ORIGINAL RESEARCH
Analysis of hospital care of maternal deaths: critical reflection
Pâmela Yuri SaitoI; Neuma Zamariano FanaiaTeixeiraII; Janete Tamami Tomiyoshi NakagawaIII
I
Nurse, graduated from the Nursing School of the Federal University of Mato
Grosso. Brazil.E-mail: pysaito@live.com
II
Obstetric Nurse, PhD in Science, Professor of the Federal University of
Mato Grosso. Brazil.E-mail: neuma.zamariano@gmail.com
III
Obstetric Nurse, PhD in Science, Professor of the Federal University of
Mato Grosso. Brazil.E-mail: tominaka2003@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.12530
ABSTRACT
Objective: to examine hospital care provided to pregnant women who died in Cuiaba, Mato Grosso. Method: this cross-sectional, quantitative, descriptive study was conducted at the hospitals where the deaths occurred with a study population of 14 women resident in the city of Cuiaba, who died between 2008 and 2010. Data were sourced from Ministry of Health maternal death review reports. The variables of interest for the study were collected directed using a questionnaire of open and closed questions. Results: it was established that 14 deaths occurred during this period, 64.3% of them resulting from obstetric causes and, of these, 88% were probably preventable. The main causes of death were infections, hypertension and hemorrhagic syndromes. Conclusion: maternal mortality in the city is strongly associated with social and care-related factors.
Keywords: Maternal mortality; maternal death; pregnancy; hospital care.
INTRODUCTION
The challenge to reduce by 75% the global Maternal Mortality Ratio (MMR) in 15 years, established in the United Nations Millennium Development Goals (MDG)1, is a goal that requires major efforts from developing countries, especially those that have a high number, such as India and Nigeria, which account for 19% (56,000 deaths) and 14% (40,000 deaths), respectively, of total maternal deaths2,3.
Brazil had position below the Millennium goal; in the past 18 years, it has reduced 52%, with an average annual rate of decrease of 4%, when the ideal is 5.5% to achieve the target established in the MDG4. To achieve this goal, it is necessary much effort and more intensive measures by the State so that the managers of each of its municipalities are committed to reducing that rate by creating specific actions for improving obstetric care.
The Mato Grosso (MT) state presented a MMR of 86.97 deaths per 100,000 live births (LB), followed by 76.29 and 71.68 per 100,000 LB in the years 2008 to 2010, respectively5, ratio much higher than 20 / 100,000 LB, defined as acceptable by the World Health Organization (WHO)4. In the face of high rates in the state, this study aimed to analyze the hospital care provided to pregnant women who died in Cuiaba, capital of Mato Grosso state.
LITERATURE REVIEW
Review studies on the subject are unanimous in considering the maternal death as a good indicator of the social reality, as it is inversely related to the human development degree6,7. The contrast between the countries with the best and worst rates is well marked, with MMR of 3 / 100,000 LB in Ireland to 1,200 / 100,000 LB in Afghanistan4.
In Brazil, it is visible the decrease of the MMR in the last 3 decades. In the 80s, the national rate was approximately 150 per 100,000 LB, with a higher concentration in the Northeast region, which had a rate higher than 200 per 100,000 LB. In the 90s, there were approximately 120 maternal deaths per 100,000 LB and in 2005, there was a significant drop, reaching 64 / 100.00 LB in 2005 and 58 / 100,000 LB in 20088.
A major study has identified a decline in 15 Brazilian capitals, with a MM Rof 54.3, with a variation of 43 to 73.2 per 100,000 LB in the South and Northeast regions, respectively 9and revealed the existence of different Brazilian realities, reflecting the degree of development of each region and the health policies adopted by managers, as occurred in the city of Juiz de Fora, which has adopted strategies to reduce maternal mortality through measures to decrease the cesarean section rate, deploying the Humanized Care Model for Birth10.
Despite the different realities of Brazil, a study highlights the social vulnerability of women who died, because their low social condition is combined with the lack of access to good health services7.
Researches have shown that black women have a much higher risk of death than other races/colors6. This was confirmed in a study conducted in the state of Mato Grosso, which revealed that 63% of maternal deaths (MD) occurred among black women, whose proportion of deaths due to failure in health care can be considered evidence of differences between ethnic and racial groups, when taking by reference the conditions of access to health services11.
