Three dimensions of care provided by health professionals to assist PLWHA are notable. These are named cognitive, affective-relational and technical-instrumental dimensions and they are manifested since the revelation of the diagnosis and persist throughout the treatment until the terminal phase7. Furthermore, concepts of human and health needs are underlying health care representations, in the same way they remain underlying health practices in general8. Health care is seen as a working technology that is organized according to each historical period, taking roots in certain definitions of needs and aiming at specific work processes, besides it is part of different networks of representations that surround the disease, the sick person and its treatment and the coping with the disease9.
Considering the complexity and the strong symbolic aspect of the disease and the virus, as well as of the health care itself, this research was guided by the theory of social representations, conceived in Social Psychology. Notably, social representations are not created by a single individual but by social groups through communication and cooperation processes10. When created, representations "gain life in itself, circulate, meet, attract and repel each other and they give opportunity to the birth of new representations while old representations die"10:213.
The represented senses and contents differ within the same society and the same culture and this differentiation must be observed according to the way of thinking and understanding of this society. The markers of these differences are "the specificities of consensual universe and reified universe and the communication contexts in which these representations are constructed"10: 213.
While it is a form of knowledge of common sense and also a particular mode of technical and professional knowledge, the social representation is understood from the context in which it operates and its functionality in everyday social relations, "articulating emotional, mental and social elements, integrating cognition, language and communication to social relationships that affect the social representations and material, social and ideational reality on which they intervene"11:41.
METHODOLOGY
This is a study of descriptive and qualitative type in which data was collected in 2010 in a public university hospital in the city of Rio de Janeiro involving 20 nurses who cared for PLWH and working in the areas of infectious and parasitic diseases, internal medicine, pulmonology and general intensive care unit.
The choice of study participants was based on convenience and associated to the performance of professional activity accustomed to the object of research, and this way, nurses who took care of PLWHA in the abovementioned sectors were invited to participate. Those who agreed to participate answered a semi-structured interview and a socioeconomic and professional characterization questionnaire addressing the following variables: age, gender, monthly income, marital status, number of children, role in the team and time spent in work, type of vocational training, time spent in vocational training and time spent working with PLWHA.
Testimonies of nurses were analyzed by applying the technique of thematic-categorical content analysis with the following steps: pre-analysis, material exploration, treatment of results, inference and interpretation of results12,13.
The study was approved by an Ethics Committee with Opinion number 1575 and professionals signed a consent form. To preserve the anonymity, interviews received an identification number, I1, I2, I3… to the extent they happened.
RESULTS AND DISCUSSION
Characterization of respondents reveals that most are female (15/75%); aged between 35-44 years and some aged at 45 years or older (9/45%); living with a partner (13/65%); with children (13/65%); with a monthly income between R$ 3000.00 to 6000.00 (14/70%); most of them with post-graduation lato sensu (15/75%); working for over 10 years in nursing (19/95%); working for 11-20 years in the investigated hospital (12/60%); working for over 20 years in nursing function (10/50%) and for 15 years or more with PLWHA (11/55%).
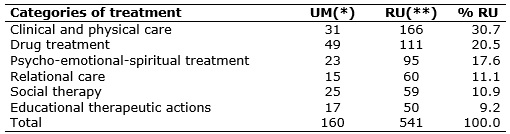
Content analysis resulted in 541 registration units (RU) distributed in 160 units of meaning. The aggregation of these units resulted in six categories presented in Table 1.
TABLE 1:
Categories, registration units and units of meaning of the treatment of PLWHA among the studied nurses. Rio de Janeiro, 2010.
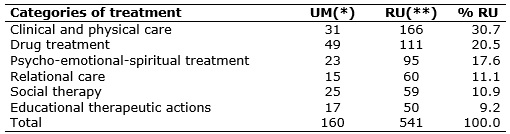
Note: (*) UM – Unit of meaning; (**)RU – Registration unit
The six categories defining the treatment of PLWHA for the studied nurses were: Clinical and physical care; Drug treatment; Psycho-emotional-spiritual treatment; Relational care; Social therapy and Educational therapeutic actions, described below.
