(*) M=Mean; (**)SD=standard deviation; (***)SEM=standard error of the mean; (****)CV=coefficient of variation.
ORIGINAL RESEARCH
Stigma among nursing students before and after contact with people with mental disorders
Isabel Maria de Assunção GilI; José Carlos Pereira dos SantosII; Luís Manuel de Jesus LoureiroIII
I
Master in Cultural Psychiatry. Nursing PhD Student at Portuguese Catholic
University. Associate Professor at Nursing School of Coimbra, Portugal.
Email: igil@esenfc.pt
II
PhD in Mental Health. Coordinator Professor at Nursing School of Coimbra,
Portugal. Email: jcsantos@esenfc.pt
III
PhD in Mental Health. Associate Professor at Nursing School of Coimbra,
Portugal. Email: luisloureiro@esenfc.pt
DOI: http://dx.doi.org/10.12957/reuerj.2016.12309
ABSTRACT
Objective: to examine nursing students' attitudes and beliefs about mental illness and the mentally ill and the effect of clinical training on these beliefs and attitudes by comparing stigma before and after clinical teaching. Method: this is a pre-experimental study and the sample comprised 89 students on an undergraduate Nursing course, in Portugal, in 2010. Data were collected using a Mental Illness Beliefs Inventory and the translated and adapted Portuguese version of the Opinions about Mental Illness Scale. Results: the results related to beliefs and attitudes before and after clinical training reveal a statistically significant effect on the belief in incurability and the attitude towards social restriction. Conclusion: the clinical training contributes to a more positive outlook in nursing students' beliefs and attitudes.
Keywords: Beliefs; attitude; students, nursing; mental disorders.
INTRODUCTION
Stigmatization, discrimination and non-respect for the human rights and the dignity of mentally ill people are still a reality challenging core European values1. Within this perspective, it is indisputable that mental disorders have been subjected to political and social rules, traditions, economic interests, and history2. Each historical period accentuates the complexity of attitudes and perceptions that coexist and give meaning to the phenomenon of madness and mental disorders.
Acknowledging that training ensures a better use of knowledge and a more reasoned intervention, nurses are now aware that mental health is developed and promoted in the day-to-day life of individuals within a given culture, technique and civilization, and that an investment should be made in education, culture and family in favor of the mental health of the populations3.
Building an identity, which is perceived as an eminently relational process, involves understanding the macrosociological structural phenomena that affect the students' attitudes and behaviors4. The way beliefs and attitudes, namely stigmatizing attitudes and discriminatory behaviors, are influenced by the contact with people with mental disorders has not been a major area of research in Portugal. Therefore, we decided to conduct a pre-experimental study with the following research questions:
- What are the beliefs about mental disorders and mentally ill patients of 3rd-year Nursing students before and after completing the Clinical Teaching in Mental Health and Psychiatric Nursing?
- What are the attitudes toward mental disorders and mentally ill patients of 3rd-year Nursing students before and after completing the Clinical Teaching in Mental Health and Psychiatric Nursing?
The purpose of this study was to analyze the beliefs and attitudes of Nursing students and the impact (through in vivo contact) of the Clinical Teaching in Mental Health and Psychiatric Nursing on those beliefs and attitudes.
LITERATURE REVIEW
Since childhood, individuals develop beliefs about themselves, the others and the world, i.e. absolute truths that guide them in their everyday lives.
These beliefs will shape attitudes, which, in turn, will operate as mediators between how we act and how we think5.
Research data suggest that attitudes result from learning and are largely influenced by individual experiences and the social context in which they occur6. Therefore, attitudes have a strong cultural influence insofar as we tend to adopt the attitudes that prevail within the culture where we grow up, particularly within the family structure.
The possibility of predicting behaviors in certain situations is one of the reasons for exploring attitudes7.
When addressing the issue of the beliefs and attitudes toward people with mental disorders, we should take into account how the prevailing view on this subject was built. The stigmatized view of the mentally ill patient - the mad person - has prevailed over time and, consequently, these individuals have remained socially excluded.