Most studies have found that maternal deaths are proportionately greater in extreme ages, that is, in the teenage phase or over 40 years old 6,7. These studies have found that women with low education in developing countries are more at risk of death due to the difficulty of access to health services12. The North and Northeast regions have the highest rates, however, deaths in these regions are under-reported and under-informed, which impairs the quality of information9.
There is prevalence of maternal deaths from hypertensive disorders, bleeding and infection, which are classified as preventable deaths. However, whereas in developing countries most deaths are due to direct obstetric causes, in some developed countries the deaths are consequences of cesarean section and anesthesia7.
METHODOLOGY
This is a descriptive, retrospective study with a quantitative approach, whose response variable (cases of deaths) and exposure variable (care data of the victims) were simultaneously investigated in research.
The study population includes all deaths of women who lived in Cuiaba, a total of 14 cases classified as MD by the Deaths and Births Management of Municipal Health Secretariat (MHS) in the period from 2008 to 2010.
Inclusion criteria were women who died due to obstetric causes (direct and indirect) living in Cuiaba and who were assisted in any health institution in the municipality under study.
The study variables were: sociodemographic characteristics of women, obstetric history, co-morbidities or pre-existing disease, cause of death recorded on the death certificate (DO), childbirth and postpartum and hospital care data.
Data collection occurred in September and October 2011. The data sources were the DO and the maternal death investigation records of the Ministry of Health (MOH), which capture data recorded in clinical records, in forms of interview with health professionals and with the victim's family.
The data collection was done through the analysis of these documents, extracting the variables of interest for the study from the data source. For this, authors used an electronic questionnaire with closed and open questions, developed in the EPI INFO 3.5.2program.
The collected data were entered and stored in the program database, which allowed the statistical analysis of data. Authors used descriptive statistics with measurements of central tendency and dispersion and the absolute and relative frequency of responses, with the aid of EPI INFO 3.5.2 program and analysis was presented in tables and figure, driven by the objective of the study.
After organizing and compiling data, each case was discussed and analyzed in detail, seeking to highlight the difficulties and failures of the care process that led the woman to the unfavorable outcome, presented as tables and figures, summarizing the main categories of study: sociodemographic characteristics of women, overview of health care conditions provided and data on the clinical condition of the victims.
The research project was evaluated by the Research Ethics Committee (REC) of the University Hospital Júlio Müller (HUJM), meeting the National Health Council Resolution No. 196/96, and obtained approval for its development through the opinion No. 883/2010. To preserve the anonymity and secrecy, the case studies were identified with the letter S, followed by an ordinal number that corresponds to the sequence in which the maternal deaths were analyzed, and according to the year in which the death occurred.
RESULTS AND DISCUSSION
The study identified 14 maternal deaths from 2008 to 2010 in the city under study.
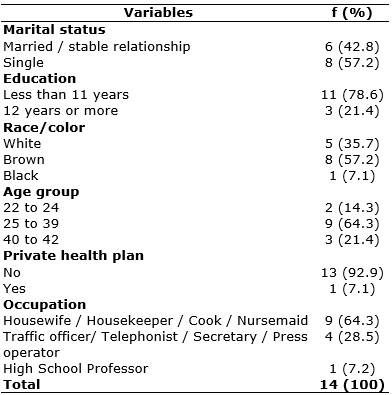
The analyzed sociodemographic variables are specified in Table 1.
TABLE 1:
Sociodemographic characteristics of female maternal deaths. Cuiabá / MT,
Brazil, 2008-2010. (N = 14)
It is observed that women were mostly single, Afro-descendants (brown and black), had low level of education and professional activity of low pay, as shown in Table 1. Only one of them had a profession with higher qualification, and she was the only one served by private health plan, whose cause of death was a pre-existing intestinal neoplasia, in full treatment with chemotherapy (S2).
The others were served by the Unified Health System (SUS)network services, whose assistance in some localities is precarious in structural, technical and human components, because, as shown by the literature, it has resulted in overcrowding of hospitals, difficulty of access to health services, lack of professional qualification in care, delay in diagnosis and therefore in the appropriate treatment6.
Added to this, in the studied reality, the SUS network essentially serves the population with low social conditions, thus enhancing the risk of life. A review study shows that the most vulnerable population to this event presents social and economic characteristics similar to those of victims 6, however, the authors pointed out that developing countries that have adopted public policies involved in the process of improving the health system, as Chile and Cuba, presented MMR similar to developed countries6,7.
