RESEARCH ARTICLES
Latent tuberculosis infection: adherence to treatment and evolution of cases
Elma Mathias DessuntiI; Denise Andrade Pereira MeierII; Bianca Cuencas DonathIII; Arlete Alves Nunes Fragoso da CostaIV; Maria Helena Dantas de Menezes GuarienteV
IPhD in Public Health, Nursing Student of the State University of Londrina. Londrina, Parana, Brazil. Email: elma@sercomtel.com.br.
IIMaster in Management of Health Services, Nursing Student of the State University of Londrina. Londrina, Parana, Brazil. Email: demeier01@gmail.com.
IIIStudent of the Nursing Course at the State University of Londrina, CNPq. Scholarship holder Londrina, Parana, Brazil. Email: b.donath@gmail.com.
IVNurse Specialist Sanitary Pneumology of the Reference Center for Tuberculosis in Londrina. Londrina, Parana, Brazil. Email: arletefragoso@gmail.com.
VPhD in Nursing, Nursing Student of the State University of Londrina. Londrina, Parana, Brazil. Email: mhguariente@gmail.com.
VIThis Article is part of the Research Project Tuberculin test: review of cases treated at the Reference Center in Londrina over a period of ten years.
ABSTRACT
Treatment of Latent Tuberculosis Infection (LTBI) constitutes an auxiliary resource to active disease control. The aim of this study was to evaluate the cases of LTBI treated at a reference center the city of Londrina-PR. This descriptive study, whose data were collected from 110 notification forms of LTBI cases treated in 2009 and 2010 and supplemented in 2012 by the medical records. Data were tabulated using the Statistical Package for the Social Sciences. An adhesion of 46.4% was detected in patients, dropout rate of 40.9% and two cases developed tuberculosis. Adherence was higher among individuals with 12 or more years of schooling (75.0%). The indication for treatment of LTBI was for contacts of cases (35.4%), conditions that predispose to tuberculosis (23.5%) and immunosuppression by drugs (23.5%). It is concluded the need for improved control of LTBI as a measure for the elimination of tuberculosis.
Keywords: Tuberculosis; prevention & control; latent tuberculosis; chemoprevention.
INTRODUCTION
Treatment of Latent Tuberculosis Infection (LTBI) constitutes a prophylactic measure to prevent the development of TB diseaseIV, especially in household contacts and individuals with a special conditionsuch as, immunosuppression by Human Immunodeficiency Virus (HIV) or through the use of some medications.
Tuberculosis (TB) is a social and public health problem throughout the world, requiring more effective measures for its control. The early diagnosis of the disease is essential action to break the chain of transmission of the bacillus. Considering that the susceptibility to Mycobcterium tuberculosis (Within Mbt) is almost universal, control of contacts is an effective measure to prevent becoming ill and early diagnosis of TB cases active.
The realization of the tuberculin skin test (TST) in the contacts of the index case, as well as individuals who may evolve to immunosuppression, either by some disease or the use of certain drugs, constitutes a valuable resource for diagnosing cases of latent infection with mbt.
The nursing profession has a fundamental role in the control of tuberculosis, through the patient orientation in relation to latent infection and the disease, the forms of transmission of the bacillus, adherence to complete treatment and appropriate and the possible consequences of non-adherence. Effective participation in the management and care actions instituted by the National Tuberculosis Control Programme (NTCP) contributes to improve the quality of health care, as well as global statistics related to the disease.
The realization of the TST at the Reference Center for Tuberculosis and Acquired Immune Deficiency (AIDS) in the city of Londrina syndrome and control of cases requiring treatment, led to the following question: How is adherence and outcome of cases who initiated LTBI treatment at this clinic?
Because of these considerations, this study was proposed with the objective of evaluating the cases of LTBI treated a reference center of the municipality of Londrina-PR.
It is expected that the data obtained may subsidize the actions of nurses and the health care team for the control of tuberculosis.
