RESEARCH ARTICLES
Formation and professional insertion of obstetrical nursing residency graduates
Adriana Lenho de Figueiredo PereiraI; Marina Caldas NicácioII
IAssociate Professor, Department of Maternal-Infant Nursing. School of Nursing. Rio de Janeiro State University. Brazil. E-mail: adrianalenho.uerj@gmail.com
IINursing Student. Scientific Initiation Scholarship. School of Nursing. Rio de Janeiro State University. Brazil. E-mail: mari_kaldas@hotmail.com.
ABSTRACT: This quantitative descriptive study aimed to describe the training and vocational placement of graduates from the Obstetrical Nursing Residency Program at Rio de Janeiro State University. Nineteen graduate nurses answered a structured questionnaire. The nurses’ prior expectations were fully met by the course (84.2%), although requiring improvements in theoretical content and direct tutorial supervision. Most of the nurses had two jobs (78.9%) and worked in obstetrics (73.7%), predominantly in normal child birth care (36.8%), antenatal care (26.3%) and obstetric emergencies (26.3%). As regards exercising their profession, 42.2% have considered working independently. However, barriers to the profession persist in the health system, such as there stricted employment market, resistance from physicians, lack of professional status, and poor working conditions.
Keywords: Obstetrical nursing; professional practice; nursing education; internship and residency.
INTRODUCTION
The nursing residency course consists of a lato sensu graduate teaching course in the form of a specialization course, characterized by teaching in service, with a workload of 60 hours per week and a minimum duration of two years, as described in Article 3 of Resolution No. 2/2012, from the Department of Higher Education at the Brazilian Ministry of Education (MEC)1.
This type of nursing training emerged influenced by the history of medical residency in the country. The first nursing training in this modality was in 1961, at the Children's Hospital in Morumbi, São Paulo. From the 1970s, other residency programs for nurses appeared in the states of Pernambuco, Rio de Janeiro, Pará and Paraíba2.
Despite the expansion of this type of training in the country, there was a lack of regulatory legislation for the residency programs as lato sensu graduate courses. This lack has caused most of these programs to be linked to non-educational institutions, substantially weakening their pedagogy and supervision, increasing susceptibility to the labor demands of the institution to which it is linked, and to the interests of the labor market, without considering the needs of the population and the Unified Health System (SUS, acronym in Portuguese)3.
Midwifery in-service training, in the form of a residency, did not meet the requirements of training or the certification required for professional practice, particularly for care during normal childbirth. Therefore, the training of these professionals has traditionally been linked to lato sensu graduate courses from higher education nursing institutions4.
The Nursing School at the State University of Rio de Janeiro (ENF/UERJ, acronyms in Portuguese), has trained nurse midwifes since 1970. Initially, this training was through the Specialization in Midwifery, which was a complementary curriculum segment of the Undergraduate Nursing Course. In the late 1990s, the Specialization Course in Obstetric Nursing was instituted.
Since that time, the Nursing School (ENF/UERJ) has established a partnership with the Rio de Janeiro Municipal Health Department for qualifying statutory nurses to work in prenatal care and normal delivery within the municipal health network.
In this context of stimulating performance within obstetric nursing in public maternity hospitals, the Rio de Janeiro Municipal Health Department instituted the Qualification Program for Perinatal Care in the City of Rio de Janeiro in 2002. This program encouraged low-risk childbirth care for nurse midwives and provided for the creation of ten childbirth centers in each municipal program area. However, an insufficient quantity of expert statutory nurses in obstetrics within the municipal health network presented a professional challenge. Moreover, when these specialized professionals were found in the maternity hospitals, most of them had not worked directly in normal childbirth care5.
This problem also occurred during the deployment process of the first Childbirth Center in Rio de Janeiro in 2003. There were few nurse midwives with five or more years of experience in normal childbirth assistance who had enrolled in the internal selection process to work in this institution whose physical structure was already under construction. This problem and the establishment of the Qualification Program contributed to the decision by the Rio de Janeiro Municipal Health Department to propose another partnership with the Nursing School (ENF/UERJ) to create the Specialization Course in Residency Type Obstetric Nursing, which was initiated in 20045.