Clinical and physical care
Clinical treatment of PLWHA has as one of its main components the monitoring of viral load which consists of the evaluation of the immune system through regular attendance at health service units for carrying out medical consultation for evaluation of laboratory tests. The RU below illustrates this observation:
It is important to explain the need to take exams regularly. (I12)
The patient's immune system is compromised due to the disease itself; a focus of infection can be absurdly fatal. (I17)
The lack of laboratorial monitoring and increased viral load may result in opportunistic infections in face of a weakened body defense system, as it is the case of HIV. HIV infection can be divided into four clinical phases: acute infection; asymptomatic phase, also known as clinical latency; initial or early symptomatic phase and aids14. Each of these stages involves specific clinical procedures equally important to the future prospects of PLWHA, and monitoring the immune system constitutes a prime indicator in their discrimination.
The incentive for practicing physical activities and nutritional counseling are also constituent elements of the clinical and physical treatment of PLWHA, besides recommendations for the adoption of a healthy lifestyle, avoiding alcohol and other drugs that affect the CD4 and viral load besides the risks of interaction with antiretroviral (ARV)14.
Drug treatment
The focus of health professionals treating PLWHA falls almost exclusively on drugs, this way causing the adherence to become the central point of pathology outcome, as well as their difficulties.
Thus, adherence to drug treatment and diagnosis concealment strategies are challenges faced by health professionals, putting drug therapy in evidence in the context of psycho-social construction of illness and of the treatment itself.
Our big problem is medication adherence. (I4)
These patients, who sometimes have to take about 20 pills a day, when they stop feeling things, they stop doing everything. They have to be feeling something to take medicine, when the feeling ceases, they quit the remedy. They fail to take it, because they do not want those at home to know, they pluck the label to avoid the family to know. (I6)
The analysis of determinants of treatment adherence is complex as it involves a web of factors that contribute to its disruption or its abandonment. Participants in this study identified some factors involved in noncompliance, factors related to the presentation of medicines, the treated person, the disease, the health service and the economic and social support.
These findings were also found in other studies15-19 and show the importance of acting as a team along with PLWHA. A study found that some periods are more favorable for abandoning the treatment, as the initial phase, and identified associated factors such as lack of a social network offering support, socioeconomic difficulties and difficulties related to the use of antiretroviral drugs and characteristics related to lifestyle such as use drugs abuse and psychiatric history15.
The absence of signs or symptoms has been reported as associated with abandoning treatment, as well as the existence of individuals that do not use the medication and do not disclose this fact to the health team, revealing the variety of behaviors triggered by the disease and the psychosocial context.
The existence of difficulties and reasons for adherence to ART was analyzed noting that the reconciliation between requirements of treatment and daily activities, representations of HIV and ART, and those inherent to the complexity of the treatment are factors that hinder adherence. The memory of AIDS symptoms, perception of increased survival and bonding with members of the social network of PLWHA are described as facilitators to adherence to treatment 16.
Psycho-emotional-spiritual treatment
Fear of death is reported as a persistent feeling in PLWHA that produces stress and psychic manifestations, as well as leads to search for support in divine entities. Self and peer discrimination are responsible for the suffering of these individuals and their families, implying the need for professional actions to support their coping.
Pay attention to the psychological side. If the person is psychologically devastated, let us at least keep the balance. (I18)
I try, in one way or another, promote spiritual care, I already experienced this with a very dear person, I know the importance of this spiritual part for the patient. (I17)
Reducing the impact of stigma and discrimination related to HIV/AIDS and improve care is one goal of the health sector. In order to reduce the suffering and emotional upheaval, the following strategies were cited by the individuals as useful in overcoming and coping with the disease: improvement of self-esteem, respect for individuality and privacy, incentive for development of religious practices and actions reinforcing spirituality.
There is evidence that religion and spirituality are associated with psychological well-being and are considered fundamental for people in times of suffering and serious disease, resulting in strength to endure hardship20.
Assistance with biopsychosocial and spiritual approach to human being can allow expanding care practices from strictly physical toward a more integral dimension. This care practice should be directed to the mind-body-spirit, not just to the virus, the disease or the patient's body, reflecting the reciprocity of human relations, essential to a comprehensive care perspective directed to PLWHA.