LITERATURE REVIEW
The LTBI corresponds to the period between the penetration of Mycobcterium tuberculosis (Within Mbt) in the body and the onset of tuberculosis disease evolution, which do not always occur, especially when drug measures are adopted1.
Tuberculosis affects more men than women, especially the economically active groups, it is estimated that two-thirds of cases occur between 15 and 59 years of age2.
The World Health Organization (WHO) has launched several challenges to eliminate TB in the world and the Stop TB strategy is one of them. Its goals are the reduction of prevalence and deaths due to TB and the elimination of the disease as a public health problem by 20152.
The strategy Directly Observed Treatment Strategy (DOTS) - proposed by WHO, from 1993, have not yet reached the global rates of detection (70.0%) and of cure (85% of cases diagnosed), having reached 60% of the cases detected and 84% cure rate2,3.
In Brazil, the cure rates were lower than the target set and dropout rates above 5%, which suggests the need for actions to improve the quality of coverage in DOTS3. The NTPC, launched in 1999, establishes joint actions for the three spheres of government, aiming at the appropriate treatment and other measures for its prevention and control. Among these, there is the detection and treatment of LTBI, especially among household contacts.
The majority of contacts resists the illness after infection, but approximately 10% develop the disease, 5% within two years (primary TB) and 5% after two years by reactivation of latent focus or exogenous reinfection (TB post- primary)4. The risk of developing TB in adults with latent TB and HIV infection rises from 10% to 60 to 80%5, and nursing should be attentive to this group of the population, in an attempt to prevent the progression of the infection to the disease.
The Ministry of Health 3 highlights other conditions that should be considered as a priority in the evaluation process of contacts and treatment of LTBI: children younger than 5 years, people with conditions deemed to be high risk (transplant, use of corticosteroids, kidney failure, among others).
Some factors contribute to increase the susceptibility of infected persons by Within Mbt, as infection by HIV and other forms of immunosuppression, persons with low weight or undernourished, smoking, illegal drug use, debilitating diseases such as chronic renal failure, cancer, silicosis and diabetes5.6.
The treatment of LTBI, when followed correctly, contributes to preventing the outbreak of tuberculosis disease in its various forms. The use of isoniazid reduces in 60 to 90% the risk of illness, being dependent on the duration and adherence to treatment4.
METHODOLOGY
This is a descriptive study, with a quantitative approach, carried out at the Reference Center of Dr Bruno Piancastelli Filho of the City of Londrina-PR. This Center is a reference to the cases of tuberculosis and AIDS and performs the TST of clients referenced in public and private services of the municipality.
The Tuberculosis sector provides medical and nursing care daily, evaluating and treating patients referred by health services in the county and region and characterized as extrapulmonary tuberculosis, reinfection, comorbid conditions, such as AIDS and other special situations. It is noteworthy that the cases of pulmonary tuberculosis are accompanied by basic health units, following the protocols of the Ministry of Health.
The study population was composed by patients notified to the treatment of LTBI and the restricted sample all the cases treated in the years 2009 and 2010, totaling 110 cases.
The data were collected from LTBI Treatment Notification Forms filed in the sector. These forms were implemented by the clinic as of 2009. Some data were supplemented by notes from medical records.
A structured instrument was used containing data such as age, gender, result of the TST reading and chest x-ray, reason for LTBI treatment, medication used and the period of use, side effects, abandonment and evolution of cases.
Data collection occurred from January to March 2012. In July of that same year search was conducted among patients with diagnosis of TB in the Aggravations of Notification (SINAN), to check possible progression to TB disease cases diagnosed with LTBI.
This study was approved by the Ethics and Research Committee of the State University of Londrina, under No. CAAE - 4674.0.000.268 -0.
The data were tabulated by means of the program Statistical Package for the Social Science (SPSS) version 19.0 and the categorical variables are presented in a descriptive manner and through table with simple and relative frequency. For the analysis of continuous variables, descriptive statistics were used with measures of central tendency and dispersion (mean and standard deviation). For comparison of categorical data were used homogeneity tests (Chi-square and Fisher's Exact), considering a significance level of 5%.