Within the new paradigm, the concept of madness evolved to the concept of mental disorder and the asylums gave place to the hospitals. This change of terminology reflects a clear change in how mental disorders and care practices are now perceived8.
Although the International Classification of Diseases (ICD-10) adopts the term mental disorders9, the terms mental illness and mentally ill patients continue to be commonly used in the academic and clinical settings, being the terminology used in the instruments applied in this study.
People with mental disorders anticipate rejection and discrimination, experiencing a form of self-stigma. In this regard, researchers distinguish between public stigma (how the general public reacts to a group based on stigmatized views about that group) and self-stigma (the process of transformation through which the person gradually loses his/her identity and stops performing his/her family, professional and social roles, adopting an attitude of self-devaluation)10-12.
Stigma is composed of three interrelated problems: the problem of knowledge: ignorance (literacy); the problem of attitudes: prejudice; and the problem of behavior: discrimination13.
The strategies for reducing the impact of public stigma and self-stigma have been grouped by relevance10. Therefore, the key strategies capable of changing stereotypes and prejudice, while promoting the adoption of health beliefs aimed at improving health care adherence, have been addressed and grouped into three processes of change: protest/complaint, education/awareness, and contact14.
Protest/complaint strategies emerge against the injustice of specific stigmas, leading to a moral appeal to change the way the public views people with mental disorders. Evidence suggests that these approaches can be successful if applied through television and cinema, namely if they reveal the successful therapies allowing millions of people with mental disorders to resume their normal lives.
Adult education strategies have also improved the attitudes toward people with mental disorders13 by contributing to promote mental health literacy and increase reflection on and change of attitudes. They are also essential to deconstruct negative beliefs and promote the development of skills for the identification and awareness of risk factors for certain mental disorders15.
Studies have shown a strong correlation between feelings of fear and the level of social distancing of the public toward mental disorders due to the scarcity of contacts16. As such, the efforts to familiarize the public with people who are more familiar with mental disorders should be intensified. This idea is corroborated by studies demonstrating an inverse relationship between the contact with mental disorders and stigma 16-18.
It should also be noted that some studies confirm a strong reduction of prejudice and promotion of positive attitudes toward people with mental disorders when the contact involved mainly face-to-face (in vivo) interaction in professional or institutional settings16,19,20.
Mental health services are currently being restructured21 with guidelines that are driven by a type of care based on prevention and reintegration aimed at eradicating stigma and increasing awareness on mental health issues through laws on the protection of people's rights. In light of these changes, we should also analyze the issues related to the qualifications and training of the health care professionals22 who play a key role in the implementation of paradigmatic, structural, operational and doctrinal changes23. Within this scope, Nursing has sought to offer a more humanized care grounded in the principles of the psychiatric reform, which requires nurses to rethink their competences and their practices, reassess their attitudes, and provide care focused on the person, who has the right to be assisted without being excluded24.
Nursing training is characterized by the alternation between periods of in-class training, with theoretical/theoretical-practical classes and laboratory practice, and periods of practical clinical teaching in several health care institutions. These are key moments for the development of professional skills, consolidation of knowledge, and reflection on the practices25.
METHODOLOGY
Given the lack of empirical research studies with Nursing students in Portugal, we conducted a pre-experimental study comparing the stigma among students before and after the Clinical Teaching in Mental Health and Psychiatric Nursing.
The sample was selected in 2010 from the population of 3rd-year students of the Undergraduate Nursing Degree attending a Nursing School in the Center region of Mainland Portugal. These students had already attended the course of Mental Health and Psychiatric Nursing, which includes 54 hours of theoretical classes, 18 hours of theoretical-practical classes, and 9 hours of laboratory practice.
A total of 140 questionnaires were distributed to all students on the first day of their Clinical Teaching in Mental Health and Psychiatric Nursing. After the Clinical Teaching, the 140 questionnaires were distributed again, of which 89 were validated. This second moment had a rate of refusal to participate of 36.44%.