The relational care
The relational dimension of care highlighted by the nurses is expressed in the dynamics of relations between PLWHA and health professionals, where involved actors are able to influence the multiple interactions present in the dynamics of care. The success of combating HIV/AIDS depends on several factors, including the welcoming and active listening of the patient by the multidisciplinary team, the link with health professionals, staff and health service, in addition to broader social support7,14,21,22.
The interaction, welcoming attitude, attention and support are key actions that result in a relationship of trust between professional and client, as pointed by nurses.
And medication is not enough, it is necessary more than just give the bath, you must also interact with him/her at that time. (I13).
They show a great deal confidence in us ... you already know the patient, know all the implications, even because of this relationship of trust. (I3)
When care includes attention and physical presence, the caregiver no longer performs procedures on someone, but he performs an integrated action with involvement, dedication and responsibility, providing growth for those involved and mutual respect in the relation of care23-25. The welcoming attitude allows for introduction of an empathic relationship in attendance, enabling the creation of a dialogic space and participation in the treatment 26.
The complexity of treating PLWHA requires a care essentially relational, considering its technical and psychosocial elements and based on the symmetry of the relationship between people, valuing and recognizing the patient's as well as the professional' singularities22,27.
Technologies in health care should incorporate the notion of light technologies that are expressed as the process of production of communication, of relationships and links that lead the user to meet with the need of health actions28.
Social therapy
AIDS is a recognized phenomenon of social nature accompanied by segregation processes based on socially constructed stigmas that are closely linked to social representations of the disease29. This aspect of the disease brings suffering and compromises the quality of life of PLWHA, imposing limitations on personal, professional and everyday relationships30.
Economic difficulties, specificities of the different groups affected by the disease and the virus, and the need for social support are recognized by respondents as care modalities.
The financial side as well, because, how will he practice prevention and how will he maintain normal body structures if he has not even what to eat? He sleeps poorly, eats poorly, how will he practice prevention? In the other hand, with a better income ... (I13)
People who have more years of schooling may be more difficult when approached by professionals. Others, who come from an underprivileged social class, may be more victimized by prejudice. (I1)
Work and economic conditions are key issues in the lives of PLWHA and can interfere in the treatment and quality of life. The PLWHA often find it difficult to maintain productivity at work, because time off from work for frequent visits to the health service is required, the side effects of ART and the deterioration of his framework31. The difficulties to maintain employment and recognize themselves as socially productive individuals are confirmed as part of the social limitations associated with the disease, implying the need for specialized support for solving them.
Another factor influencing the treatment of PLWHA is the level of education, acknowledging that individuals with low education levels tend to suffer greater prejudice and face greater difficulties to receive emotional support32. The support and social backing are fundamental for the quality of life of PLWHA because they contribute to the adaptation by managing emotions, affective and cognitive orientation and retro information, reducing isolation and increasing life satisfaction33.
Educational therapeutic actions
The education in health is recognized as indispensable for the prevention of infection, to control the disease, retrieve and restore self-care health in the context of HIV/AIDS. This is a care aimed at the clarification and guidance, developed at the institutional daily life, and allows for a dialogic space and interaction between clients and health professionals.
Education is understood as a form of care which should be developed through dialogue education aiming to enable the client to promote his own care, and aiming at the strengthening of autonomy34. Educational care was found in this study as part of the set of essential actions to combat the disease.
In our practice, for being a health professional, we worry a lot and we try to advise in every opportunity on prevention, thinking even in terms of the big picture of the disease as a whole, and in the spread of the disease in the world. (I12)
Try to get some more knowledge, find out what he knows about the disease, how to care, how to feed, to see if he gets better and does not take more opportunistic infections. (I13)
The speeches show that care should not be automatic or full of protocols, but it is necessary to know the individual and the collective experiences of individuals and their moment in life35. Prevention of infection by the virus and the care for the established disease are recognized as objects of educational practices.
The practice of education in health constitutes one of the facets of care in HIV/AIDS and it is indispensable for prevention and quality of life of individuals with or without the virus. It is necessary, however, that this care is suited to the socio-cultural reality of the customers, allowing for participation and self-responsibility of individuals in the process.
CONCLUSION
I face of technical-scientific and pharmacological developments of ART, the survival of PLWHA has increased, causing a syndrome represented as death to become one with features of chronicity. Although incurable, AIDS has effective possibilities of control, bringing new challenges for health professionals.