RESULTS AND DISCUSSION
The study sample was composed of 110 patients reported with LTBI, being that 57 (51.8%) cases occurred in males. It is noteworthy that TB disease has a higher incidence in men, as well as higher mortality rates and fatality3,7. This allows inferring that the same will happen among individuals with LTBI.
It was observed that 65 (59.0%) subjects were Caucasian, which is predominant in the region where the research was performed and 15 (13.7%) were browns or blacks. In addition, 55 (50.0%) patients had 4 to 11 years of schooling, and 27 (24.5%) less than 3 years or none.
The majority of the cases examined, 89 (80.9%), are from the urban region and 18 (16.4%) of another municipality, which is justified by Londrina to be reference to cases of tuberculosis in the region.
It was identified that some data are not populated in the notification forms, which occurred in 30 (27.3%) cases in relation to race/color and 20 (18.2%) cases in relation to schooling, which can interfere with the definition of the profile of these individuals.
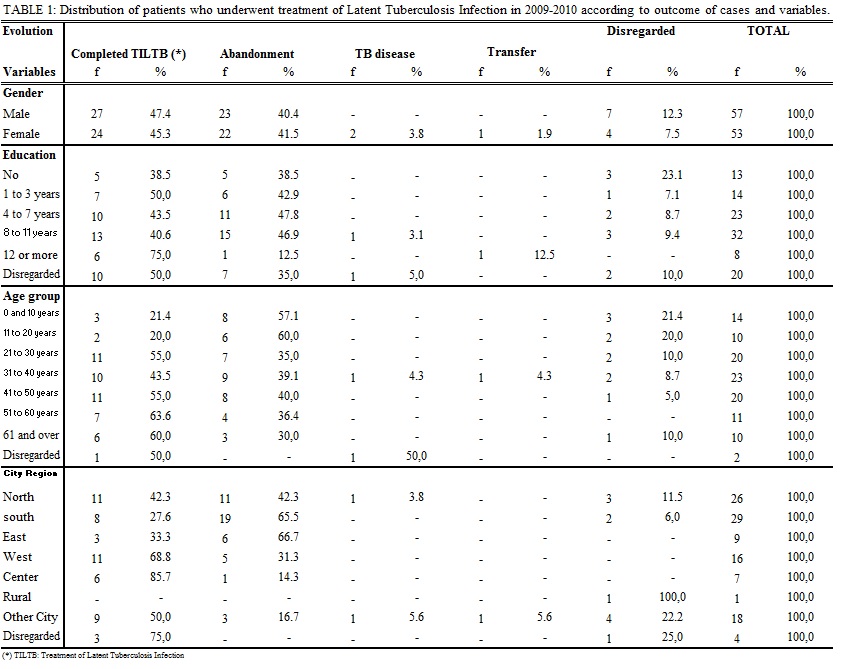
The sociodemographic data, according to the outcome of the cases, are presented in Table 1.