Regarding age, the minimum was 22 years and the maximum was 42 years. The mode was 27 years, the median was 32 years and the mean was 31.8 years with standard deviation (SD) of 6.47. The literature suggests that the age at its extremes - less than 15 years old and more than 35 years old - is one of the pregnancy risk factors, especially when associated with other social and health conditions that are also unfavorable to pregnancy 13. It was found that 78.6% of deaths analyzed in the study occurred in women aged within the lowest obstetric risk, which is important and deserves further observation as it is the lowest risk group.
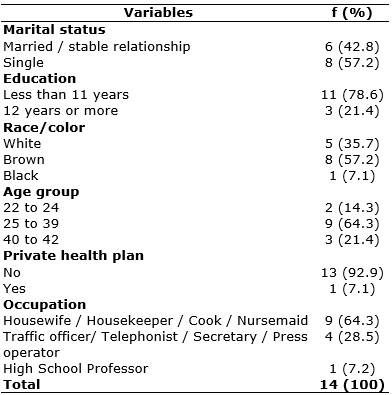
The underlying and the immediate cause of each death are listed in Figure 1.
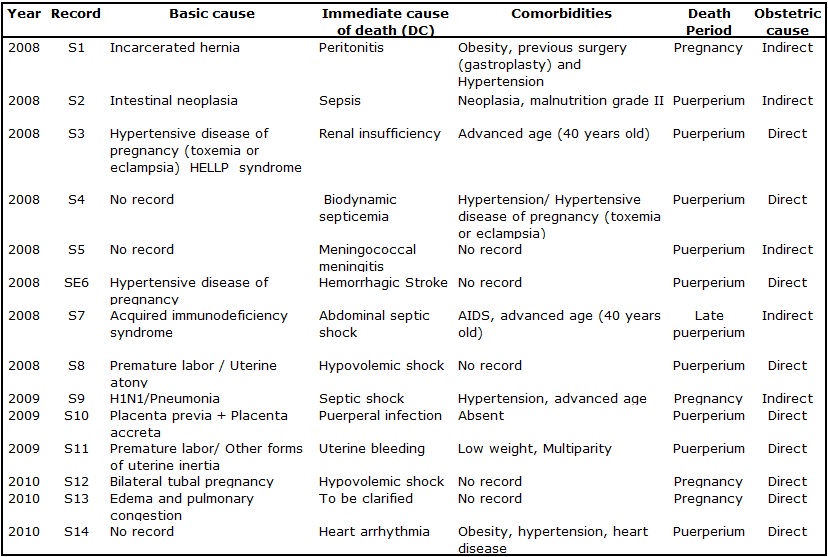
FIGURE 1:
Maternal clinical and obstetrical data and death causes. Cuiaba/MT, Brazil,
2008-2010
Of the total of 9 (100%) deaths from direct obstetric causes, 5 (55.5%) had no other comorbidities or clinical risk factors and 8 (88%) were classified as probably preventable, as shown by the data in Figure 1 and Table 2, respectively. This agrees with the MOH, which estimates that 90% of these occurrences are considered preventable13and are those that maintain the high levels of MD10. The health care conditions for the studied women are specified in Table 2.
TABLE 2:
Distribution of health care conditions of maternal deaths. Cuiaba/MT,
Brazil, 2008-2010.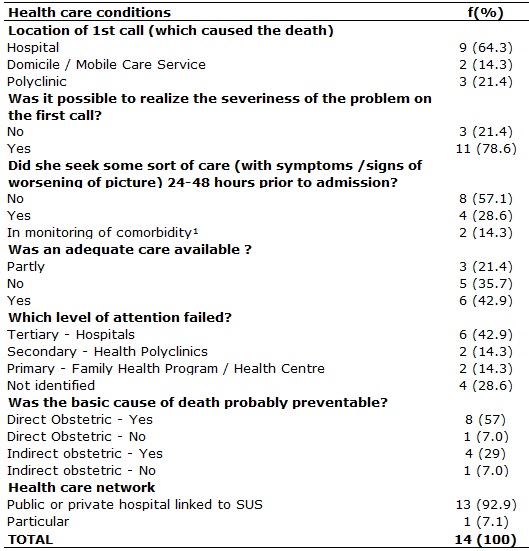
It was found that structural and technical deficiencies were co-decisive in some situations, as observed in the care of pregnant women in the emergency room with symptoms of peritoneal irritation, whose main barrier was the non-investigation of a pregnancy in the first call, eliminating the possibility of identifying an ectopic pregnancy (S12).