The Nursing School (ENF/UERJ) is responsible for coordinating the education and certification of registered nurses in lato sensu graduate courses. The theoretical and practical training takes place over a two-year period, with a workload of 60 hours per week. There is also an allowance for residents, which is funded by the Rio de Janeiro Municipal Health Department. Ten vacancies are offered per year and 45 graduate nurses from five groups have qualified as of March 2012.
The Obstetric Nursing Residency at the State University of Rio de Janeiro (UERJ) has clinical partnerships with five large public maternity wards and one childbirth center. The course aims to enable nurses to give complete and humane midwifery care for women experiencing pregnancy, childbirth and puerperium, with an understanding of the social, cultural, emotional and biological determinants of reproductive health. It will also deepen their knowledge of physiology and potential related problems, as well as develop comprehensive care practices that are sensitive to the woman, her child and her family6.
For their pedagogical development, free from the understanding that pregnancy and childbirth are merely physiological events, care should be de-medicalized, humane and respectful of women's sexual and reproductive rights. The second guiding principle of the training residency is that nursing training is a continuous, lifelong process involving the practice-theory-practice movement, and that health care institutions are privileged learning spaces6.
Considering the interaction between training and practice, this present study was proposed to describe the evaluation of the training and professional placement of the alumni from the Residency Course in Obstetric Nursing at the State University of Rio de Janeiro.
LITERATURE REVIEW
Since 1960, nursing teaching has been increasingly guided by the biomedical model and the healthcare trends that gave rise to complex welfare, medical and hospital care. This new conformation of the Brazilian health system prioritized curative actions rather than preventive ones and made the hospital the primary locus of health care. Therefore, the education of health professionals followed this trend of specialized and curative practices3.
At that time, graduate courses were also created through Law No. 4.024/1961, the Guidelines and Bases Law for National Education. Subsequently, Opinion No. 977/1965, from the Federal Council of Education, distinguished graduate courses for graduate candidates who have obtained their diploma, with an emphasis in research training, as specialization, improvement and outreach courses3.
In nursing education, qualifications were established through Opinion No. 163 of the CFE, in 1972, which classified teaching as either pre-professional or common professional. At the end of the common professional segment, the student could opt for qualification in medical-surgical nursing, obstetric nursing or public health nursing7.
This conformation of teaching followed the technical educational model, which was based on behaviorist theories of learning and was appropriate to the requirements of an industrialized and technological society. This educational model placed the health care system under the aegis of modern rationality and the development of the capitalist system in the country7.
The obstetrics area was also influenced by this context, whose care model has become medicalized, technological, interventional and focused on the medical professional. Despite the availability of qualifying midwifery training since the 1970s and 1980s, there were institutional barriers and a lack of political incentive for nursing work in normal childbirth care, which exacerbated the nursing shortage and contributed to the consolidation of the hegemony of this care model in the country5.
From the 1990s, there were important changes in educational and health policies resulting from the democratization of the Brazilian state. Segments adherent to critical theory in education proposed new curricular guidelines conducive to ideals in health reform and in training with a generalist imprint7.
Decree No. 1.721, of December 15, 1994, was published in this context of change, which led to the redesign of the nursing curriculum and fixed the minimum content and duration of the Undergraduate Nursing Course. Since then, the training of nurse midwives has occurred through graduate lato sensu courses3.
The Brazilian Ministry of Health has been undertaking actions aimed at the humanization of obstetric care and the placement of nurse midwives during normal childbirth care. Between 1999 and 2004, 76 specialization courses in midwifery were funded in the country, and 1,366 nurses were qualified as nurse midwives8.
These funded courses faced weaknesses in practical teaching, which hindered the acquisition of necessary technical abilities for care in normal childbirth. Moreover, the graduates from the courses faced factors restrictive to practice due to the persistence of hegemonic structures in the current obstetric practice model4,8,9.