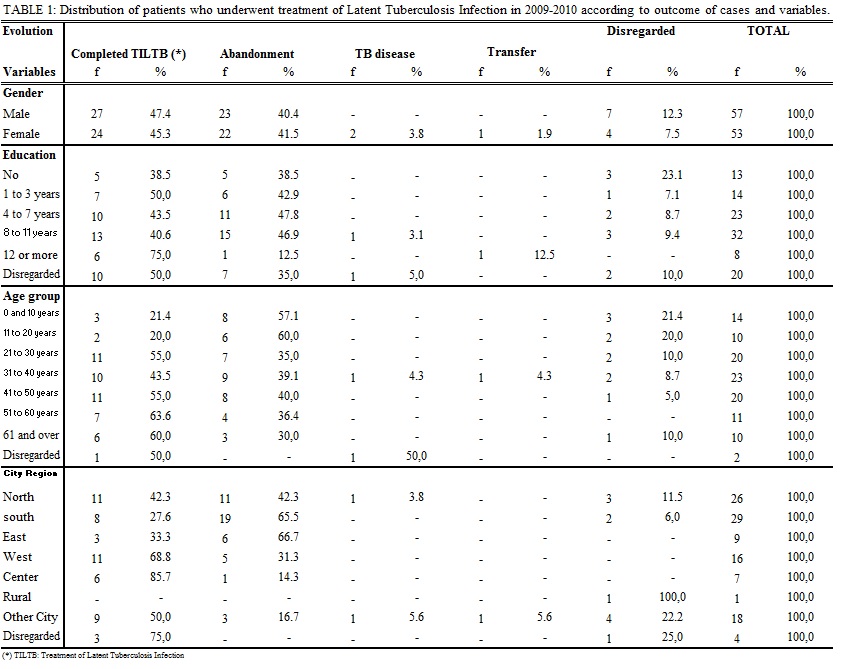
The treatment of the LTBI was complete (6 months) for 27 (47.4%) men and 24 (45.3%) women, as shown in Table 1. However, it was observed that a large number of patients who did not complete the regime, which corresponded to 23 (40.4%) men and 22 (41.5%) women. These individuals are potential cases to develop tuberculosis in the future, especially if they have some condition such as debilitating disease or use of immunosuppressants. It was observed that among women, 2 (3.8%) who did not complete the treatment for LTBI evolved for tuberculosis, both with a form of pulmonary bacillus. A case occurred 18 months after the indication of chemoprophylaxis and another, 12 months after, being that this case presented resistance to isoniazid during the treatment. Analyzing only those cases of termination and abandonment of treatment for LTBI, it showed no association with statistical significance between the genders (p>0.005).
This Study was performed to compare differences between the genders in patients with tuberculosis, a priority city, detected abandonment rate similar between the genders, but well less than that of the present study, i.e., 18.3% in men and 17.1% in women7. These rates may differ between the cases of LTBI and TB, since in the absence of clinical signs and symptoms in first case may encourage non-adherence to treatment and be seen as unnecessary when the individual is not well oriented.
It is noteworthy also that among individuals aged 12 years or more of study, 6 (75.0%) completed the treatment regimen for LTBI, observing similar percentages of completion and abandonment in other levels of education, as exposes Table 1. Regarding the treatment of tuberculosis, the Health Ministry3 percentage points higher healing among individuals with more than eight years of education (77.2%) and highest dropout rate among the illiterate (9.5%). In this study the rate of LTBI treatment noncompliance was 38.5% among the illiterate. However when considering the two extreme ranges of schooling (zero to 3 years and 8 years and more of study) no significant difference (p> 0.005) was observed.
A large percentage of noncompliance of the treatment regimen can demonstrate ignorance about the real need of treatment and the possible consequences such as progression to active tuberculosis and the development of multidrug-resistant bacteria. One of the causes of noncompliance with treatment is the period of 6 months recommended for the use of the drug isoniazid, beyond the side effects resulting from its use. In this study, 19 (17.3%) patients reported one or more adverse effects, not having been possible raise if it was the cause of treatment noncompliance. Noteworthy are the notes contained in the medical records, the digestive effects (13), the joints (4), neurological (3), fatigue (3), and others. No cases of hepatotoxicity were identified.
A systematic review to evaluate treatment regimens of LTBI showed that isoniazid remains effective in preventing TB, both for a period of 6 months as 12 months, recommending the latter regimen for very high-risk groups8.
A multicenter clinical trial was performed to compare the self-administered treatment with isoniazid, for 9 months with supervised treatment with a combination of rifapentine, and isoniazid once a week for three months. The study showed that the two types of regimens are effective to prevent active disease, however, the rate of compliance was lower in the group that used only isoniazid (69%) than in the group with a combination of two drugs (82%), concluding that a shorter treatment time and fewer tablets increases the rate of LTBI treatment adherence (p <0.001)9.