From the analyzed cases, researchers concluded that the deaths from hypertensive syndrome could have been prevented by identifying vulnerabilities and risks during pregnancy (S3, S6), as illustrated by the data in Figure 1. Prenatal care is the best time to detect possible complications, abnormalities and disease prevention related to pregnancy, especially the increase in blood pressure levels. However, a study showed that consultations are fast, causing signs and symptoms go unnoticed and inhibiting the woman to ask her questions and complaints regarding pregnancy14. According to the literature, 15% of pregnancies are characterized as high risk12, and early detection of changes is decisive for the maintenance of these women's lives.
Usually, IN the studied reality, patients are discharged from prenatal at their most critical moment, around the eighth month - when pregnancy conditions such as hypertension, diabetes are developed or worsened - leaving them with lack of knowledge as for which service they should seek in case of a complication or at delivery. In addition, it is recommended that from the 36th week, the consultation becomes weekly13. It is possible to verify the importance of this recommendation by analyzing the data. Study on neonatal mortality conducted in the city found that the precariousness of prenatal care has contributed in some way to the occurrence of neonatal deaths, as 70% of them occurred in infants of low birth weight15.
In the study, two deaths (S13, S14) shown in Figure 1 occurred suddenly, apparently related to cardiac and circulatory problems without previous clinical manifestation, but that could have been diagnosed during prenatal care.
It was found that among the deaths from indirect causes, the delay in recognizing the severity were the most common factors. In one of the cases, the underlying cause was elucidated only after the autopsy. Most likely, the aggravation would have been avoided if the gravity thereof (S1) had been identified in the first call. The data of this case are shown in Figure 1.
It is noteworthy that the analyzed cases show the complexity and the difficulty of making an accurate diagnosis, as several factors interact and obscure the correct diagnosis. For example, a pregnant woman (S1) sought hospital care complaining of general malaise and vomiting and returned to home with medication to alleviate the symptoms, very common in pregnancy. After 3 days, having come back to hospital, she had already presented a sepsis frame, whose progression to death occurred in less than a week. The cause of death was only informed after the autopsy, which identified an incarcerated hernia, responsible for the sepsis frame.
It may be identified, in this and in other cases, barriers at different times of the care process. However, it stresses the importance of valuing the clinical history, as in the case of the said pregnant (S1), who had undergone abdominal surgery (gastroplasty) before pregnancy, and that information had not been recorded in the hospital record and probably was not associated by professionals during clinical investigation.
Also, regarding the indirect obstetric causes, a possible failure of the health system resoluteness was observed in one case (S5), for the admission to specialized services and intensive care unit (ICU) was not assured. The basic cause of death was declared as meningitis. The mother had sought a basic health unit next to her neighborhood when the first symptoms appeared, but at that time, the neurological status, still being installed, was not recognized. After the worsening of the symptoms, she sought care in the secondary care service, but there was a delay in the regulation of the bed in a specialized service.
In Brazil, mortality from indirect obstetric causes increased 33% from 1990 to 2000 and has maintained the same level in the following years 13. In this study, the examined cases highlighted the need for ongoing research of deaths of women of childbearing age, because many of them have been hospitalized in early pregnancy, with bleeding and infection resulting from unsafe and undeclared abortion, which leads to underreporting of such deaths.
From the data in Figure 1, authors analyzed the presence of comorbidities, and 5 (35.7%) of women had a comorbidity or pre-existing condition that contributed to the death (S1, S2, S4, S7, S14). Among the various situations of comorbidities, it is essential to mention the occurrence of pregnancy in the course of a cancer treatment, with assistance of a specialist professional of the private system (S2). Thus, it is observed that women must be examined in their multiple dimensions, in their entirety, without reducing them to a medical specialty, disregarding reproductive life and the need to prevent pregnancies in women being treated for cancer.
Although the data have been recorded in technical and objective way, the scenario of the family despair transpired in the notes of records of deaths. Therefore, in analyzing such descriptions, researchers detected episodes in which some women and their families sought various health services in the municipality, mostly in times that are typical of emergency situations, which evidences a call for help from family members to health services (S1, S9, S12).