Subsequent government actions, based on the principles of the SUS (Public Health System), have also started to organize training and professional development in the health sector. Regulations for residency courses have been established, such as Law No. 11.129, of June 30, 2005, which created the Residency in the Professional Area of Health and the National Commission on Multidisciplinary Residency in Health, which are linked to the Brazilian Ministry of Education3.
As a result of these policies, in 2012 the Brazilian Ministry of Health promoted a new incentive for the training of nurse midwives in partnership with the Ministry of Education, by creating the National Residency Program in Obstetric Nursing (PRONAENF, acronym in Portuguese).
The PRONAENF residency courses are linked to educational institutions, ensuring the certification of nurses for specialized professional practice. As this is a service-based teaching modality, health care institutions are the central training sites.
These residency courses in midwifery are seen as a promise of a new educational modality that has the greatest potential to qualify nurses with technical skills for care that are based on the principles of humanization and scientific evidence. Nevertheless, the ambivalences and contradictions of the healthcare system described above persist, such as the low degree of interaction between the different professions and specialties, the fragmentation of clinical practice and the poor working conditions of professionals, especially in nursing. These are the substantial pedagogical challenges facing residency programs.
METHODOLOGY
This descriptive and quantitative research study, whose subjects were the 2004-2011 graduates from the Residency Course in Obstetric Nursing at the Nursing School of the State University of Rio de Janeiro (ENF/UERJ), was approved by the Research Ethics Committee, protocol no. 105A/2010.
Structured questionnaires were applied, consisting of 21 closed questions and one open question. Among the closed questions, four provided the choice of up to three alternatives.
The data collection period was from August 2011 to March 2012. There were difficulties related to outdated telephone and electronic contacts, requiring an active search to locate some former student nurses from the course. There were also delays in the return of the questionnaires and, in some cases, this required multiple workplace meetings with the nurses.
The study variables pertained to the socio-professional profile (age, marital status, monthly income and area of professional performance), evaluation of training (prior expectations and shortcomings during the training course) and professional placement (contributing and restrictive factors of professional practice).
The data for the objective questions were tabulated and subjected to descriptive statistical analysis. In the answers to the open question of the instrument, the thematic grouping technique was employed to analyze the content, with registry units (RU) being quantified. Data analysis was based on distribution and dispersion, which were compared with investigations on the theme.
RESULTS AND DISCUSSION
Thirty-six nurses graduated from the Residency Course in Obstetric Nursing at Nursing School of the State University of Rio de Janeiro (ENF/UERJ) in the 2004-2011 period. Nineteen nurses participated in the survey (100%), which corresponded to the sample studied.
The graduates from the course are predominantly female - 18 (94.7%). Most of them are aged between 25 and 30 years - 15 (78.9%) and 1 (5.3%) is over 40 years of age. Most of the graduates (9,47.3%) are single, eight (42.1%) are married, and one (5.3%) lives in a common law marriage. However, one research participant (5.3%) did not respond on to this question.
Nearly all (18,94.7%) subjects are professionally employed. Of these, only two (10.5%) nurses work autonomously in home childbirth care. The majority (15,78.9%) of the graduates work two jobs and one (5.3%) was unemployed. A previous study of 127 graduates from the Specialization Courses in Obstetric Nursing in the Northeast Region of Brazil also found that most nurse midwives (52%) also worked at least two jobs8.