In Brazil, the Ministry of Health 4 ponders that the number of doses taken is more important than the daily use of isoniazid, recommending that the minimum number of 180 doses over a period of 6 to 9 months.
In this study, the average age of patients with LTBI was 34.8 years (SD= 18.1), with a minimum age of 1 year and a maximum of 79 years. There was a significant dropout rate among children 0-10 years (57.1%) and 11-20 years (60.0%), more patients who completed treatment were in the age group of 51 years or more as shown in Table 1. Noncompliant cases in younger age groups associated the ability of the MBT to remain in a latent form, contribute to the onset of active tuberculosis in adults and elderly individuals, especially if they are suffering from other diseases such as AIDS, diabetes, immunosuppression, among others.
The recommendation is that the treatment of the LTBI is instituted for the minors of 5-years of age, adolescents and young adults who present TST positive8.10.
Among the regions of the municipality in which there is a higher rate of abandonment, asserting that the eastern region (66.7%), south (65.5%) and north (42.3%), according to Table 1. The patients of the center region were those who most joined the full treatment (85.7%), followed by the western region (68.8%). These data point to the need to improve the control of cases of LTBI, especially in regions that are concentrated neighborhoods with more vulnerable populations.
For the prevention of noncompliance with treatment for active TB, the NPTC recommends actions for community participation and intrasectoral links with poor or extremely poor population 11, a strategy is that it could be applied to cases of LTBI.
The distribution of patients underwent to TST, according to the indication of LTBI treatment, is analyzed below.
It was noted that 49 (35.7%) patients with LTBI, were requested contact with people with TB in their homes, both adults as well as minors under 10 years of age. The Centers for Disease Control and Prevention considers that the investigation of contacts must be one of the priority activities for the control of TB, action that has helped to reduce the incidence of the disease in approximately 44%, between the years 1993 and 2004 in the United States10. It is assumed that the primary healthcare units should provide a better access to individuals who require treatment of LTBI, a time that is the main port of entry for the treatment of TB, according to the study carried out in a capital of the northeast Brazil12.
Among the 32 cases of diseases that predispose to TB, 24 (75.0%) were associated with HIV infection and 7 (21.9%) to diabetes.
In HIV-infected patients and with tuberculin test ≥ 5mm, the treatment with isoniazid has been effective in preventing TB. However, it is observed that the exam has not been routinely indicated for these individuals, as was demonstrated in a study conducted with 669 patients with HIV/AIDS, in which only 23.4% of them received a referral for the exam13.
The non-use of isoniazid is associated with the risk of seven to 80 times higher to develop TB, being well tolerated in patients with HIV and is not associated with a significant increase of hepatic adverse effects 14. There is controversy in relation to the period of use of this drug, with recommendation of 6, 9 and up to 12 months3.
It has been observed low protection of isoniazid in HIV positive individuals anergics (negatives to TT), possibly due to the difficulty in drug absorption and advanced immunosuppression 8. This reinforces the importance of early diagnosis of HIV infection, considering that the cellular response is more effective to TST, directing for the treatment of LTBI when positive, provided that it ruled out the possibility of active TB.
Another recommendation for the treatment of LTBI is Diabetes Mellitus, as well as lymphomas and severe kidney disease that cause some degree of immunosuppression or require the use of corticosteroids as part of their treatment, favoring the development of TB by reactivation of the infection8.
The use of drugs such as TNF-α blockers for the treatment of rheumatoid arthritis and other inflammatory diseases has contributed to the development of pulmonary and extrapulmonary tuberculosis, recommending prophylactic use of isoniazid for individual TST reactors. In this study, 32 cases were referred for treatment of LTBI due to immunosuppression by drugs, 19 (59.4%) by the use of TNF-α and 14 (43.8%) by use of corticosteroids. The prospective study has detected a dropout rate of 2.2% and the authors point out that the good adherence occurred due to some factors, such as the awareness of patients about the importance of prevention of tuberculosis in the course of treatment with immune-biological drugs. They also highlighted that the use of isoniazid reduces the risk of TB, but does not eliminate, one should maintain surveillance during treatment with TNF-α immunobiological inhibitors.