The contents of the social representation of the treatment of PLWHA have suffered transformations, accompanying the evolution of the disease and incorporating virus, besides clinical and physical care and drug treatment, relational care, educational activities, the psycho-emotional-spiritual perspective and social therapy. This representation exceeded the biological nature of treatment and reached a nature more related to the human person, considering that HIV/AIDS causes many psychological, spiritual, social, professional and familiar consequences, embracing the human being in its entirety and reflecting on various aspects of life.
A range of involved actions in different treatment modalities was found in this study, and therefore a range of care of PLWHA not restricted to clinical and drug treatment, but involving a set of physical, psychological, spiritual, social, educational, familiar and relational needs. A network of representations associated with the treatment of PVHA was observed. This network points to actions recognized as part of disease control and turns to the extent of quality of life and the future of PVHA and of society itself.
The present study has as limitations the amount of professionals studied and the time elapsed since its realization. However considering the national and world scenario of AIDS, these findings certainly are relevant for research in nursing and care of PLWHA.
REFERENCES
1.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Departamento de Aids e Hepatites Virais. Boletim Epidemiológico DST/Aids 2014. Brasília (DF): Ministério da Saúde; 2014. [citado em 10 jul 2015]. Disponível em:
2.Navarro AMA, Bezerra VP, Oliveira DA, Moreira MASP, Alves MSCF, Gurgel SN. Social Representations of the HIV/AIDS: perception of the primary health care professionals. R pesq.: cuid fundam. [online] 2011; (Supl): 92-9.
3.Hall R, Ravasi G, Kuchenbecker R, Greco D, Simão M. O acesso universal ao tratamento antirretroviral no Brasil. Tempus actas de saúde colet. 2010; 4: 53-65.
4.Souza S. Os discursos de adesão ao tratamento de AIDS – uma reflexão ética. Rev Bioethikos - Centro Universitário São Camilo. 2011; 5: 98-106.
5.Luz PM, Miranda KCL. As bases filosóficas e históricas do cuidado e a convocação de parceiros sexuais em HIV/aids como forma de cuidar. Ciênc saúde coletiva. 2010; 15: 1143-8.
6.Formozo GA, Oliveira DC. Representações sociais do cuidado prestado aos pacientes soropositivos ao HIV. Rev Bras Enferm. 2010; 63: 230-7.
7.Souza CSO, Silva AL. O cuidado a pessoas com HIV/aids na perspectiva de profissionais de saúde. Rev esc enferm USP. 2013; 47: 907-14.
8.Oliveira DC, Gomes AMT, Pontes APM, Costa CPM. Construção de um paradigma de cuidado de enfermagem pautado nas necessidades humanas e de saúde. Esc Anna Nery. 2011; 15: 838-44.
9.Gonçalves RBM. Práticas de saúde: processos de trabalho e necessidades. São Paulo: CEFOR; 1992.
10.Moscovici S. Representações sociais: investigações em psicologia social. Petrópolis(RJ): Vozes; 2003.
11.Jodelet D. organizadora. As Representações Sociais. Rio de Janeiro: EdUERJ; 2001.
12.Bardin L. Análise de Conteúdo. Lisboa(Pt): Ed. 70; 2007.
13.Oliveira DC. Análise de Conteúdo Temática: uma proposta de sistematização. Rev enferm UERJ. 2008; 16: 569-76.
14.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Departamento de Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para manejo da infecção pelo HIV em adultos. Brasília (DF): Ministério da Saúde; 2013. [citado em 10 jul 2015]. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_manejo_hiv_adultos.pdf
15.Schilkowsky LB, Portela MC, Sá MC. Fatores associados ao abandono de acompanhamento ambulatorial em um serviço de assistência especializada em HIV/aids na cidade do Rio de Janeiro, RJ. Rev bras epidemiol. 2011; 14: 187-97.
16.Santos WJ, Drumond EF, Gomes AS, Corrêa CM, Freitas MIF. Barreiras e aspectos facilitadores da adesão à terapia antirretroviral em Belo-Horizonte – MG. Rev Bras Enferm. 2011; 64: 1028-37.