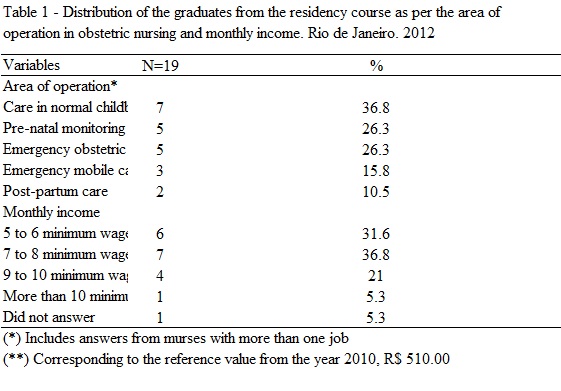
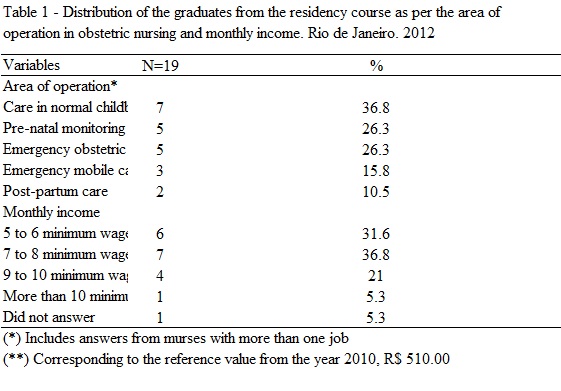
Most of the graduate nurses from the residency course, 14 (73.7%), work in the obstetrics area. This percentage was higher than those found in other surveys of former students from the Specialization Courses in Obstetric Nursing, 37%9 and 52.5%10. These graduate nurses work in normal childbirth care - 7 (36.8%), prenatal - 5 (26.3%), obstetric emergencies - 5 (26.3%), mobile emergency transport - 3 (15.8%) and postpartum care - 2 (10.5%), according to Table 1.
It should be clarified that the emergency obstetric care and mobile emergency transport are components of the Programa Cegonha Carioca Stork Program (a carioca is a person from Rio de Janeiro). The stork refers to both the maternity hospital during the labor process and the obstetric ambulances, which transport the pregnant women enrolled in the program11.
In terms of normal childbirth care, the percentage of former students from the residency course was less than that identified in other investigations, 40.6%8 and 54.5%12. This finding may indicate that there are professional barriers to retention within this nursing specialty. The majority of nursing work is still in large municipal maternity wards. Nurses are still rare or absent in municipal, state, federal or university administration.
After data collection was completed, two municipal hospitals opened in 2012. These institutions, which rely on nurse midwives in normal childbirth care, are administered by social health organizations with publicly controlled labor relationships.
As regards the monthly wage income, seven (36.8%) graduate nurses receive 7-8 minimum wages; six (31.6%) 5-6 minimum wages; four (21%) 9-10 minimum wages and only one (5.3%) had a monthly income greater than ten minimum wages, as described in Table 1.
Demanding activities, requirements and tasks, the low rate of pay and the need for double shifts are factors associated with job stress among nurses. The majority of these professionals are females, who more frequently strive to balance the demands of personal and professional life. Such problems explain the influence of gender as a determinant of professional practice. These issues generate greater vulnerability of these professionals across the current context of casualization of labor and the production process in health care13.
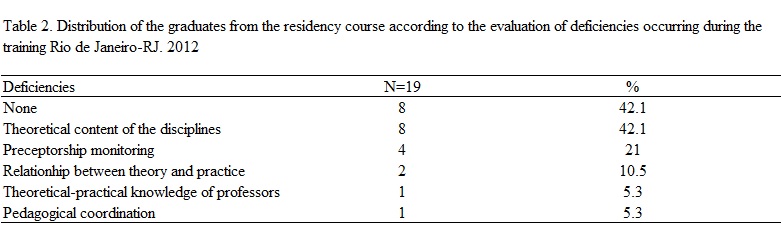
It should be highlighted that 16 (84.2%) nurses reported that the course fully met their expectations and three (15.8%) responded that they were partially met. By way of contrast, eight (42.1%) of the graduates gave the assessment that no deficiencies occurred in their training. The rest found deficiencies in the theoretical component - eight (42.1%), monitoring of the preceptorship - 4 (21%) and the relationship between theory and practice - 2 (10.5%). See Table 2.
Evaluating the training program is not a simple task. Educators have addressed the evaluation methods considering the theories of learning, and the curriculum and its epistemological and philosophical perspectives, which express a particular underlying educational paradigm14.
The positive evaluation expressed by meeting the expectations of the graduates from the residency course did not camouflage the need for improving the theoretical and practical content offered. In contrast, evaluation of training in the residency program had additional complexities, since the process of teaching and learning takes place primarily through the daily care routine at health institutions. Therefore, education and health work are components of this process that need to be considered in the evaluation.