These data are not presented in the study, but it was possible to recognize the context of the assistance provided in the transcripts made from the clinical records, as the analyzed cases were quite complex, involving other clinical conditions that obscured the main cause of the problem, besides individual, social and structural factors of care that certainly made the diagnostic elucidation difficult at the exact moment. They also revealed the technical difficulty of the health team to satisfactorily respond to complex situations, as these require from professionals more than technical competence, but the ability to understand the reality of life and health of an extremely poor population that depends exclusively on SUS.
The site of the first call to the cause that led to the death was directly the hospital in 9 (64.3%) cases, as shown in Table 2. This data shows that the symptoms / early signs were recognized by family and deserved a more complex care (S1, S2, S3, S5, S6, S7, S8, S10, S11). In 4 cases, the reason for hospitalization was not what caused death, which often generates a feeling of revolt in the victims' families (S1,S8,S10,S11).
It was found in 2 (14.3%) cases that the family called the Mobile Emergency Service, but the death occurred before the arrival of the service team; one occurred in the countryside (S13, S14). These data are given in Table 2. Studies performed in India concluded that the delay in the recognition of complications is a major factor for the occurrence of the worst outcome 16, especially in developing countries.
Table 2 also shows that 3 (21.4%) women sought the polyclinic, and two of them were referred to the tertiary care service because they required special care. To illustrate, we present the case of pregnant woman whose underlying cause of death was respiratory infection - with initial signs and symptoms similar to cold, which made it impossible to establish the life support when presenting the worsening of the respiratory condition (S9). The second case was an ectopic pregnancy, in which the family denied this possibility, as they had at hand a pregnancy test with a negative result. The health team only treated the symptom of abdominal pain presented by the woman, not being able to avoid death before the hemorrhagic shock was installed (S12). In the third case, the mother sought the polyclinic in the seventh day after delivery, with fever and abdominal pain, was transferred to a more complex service, and died on the 12th postoperative day from septicemia. It is observed that in this case, the search for the hospital care occurred belatedly (S4).
Authors investigated whether there was demand for a health service within the 24-48 hours prior to their hospitalization, according to data presented in Table 2. Of the 14 cases, 4 (28.6%) sought the health service with severe clinical picture (S9, S12, S13, S14) and 8 (57.1%) did not seek any kind of health care within that period (S1, S3, S4, S5, S6, S8, S10, S11). Two pregnant women were in medical care due to pre-existing serious illness (S2,S7).
Regarding the service, researchers verified whether there were conditions for diagnosis and treatment, availability of equipment and health staff with necessary skills and the efficiency of the reference and counter reference system. Of these, 42.9% provided adequate care in the majority of cases (S1, S3, S4, S5, S7, S13) and 21.4% of cases received partially satisfactory service, factors that contributed to death ( S9, S12, S14), as shown in Table 2.
It is worth mentioning that attendances were essentially held in a common maternity and three in tertiary reference hospitals of the SUS network of the municipality, whose installation of a minimum structure is required, as determined by the National Health Surveillance Agency in items related to physical space, materials and equipment of maternities of health care facilities, as well as training of health professionals necessary for a good care.
It was found that cesarean sections were more frequent, so it is recommended to reduce the rate of unnecessary cesarean sections. Although the indication of operative delivery occurs mostly in emergency cases, it increases the risk of death during post-partum, because a study shows that there are a significant number of maternal deaths directly related to the surgery / anesthesia, such as post-cesarean infections, anesthetic complications, hemorrhage and amniotic fluidembolism6.
CONCLUSION
Although noticing a reduction in the number of deaths during the studied three years, the study showed that maternal mortality in that city is strongly associated with social factors and revealed the vulnerability of the socially disadvantaged group, which, in most cases is a decisive factor for the occurrence of death. Among the direct obstetric causes, there were infections, hypertensive disorders and hemorrhagic syndromes, and the occurrence of deaths almost exclusively in the health services linked to SUS.
Although all women in the study had had access to some kind of health care, it does not mean that it was enough. However, maternal mortality stems from a series of unsuccessful factors that goes beyond the health care provided to the woman. This process includes the living conditions of women, access to health, sociodemographic characteristics, the cultural level of the people next to them, the family and social support, and many other peculiarities.
It is necessary to overcome the difficulties and failures of health services at all levels of care of the current health system, and it is necessary to involve the subjects, so that health professionals and managers are also feel responsible for the assistance provided.
Professionals should give for the assisted population the necessary tools so that they can recognize abnormalities, clarify doubts and anxieties, and do not remain submissive if their main complaint is not settled.