The Clinical Teaching in Mental Health and Psychiatric Nursing, which is carried out in short- and long-term psychiatric inpatient units, lasts 5 weeks, and has a workload of 35 hours/week, in a total of 175 contact hours.
Data were collected through a questionnaire consisting of a sociodemographic characterization, the Opinions about Mental Illness (OMI) scale26, which was translated and validated for the Portuguese population27,28, and theInventário de Crenças acerca das Doenças Mentais (ICDM) 28.
The OMI scale is composed of five factors corresponding to five attitudes: Authoritarianism (view that considers mentally ill people as belonging to an inferior class and requiring coercive handling); Benevolence (a moralist, paternalistic and protective view of mentally ill people that is based on a humanist and religious-moral perspective rather than on a scientific and professional ideology) ; Mental hygiene ideology (a positive view of mental disorders which demonstrates confidence in the interventions of mental health professionals); Social restrictiveness (a view in which mentally ill people are seen as a threat to society and whose freedom must be restricted); and Interpersonal etiology (a view that considers mental health as arising from individual life choices). The scale is rated from 1 (strongly disagree) to 6 (strongly agree)27,28.
The ICDM is a 6-point Likert-type scale composed of 45 items divided into six beliefs: Incurability (belief in mental disorders as being chronic and incurable); Recognition of the disease (belief in a non-stigmatizing view of mental disorders associated with the acceptance of the disease); Dangerousness (belief in mentally ill people as dangerous individuals, given the unpredictability of their behavior, tending to criminality); Disease as a cause of stigma and discrimination (personal belief of disease-related stigma and prejudice in the social contexts surrounding people with mental disorders); Personal responsibility (belief in the individual as responsible for his/her health/illness); Disease as a medical condition (belief in mental disorders as clinical conditions which should be pharmacologically treated). The answers range from 1 (strongly disagree) to 6 (strongly agree)28.
In relation to the ethical procedures, this study was approved by the Ethics Committee of the Faculty of Medicine of the University of Coimbra and by the President of the School where the study was conducted.
The statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 17 for Windows, and the G*Power software for calculating the effect size and the power of tests.
With regard to the statistics, the absolute and percentage frequencies, as well as the summary statistics were calculated. To assess the impact of the Clinical Training on the beliefs and attitudes, we compared the means before and after the Clinical Training using the paired Student's t-test. We also calculated the post-hoc power of the tests and the measure of effect size.
To calculate the effect size, we used Cohen's d, which corresponds to the standardized mean difference, with the Student's t-test, and transformed it into r2 (coefficient of determination), which represents the percentage of explained variance. A post-hoc power analysis was conducted, considering an alpha of .05 for n=89. We used the values proposed by Cohen29 for interpreting the effect size.
RESULTS AND DISCUSSION
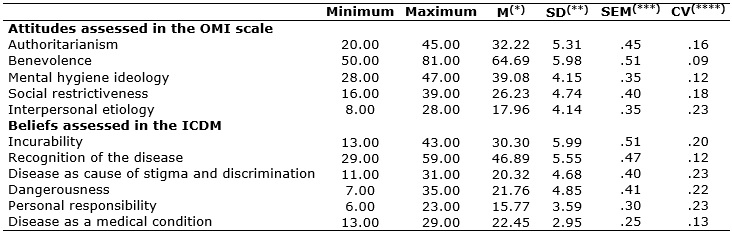
With regard to the results, Table 1 shows the summary statistics for each belief and attitude.
TABLE 1:
Summary statistics for the dimensions of the OMI scale and the ICDM (n=89)
- attitudes and beliefs of Nursing students toward mental disorders and
people with mental disorders, Coimbra, Portugal, 2010.