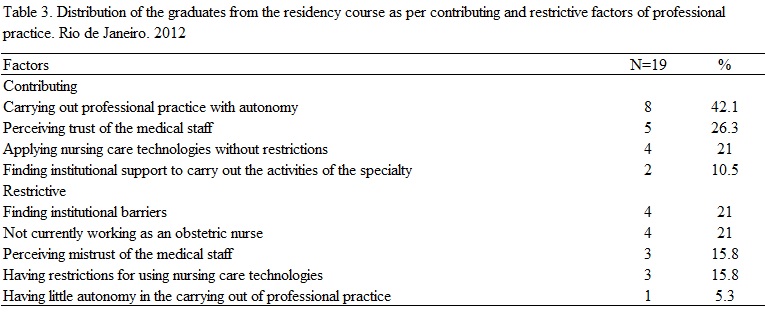
As regards the contributing factors to professional midwifery practice, 8 (42.2%) of the graduates considered entering autonomous practice, 5 (26.3%) perceive that the medical staff has confidence in their practice and 4 (21.0%) apply obstetric nursing care technologies without restrictions.
Despite these findings, the nurses qualified through the course also find restrictions while performing the specialty. It is noteworthy that 4 (21.0%) nurses face institutional barriers to perform their specific functions, 4 (21.0%) do not work as nurse midwives and 3 (15.3%) perceive distrust of the medical staff regarding their professional skills, as can be seen in Table 3.
Analysis of the RU revealed that the major challenges facing the nurse midwives studied were the devaluation of the professional practice of the nurse midwife, poor working conditions, the need for professional recognition, resistance of professional physicians, the need for ongoing qualification and the absence of specific public entrance exams.
Another researcher similarly noted that graduates from the Specialization Courses in Obstetric Nursing considered the following their main professional challenges: the tight labor market, the lack of professional autonomy, medical hegemony and the persistent dominance of the biomedical care model in health services15-17.
Despite this prevalent reality in obstetric care services in the country, the positive professional performance evaluations of the graduates are new data and represent progress of the obstetric nursing profession as a whole in Brazil. This finding requires further investigation through more sensitive methodological designs that can more thoroughly examine the changes in professional practice.
Autonomy, as a value, implies the pursuit of the democratization of relationships, the sharing of knowledge, recognition, respect and appreciation of multiplicity, diversity and uniqueness, greater accountability and citizen participation, redemption of subjectivity and, above all, an ethic of solidarity and responsibility18. This is the great challenge for the ethical-political project contained in the humanization policy of obstetrics, which requires a transformative praxis of interpersonal relationships between subjects and care professionals, as well as between professionals and their peers.
CONCLUSION
The graduates from the Residency Course in Obstetric Nursing at the State University of Rio de Janeiro (UERJ) believed that the training met their expectations. Nevertheless, they pointed out weaknesses in its theoretical content and in the supervision of practical activities during the preceptorship.
Most of the graduates work in the obstetrics area. However, limitations for professional practice still persist, such as institutional barriers, the tight labor market, resistance of medical professionals, little professional recognition and poor working conditions.
The survey also highlighted the need to improve training and teaching strategies to facilitate the construction of socio-political attitudes and skills for the defense of professional practice, with the aim of improved working conditions, since graduates continue to face professional challenges and constraints.
It is worth mentioning that there are limitations in this study related to the research sample size and the methodological design used, which limit the generalization of the findings.
Further investigations are needed to elucidate the issues not resolved by the study and advance the production of data relevant to training nurse midwives, especially in the residency program.
BIBLIOGRAPHY
1. Ministério da Educação (Br). Comissão Nacional de Residência Multiprofissional em Saúde. Resolução nº 2 de 13 de abril de 2012. Dispõe sobre Diretrizes Gerais para os Programas de Residência Multiprofissional e em Profissional de Saúde. Diário Oficial da União 2012 abr; nº 73, Seção 1: 24-5.