17.Beyene KA, Gedif T, Gebre-Marian T, Engidawork E. Highly active antiretroviral therapy adherence and its determinants in selected hospitals from south and central Ethiopia. Pharmacoepidemiology And Drug Safety. 2009; 18:1007-15.
18.Roura M, Busza J, Wringe A, Mbata D, Urassa M, Zaba B. Barriers to Sustaining Antiretroviral Treatment in Kisesa, Tanzania: A Follow-Up Study to Understand Attrition from the Antiretroviral Program AIDS. Patient care and STDs. 2009; 23: 203-10.
19.Bonolo PF, Machado CJ, Cesar CC, Ceccato MGB, Guimaraes MDC. Vulnerability and non-adherence to antiretroviral therapy among HIV patients, Minas Gerais State, Brazil. Cad Saúde Pública. 2008; 24: 2603-13.
20.Fleck MPA, Borges ZN, Bolognesi G, Rocha NS. Desenvolvimento do WHOQOL módulo espiritualidade, religiosidade e crenças pessoais. Rev Saude Publica. 2003; 37: 446-55.
21.Neves CLR, Amorim WM, Moraes NA, Leite JL. The nursing care of the client with hiv/aids in a university hospital in the 1980's. R pesq: cuid fundam. 2009; 1: 299-316
22.Monteiro JFA, Figueiredo MAC. Vivência profissional: subsídios à atuação em HIV/AIDS. Paidéia. 2009; 19: 67-76.
23.Ferreira M A. O corpo no cuidado de enfermagem: representações de clientes hospitalizados [tese de doutorado]. Rio de Janeiro: Universidade Federal do Rio de Janeiro; 1999.
24.Waldow VR. Cuidado humano: o resgate necessário. 2ª ed. Porto Alegre (RS): Sagra D.C. Luzzatto; 1999.
25.Barcelos LMS, Alvim NAT. Atenção e presença física: dimensões expressivas e a prática dialógica do cuidado de enfermagem na perspectiva do cliente hospitalizado. Rev Bras Enferm. 2006; 59: 25-9.
26.Silva NEK, Oliveira LA, Figueiredo WS, Landroni MAS, Waldman CCS, Ayres JRCM. Limites do trabalho multiprofissional: estudo de caso dos centros de referência para DST/AIDS. Rev Saude Publica. 2002; 36: 108-16.
27.Santos EI, Gomes AMT, Oliveira DC, Santo CCE. Entre sofrimento e prazer – a vulnerabilidade para enfermeiros nas relações interpessoais com paciente com HIV/AIDS. Rev enferm UERJ. 2013; 21: 9-15.
28.Merhy EE, Franco TB. Por uma composição técnica do trabalho em saúde centrada no campo relacional e nas tecnologias leves: apontando mudanças para os modelos tecno-assistenciais. Saúde debate. 2003; 27: 316-23.
29.Malbergier A. AIDS e psiquiatria: um guia para os profissionais de saúde. Rio de Janeiro: Revinter; 2000.
30.Sousa MMO. SIDA: e a vida continua. Lisboa (Pt): Associação Portuguesa de Enfermeiros; 2001.
31.Tunala LG. Fontes cotidianas de estresse entre mulheres portadoras de HIV Rev Saude Publica. 2002; 36: 24-31.
32.Seidl EMF, Zannon CMLC, Troccoli BT. Pessoas Vivendo com HIV/AIDS: Enfrentamento, suporte social e qualidade de vida. Psicol Reflex Crit. 2005; 18: 188-95.
33.Resende MC, Bones VM, Souza IS, Guimaraes NK. Rede de relações sociais e satisfação com a vida de adultos e idosos. Psicol Am Lat. [Internet]. 2006; 5: 0-0 [citado em 24 set 2014]. Disponível em: http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1870-350X2006000100015&lng=pt&nrm=iso .
34.Alves IC, Padilha MICS, Mancia JR. A equipe de enfermagem e o exercício do cuidado a clientes portadores de HIV/AIDS. Rev enferm UERJ. 2004; 12: 133-9.
35.Paiva V, Latorre MR, Gravato N, Lacerda R. Sexualidade de mulheres vivendo com HIV/AIDS em São Paulo. Cad Saúde Pública. 2002; 18: 1609-20.