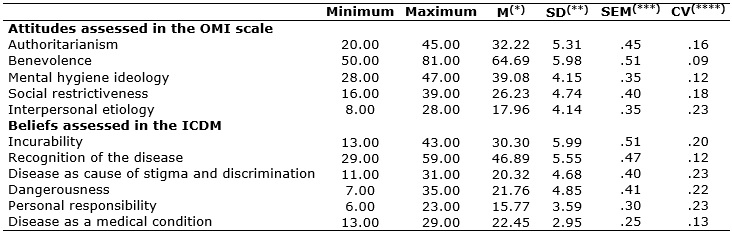
(*)
M=Mean; (**)SD=standard deviation; (***)SEM=standard
error of the mean; (****)CV=coefficient of variation.
From the analysis of the weighted averages, we concluded that the beliefs with higher scores (>4.00 points) toward concordance are theRecognition of the disease and Disease as a medical condition, pointing to homogeneous responses. Conversely, the scores in the remaining beliefs generally point to discordance, being more marked in Disease as cause of stigma and discrimination. This shows that, in this specific belief, Nursing students do not believe that mental disorders are, by themselves, a cause of social stigma and discrimination.
These results show that Nursing students have a non-stigmatizing view of mental disorders, associated with the acceptance of the disease and the belief in treatment and rehabilitation when patients are diagnosed in a timely manner. However, we should note that the results obtained in our study can somehow be explained by the fact that students had already acquired theoretical knowledge about this issue during the course of Mental Health and Psychiatry, and that such knowledge may have contributed to a less stigmatizing view. Despite this, the stereotypes of dangerousness, incurability and personal responsibility are still intensified. These findings are in line with some studies that also point to the persistence of myths characterized by beliefs in the dangerousness and incurability of people with mental disorders28,30.
With regard to the attitudes about mental disorders and people with mental disorders, we applied the same procedures to the OMI dimensions. Thus, as in the ICDM, the low standard error of the mean in all dimensions shows that the mean is a good estimator. On the one hand, the high values (>.15) of the coefficients of variation indicate that the scale, has discriminating ability, and, on the other hand, suggest a more homogeneous position in the answers related to the Benevolence and Mental hygiene ideology dimensions.
As regards the mean score of attitudes, we observed that the Benevolence dimension obtained a higher mean score, immediately followed by the Mental hygiene ideology and the Authoritarianism dimensions. The Interpersonal etiology dimension had the lowest mean score.
These results, which suggest high levels of tolerance and social sensitivity toward these problems, may be related to previously acquired knowledge since studies indicate that a better knowledge on mental disorders makes people less prone to stigma and discrimination16,18,31,32.
According to Table 2 on the analysis of the results of the Student's t-test for paired samples, we observed that, despite the very low power of tests, all belief-related dimensions are statistically significant, with the exception of the Incurability and Personal responsibility dimensions.
TABLE
2 -
Results of the Student's t-test for paired samples (t -
calculated t; P - level of significance; d -
measure of effect size; OP - Observed Power). Dependent variables:
beliefs and attitudes toward people with mental disorders (n=89), Coimbra,
Portugal, 2010.
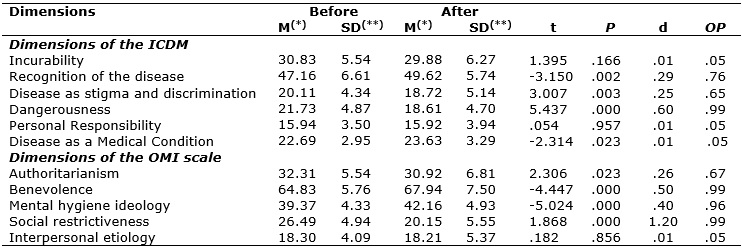
(*) M= Mean; (**) SD= Standard deviation
We found an increase in the mean scores for the beliefs related toRecognition of the disease and Disease as a medical condition, and a decrease in the mean scores for the beliefs related toDisease as cause of stigma and discrimination and Dangerousness.
With regard to the results obtained from the effect size measures and the power of tests, we should note that, when the mean differences are statistically significant, the d-values are small, with the exception of the belief in Dangerousness, which points to a medium effect size.