2. Justino ET, Przenyczka RA, Kalinke LP, Campos O. História da especialização em enfermagem oncológica - modalidade residência - no hospital Erasto Gaertner. Ciênc Cuid Saúde. 2010; 9(1):167-72
3. Rosa SD, Lopes RE. Residência multiprofissional em saúde e pós-graduação lato sensu no Brasil: Apontamentos históricos. Trab Educ Saúde. 2009-2010; 7(3): 479-98
4. Sacramento MTP, Tyrrell MAR. Vivências das enfermeiras nos cursos de especialização em enfermagem obstétrica. Rev Enferm UERJ. 2006; 14:425-33.
5. Pereira ALF. O processo de implantação da casa de parto no contexto do Sistema Único de Saúde: uma perspectiva do referencial teórico de Gramsci [tese de doutorado]. Rio de Janeiro: Universidade Federal do Rio de Janeiro; 2007.
6. Universidade do Estado do Rio de Janeiro. Faculdade de Enfermagem. Projeto Político-Pedagógico do Curso de Residência em Enfermagem Obstétrica apresentado à Comissão Nacional de Residência Multiprofissional e em Área Profissional do Ministério da Educação. Rio de Janeiro: Departamento de Enfermagem Materno-Infantil; 2012
7. Renovato RD, Bagnato MHS, Missio L, Bassinello GAH. As identidades dos enfermeiros em cenários de mudanças curriculares no ensino da enfermagem. Trab educ saúde. 2009; 7:231-48
8. Costa AANM, Schirmer J. A atuação dos enfermeiros egressos do curso de especialização em obstetrícia no nordeste do Brasil – da proposta à operacionalização. Esc Anna Nery. 2012; 16:332-39
9. Merighi MAB, Yoshizato E. Seguimento das enfermeiras obstétricas egressas dos cursos de habilitação e especialização em enfermagem obstétrica da Escola de Enfermagem, da Universidade de São Paulo. Rev Latino-Am Enferm. 2002;10:493-501
10. Ferreira S L, Rocha MMS, Nunes IM. Atuação de enfermeiras obstetras no sistema único de saúde (SUS-BA): estudo entre as egressas dos Cursos de Especialização em Enfermagem Obstétrica da EEUFBA. Rev Baiana Enferm. 2009; 23(1, 2, 3): 23-32
11. Secretaria Municipal de Saúde e Defesa Civil. Comunicado: Cegonha Carioca expande serviço de ambulância para toda a cidade. Diário Oficial do Município do Rio de Janeiro 2012 nov; n. 166: 124.
12. Barbosa PG, Carvalho GM, Oliveira LR. Enfermagem obstétrica: descobrindo as facilidades e dificuldades do especialista nesta área. O Mundo da Saúde. 2008; 32:458-65
13. Fernandes D. Para uma teoria da avaliação no domínio das aprendizagens.Est Aval Educ. 2008; 19(41): 347-72
14. Baggio MA, Formaggio FM. Trabalho, cotidiano e o profissional de enfermagem: o significado do descuidado de si. Cogitare Enferm. 2008; 13(1):67-74
15. Santos EKA, Monticelli M, Brüggemann OM, Zampieri MFM, Gregório VRP, Oliveira ME. Especialização em Enfermagem Obstétrica da UFSC-1999/2003: perfil e atuação dos egressos. Cienc Cuid Saude. 2008; 7:155-62
16. Vieira BDG, Moura MAV, Alves VH, Rodrigues DP. A prática dos enfermeiros obstetras egressos da especialização da Escola de Enfermagem Anna Nery. Rev enferm UERJ. 2012; 20:579-84
17. Monticelli M, Brüggemann OM, Santos EKA, Oliveira ME, Zampieri MFM, Gregório VRP. Especialização em Enfermagem Obstétrica: percepções de egressas quanto ao exercício profissional e satisfação na especialidade. Texto contexto - enferm. 2008;17:482-91
18. Soares JCRS, Camargo Jr KR. A autonomia do paciente no processo terapêutico como valor para a saúde. Interface - Comunic, Saude, Educ. 2007; 11(21): 65-78.