The main limitations of this study were the lack of records of the care provided to women during their stay in the health services and errors in the completion of death certificates. To overcome this problem, it is necessary to provide training for professionals in the correct filling of forms / records and DCs, stressing the importance of this information for vital statistics, and that the professionals themselves start to claim for a technical training and do not hide the facts for fear of punishment.
REFERENCES
1.Programa das Nações Unidas para o Desenvolvimento [site de internet]. Objetivos de Desenvolvimento do Milênio (ODM). [cited 2015 Oct 12] Available from: http://www.pnud.org.br/ODM.aspx
2.Organização Panamericana de Saúde [site de internet]. Organización Mundial de la Salud. Situación de salud en las Américas: indicadores básicos 2012. [cited 2015 Oct 20] Available from: http://www.paho.org/uru/index.php?option=com_content&view=article&id=756:situacion-salud-americas-indicadores-basicos&Itemid=260
3.Serruya SJ. A morte materna no Brasil: razão e sensibilidade. Rev Bras Ginecol Obstet [Scielo-Scientific Electronic Library Online] 2012 [cited 2015 Nov 15]. 34: 5315. Available from: http://www.scielo.br/prc
4.Organização Mundial de Saúde [site da internet]. The Millennium Development Goals Report 2008. [citado em 15 nov 2013] Available from: http://www.un.org/millenniumgoals
5.Secretaria do Estado de Saúde de Mato Grosso [internet]. [cited 2014 Apr 12] Available from: http://www.saude.mt.gov.br/aplicativo/indicadores
6.Viana RC, Novaes MRCG, Calderon IMP. Mortalidade materna - uma abordagem atualizada. Com Ciências Saúde. 2011; 22 Sup 1:S141-52.
7.Morse ML, Fonseca SC, Barbosa MD, Calil MB Eyer FPC Mortalidade materna no Brasil: o que mostra a produção científica nos últimos 30 anos? Cad. Saúde Pública [Scielo-Scientific Electronic Library Online] 2011 [cited 2015 Nov 15]. 27: 623-38. Available from: http://www.scielo.br/prc
8.Organização Mundial de Saúde [site da internet]. World Health Organization 2010. Trends in maternal mortality: 1990–2008. [cited 2015 Apr 12] Available from: https://www.unfpa.org/sites/default/files/pub-pdf/trends_matmortality90-08.pdf
9.Laurenti R, Jorge MH, Gotlieb SL. A mortalidade materna nas capitais brasileiras: algumas características e estimativa de um fator de ajuste. Rev Bras Epidemiol [Scielo-Scientific Electronic Library Online] 2004 [cited 2015 Nov 15]. 7:449-60. Available from: http://www.scielo.br/prc
10.Progianti JM, Hauck FT. A implantação do modelo humanizado de assistência ao parto na cidade de Juiz de Fora. Rev. enferm. UERJ. 2013; 21:324-9.
11.Teixeira NZF, Pereira WR, Barbosa DA, Vianna LAC. Mortalidade materna e sua interface com a raça em Mato Grosso. Rev. Bras. Saude Mater. Infant. [Scielo-Scientific Electronic Library Online] 2012 [cited 2014 Apr 12]. 2:27-35. Available from: http://www.scielo.br/prc
12.Langaro F, Santos AH. Adesão ao Tratamento em Gestação de Alto Risco. Psicol cienc prof [Scielo-Scientific Electronic Library [Online] 2014 [cited 2015 Nov 15].34: 625-42. Available from: http://www.scielo.br/prc
13.Ministério da Saúde(Br). Secretaria de Atenção à Saúde. Atenção ao pré-natal de baixo risco. Brasília: Ministério da Saúde, 2012.
14.Barbosa TLA, Gomes LMX, Dias OV. O pré-natal realizado pelo enfermeiro: a satisfação das gestantes. Cogitare enferm. [online] 2011 [cited 2015 Nov 15]. 16: 29-35 Available from: http://ojs.c3sl.ufpr.br/ojs/index.php/cogitare/article/view/21108/13934
15.Gaíva, MAM, Fujimori E, Sato, APS. Mortalidade neonatal: análise das causas evitáveis. Rev. enferm. UERJ. 2015; 23:247-53.
16.Khan N , Pradhan MR. Identifying Factors Associated with Maternal Deaths in Jharkhand, India: A Verbal Autopsy Study. J Health Popul Nutr [online]. 2013 [cited 2015 Nov 15]. 31:262-71.