Therefore, based on the analysis of the impact of the Clinical Teaching on the beliefs about people with mental disorders, we found a decrease in negative beliefs. These results are in line with other studies which reported that the discriminatory beliefs of students are positively influenced by education16,32. We concluded that the beliefs related to the unpredictability and dangerousness of the mentally ill person proved to be weaker, thus, less stigmatizing. The model proposed by some authors also indicates that contact significantly decreased the belief in the dangerousness of people with mental disorders16. Here, it is important to stress that educational strategies have more positive effects when associated with the direct contact with people with mental disorders14. In this case, contact is particularly important for the person to acknowledge the mentally ill patient as a real person33,34, contributing to the reduction of stigmatizing beliefs. Furthermore, the combination of contact and education has proven to be the most effective strategy, particularly in the long-term31.
With regard to the impact of Clinical Teaching on the students' attitudes, with the exception of the attitude related to Interpersonal etiology, all the mean differences were statistically significant before and after the Clinical Teaching, decreasing in the Authoritarianism andSocial restrictiveness dimensions, and increasing in the Benevolence and Mental hygiene ideology dimensions.
The analysis of the effect size values revealed small effect sizes in the attitudes related to Authoritarianism (d=.26) and Mental hygiene ideology (d=.40) and medium effect sizes in the attitude of Benevolence (d=.50). The highest effect size was observed in the attitude related to Social restrictiveness (d=1.20), which showed a large effect size, with Clinical Teaching having a substantial impact.
Similarly to what we found regarding the beliefs, we also found that Clinical Teaching reduced the students' negative attitudes of Authoritarianism and Social restrictiveness and increased the positive attitudes of Benevolence and Mental hygiene ideology. These results confirm that the Clinical Teaching contributes to a more positive view, which is corroborated by other studies confirming that the direct interaction with people with mental disorders has a positive significant impact on the attitudes of Nursing students toward these patients35,36 and, more specifically, that the Clinical Teaching in Mental Health and Psychiatric Nursing contributes to a positive change in the students' perceptions of people with mental disorders34,37. Therefore, the clinical practice in hospital settings is a fundamental pillar in the students' training process38. Similarly, the results of a study carried out in Brazil also revealed that the Nursing education led to a change of attitudes among students, namely by reducing negative attitudes39.
CONCLUSIONS
Based on the objectives set out for this study, we will summarize the most relevant conclusions:
· The beliefs and attitudes showing a greater acceptance and tolerance point to an increasing recognition and awareness of the nature of mental disorders as medical conditions, although we should not overlook the myths on the incurability, dangerousness and unpredictability of people with mental disorders;
· Although the Clinical Teaching promotes a change in the beliefs and attitudes of Nursing students, the fact that it has a moderate effect indicates the need to prioritize contents that increase mental health literacy in the curricula;
· The change of attitudes and beliefs is more evident in the need to socially reintegrate the patients, as shown by the decrease in the attitude of Social restrictiveness. This is a positive effect of the Clinical Teaching, indicating that the contact and experience with Psychiatric Nursing practice increases the awareness of the need to ensure the protection of patients' rights and freedoms.
Since this study was conducted in a single Portuguese Nursing School, the sample is not representative of the Portuguese population. As such, the results, and subsequent conclusions, should be carefully interpreted.
Although we sought to include in the sample all 3rd-year students of the Undergraduate Degree, the rate of refusal to participate was high, which constituted a limitation of this study.
REFERENCES
1.Comissão das Comunidades Europeias. Livro Verde melhorar a saúde mental da população rumo a uma estratégia de saúde mental para a União Europeia. Bruxelas; 2005.
2.Foucault M. História da loucura na Idade Clássica. 8ª ed. São Paulo: Editora Perspectiva; 2007.
3. Milheiro J. Loucos são os outros. Porto: Laboratórios Bial; 1999.
4.Serra MN. Aprender a ser enfermeiro: Construção identitária profissional por estudantes de Enfermagem. Lisboa: editora Lusociência; 2013.
5. Lima M. Atitudes. Psicologia Social. 2ª ed. Lisboa: Fundação Calouste Gulbenkian; 1997.
6.Cardoso A. A receptividade à mudança e à inovação pedagógica: o professor e o contexto escolar. Edições ASA: Perspectivas actuais/educação; 2003.
7.Oliveira ERFLD. Atitudes dos alunos brancos em relação a alunos negros. Tese publicada. Porto: Universidade Aberta; 2007.
8.Moreira P, Melo A, Lima A, Pires C, Crusellas L. Saúde mental. Do tratamento à prevenção. Porto: Porto Editora; 2005.
9.Organização Mundial de Saúde. CID-10: Classificação Internacional de Doenças; 2010; [cited 2014 Jan 10]; Available from: http://www.who.int/classifications/icd/icdonlineversions/en
10.Watson, AC, Corrigan PW. Challenging public stigma: a targeted approach. On the stigma of mental illness: practical strategies for research and social change. Washington: American Psychological Association. 2005:281-95.
11.Brohan E, Gauci D, Sartorius N, Thornicroft G. Self-stigma, empowerment and perceived discrimination among people with bipolar or depression in 13 European countries: The GAMIEN-Europe study. Journal of Affective Disorders. 2011; 129(1):56-63.
12.Yanos PT, Roe D, Markus K, Lysaker P.H. Pathways between internalized stigma and outcomes related to recovery in schizophrenia spectrum disorders. Psychiatric Services. 2008; 59(12): 1437-442.
13.Thornicroft G, Brohan E, Kassam A, Lewis-Holmer E. Reducing stigma and discrimination: candidate interventions. International Journal of Mental Health Systems. 2008; 2 (39):1-7.
14.Corrigan PW, Penn, DL. Lessons from social psychology on discrediting psychiatric stigma. American Psychologist. 1999; 54 (9):756-76.
15.Oliveira S, Carolino L, Paiva A. Programa Saúde Mental Sem Estigma: Efeitos de Estratégias Diretas e Indiretas nas Atitudes Estigmatizantes. Revista Portuguesa de Enfermagem de Saúde Mental.2012; (8): 30-37.
16.Corrigan PW, River LP, Lundin RK, Penn DL, Uphoff-Wasowski K, Campion J, et al. Three strategies for changing attributions about severe mental illness. Schizophrenia Bulletin. 2001; 27(2):187-95.
17.Penn DL, Combs DR, Ritchie M, Francis J, Cassisi J, Morris S, Towsend M. Emotion recognition in schizophrenia: further investigation of generalized versus specific deficit models. Journal of Abnormal Psychology. 2000;109 (3):512-16.
18.Romem P, Anson, O, Kanat-Maymon Y, Moisa R. Reshaping students' attitudes toward individuals with mental illness through a clinical nursing clerkship. The Journal of Nursing Education. 2008; 47(9): 396-402.
19.Read J, Harre N. The role of biological and genetic causal beliefs in the stigmatisation of "mental patients", Journal of Mental Health. 2001;10(2):223-35.
20.Pinfold V, Toulmin H, Thornicroft, G, Huxley P, Farmer P Graham T. Reducing psychiatric stigma and discrimination. Evaluation of educational interventi ons in UK secondary schools. British Journal of Psychiatry. 2003;182(4):342-46.
21.Direção Geral de Saúde (Pt). Reatualização do Plano Nacional de Saúde Mental. Programa Nacional para a Saúde mental. Portugal, 2012; [cited 2014 June 2]; Available from: http://www.saudemental.pt/wpcontent/uploads/2012/06/Recalendarizac%CC%A7a%CC%83o_PNSM.pdf
22.Silva LH. Educação do campo e pedagogia de alternância. A experiência brasileira. Texto da conferência proferida na Faculdade de Psicologia e de Ciências da Educação da Universidade de Lisboa a 17 de Maio de 2007. Sísifo: Revista de Ciências da Educação; [cited 2008 Sep 20]; 5: 105-12. Available from: http://sisifo.fpce.ul.pt
23. Pessoa JM., Santos RCA, Clementino FS, Oliveira KKD, Miranda FA. A política de saúde mental no contexto do hospital psiquiátrico: Desafios e perspectivas. Esc. Anna Nery [Internet]. 2016 Mar [cited 2016 Mar 15]; 20(1):83-89. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414-81452016000100083&lng=pt .
http://dx.doi.org/10.5935/1414-8145.20160012
24.Terra MG, Ribas DL, Sarturi F, Erdmann AL. Saúde mental: do velho ao novo paradigma – uma reflexão. Revista Esc Anna Nery Enferm. 2006;10(4):711-17.
25.Simões JF, Alarcão I, Costa N. Supervisão em ensino clínico de enfermagem: a perspectiva dos enfermeiros cooperantes. Referência. 2008;6:91-108.
26.Cohen J, Struening EL. Opinions About Mental Illness in the personnel of two large Mental Hospitals. Journal of Abnormal and Social Psychology. 1962;64(5):349-60.
27.Oliveira SA. Loucura no outro: Um contributo para o impacto da loucura no profissional de saúde mental. Tese de Doutoramento publicada da Faculdade de Psicologia e Ciências da Educação da Universidade de Coimbra; 2005.
28.Loureiro LMJ. Representações sociais da loucura: Importância para a promoção da saúde mental. Estudo realizado numa amostra de residentes no concelho de Penacova. Tese de Doutoramento publicada do Instituto Superior de Ciências Biomédicas de Abel Salazar. Porto. Universidade do Porto; 2008.
29.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, New Jersey: Lawrence Erbaum;1988.
30.Goerg D, Zbinden E, Fischer W, Guimon J. Representations of psychiatric treatments. Advances in Relational Mental Health. 2004; [cited 2009 July 10] 3(3); Available from http://www.bibliopsiquis.com/asmr/0303/2.pdf
31.Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16-20.
32.Corrigan PW, O'Shaughnessy JR. Changing mental illness stigma as it exists in the real world. Australian Psychologist. 2007;42(2):90-7.
33.Corrigan PW, Lurie BD, Goldman HH, Slopen N, Medasani K, Phelan S. How adolescents perceive the stigma of mental illness and alcohol abuse. Psychiatric Services. 2005;56 (5):544-50.
34.Markstrom U, Gyllensten AL, Bejerholm U. Attitudes towards mental illness among health care students at Swedish universities – a follow-up study after completed clinical placement. Nurse Education Today. 2009;29(6):660-65.
35.Madianos MG, Priam M, Alevisopoulos G, Koukia E, Rougakou E. Nursing students' attitude change toward mental illness and psychiatric case recognition after a clerkship in psychiatry. Issues in Mental Health Nursing. 2005;26(2):169-83.
36.Emrich K, Thompson TC, Moore G. Positive attitude. An essential element for effective care of people with mental illnesses . Journal of Psychosocial Nursing and Mental Health Services. 2003;41(5):18-25.
37.Francisco I. Estudo da percepção dos alunos de enfermagem face à doença mental. Dissertação de Mestrado não publicada em Reabilitação Psicossocial. Porto. Universidade Católica Portuguesa; 2010.
38. Reza CG, Ferreira MA, Silva RC, Gandarilla JV, Solano GS, Martínez VG. Perfil de los estudiantes mexicanos en las clínicas de enfermería. Esc. Anna Nery [Internet]. 2016 Mar [cited 2016 Mar 15]; 20(1): 11-16. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414-81452016000100011&lng=pt . http://dx.doi.org/10.5935/1414-8145.20160002
39.Pedrão LJ, Avanci RC, Malagueti SE, Aguillera AMS. Atitudes frente à doença mental: estudo comparativo entre ingressantes e formandos em enfermagem. Medicina [Ribeirão Preto Online]. Brasil. 2003 [cited 2010 May 14]. 36(1): 37-44. Available from: http://www.revistas.usp.br/rmrp/article/view/533/533