Limiting the use of TST has been identified in individuals with rheumatoid arthritis, candidates for the use of TNF-α, due to abnormal cellular immune function observed in these patients, resulting in a false-negative response16. On the other hand, the use of these drugs seem to favor the disruption of granuloma limiting the spread of Mbt during latent infection, which contributes to the development of active TB17. Thus, it is recommended that all patients with rheumatoid arthritis are submitted to TST, the chest x-ray, as well as a careful investigation of the history of exposure to the microorganism16,17. These patients should be monitored during the entire treatment and guided on the appearance of signs and symptoms of tuberculosis, especially when there are no formal indication for treatment prior to LTBI.
In Brazil, the use of corticosteroids (>15mg of prednisone or equivalent, for a period of more than 1 month) for patients whose TST is ≥5mm, there is no indication of LTBI treatment1,3.
The low specificity of the TST due to cross-reaction with the BCG vaccine and with other mycobacteria has led to the search for other substances for the diagnosis of LTBI, such as the T-Spot.TB test. In patients with psoriasis treated with immunobiological drugs, no indication of LTBI research, due to the risk of developing serious forms of TB. The low specificity of TST, associated with dubious results presented by patients with psoriasis, it would indicate the achievement of other alternative tests for the detection of LTBI. These patients may have both false negative and false positive TST, recommending the completion of the T-Spot.TB test, whose sensitivity reaches 96%, significantly higher than the TST (69%) (69%) 18. However, this test is not yet available for use in Brazilian health services, maintaining the indication of TSTwith a recommendation of strict monitoring of negative cases prompting especially for the clinical manifestations of TB.
The TST conversion was indication for treatment of LTBI, 11 (8.0%) contacts with TB patients. The recent tuberculin conversion (last 12 months) with an increase of at least 10 mm in response to the second TST, is indicated for the treatment of LTBI, especially in contacts bacillary cases and in workers exposed to Mbt3,8.
Although it has not been the history of contact as the main indication for the LTBI treatment, it was noted by in the SINAN forms that 58 (52.7%) patients had contact with TB cases, the majority being at the home (69.0%) and at work (6.9%). Thus, it becomes essential that the primary healthcare units, considered gateways to health services, promoting actions for the active search for these contacts. A Study carried out in Joao Pessoa-PB, Brasil, showed that only 47.2% of patients with TB, who reported previous contact with family members affected by the same disease, sought primary care for the diagnosis of the disease19.
Regarding clinical form of the index case was identified only two annotations in the form of pulmonary bacillus, without reference to other cases, which complicates the evaluation of contacts infected by Mbt.
CONCLUSION
Among the 110 LTBI notification forms of patients treated in the years 2009 and 2010, the majority corresponded to the male gender, white race and schooling 4-11 years of education. The indication of LTBI treatment occurred mainly for the contacts with TB, being adults or minors less than 10 years of age, ffor individuals with TB disease that predisposes (AIDS and diabetes) and by the use of immunosuppressive drugs.
Although the treatment with isoniazid has been full to the considerable number of cases, without distinction between the sexes, a large number of patients did not complete the treatment regimen, which puts this population at risk of developing tuberculosis in the future.
The average age of patients reported with LTBI was 34.8 years old, observing a high abandonment rate between the age ranges from 0 to 10 years and 11 to 20 years.
The analysis of the results shows that the answer to cases of LTBI needs better control, especially by strengthening the guidelines of adherence to treatment, the monitoring of cases and the search for culprits. The indication for treatment of LTBI as a measure of prevention of tuberculosis disease, prevents susceptible individuals and infected by Mbt evolve to severe forms of the disease, and to control the transmission cycle of the bacillus.
The identification and treatment of LTBI strategies are essential for the elimination of tuberculosis, and the professionals who work in primary care should be prepared to search for contacts throughout their coverage area.
REFERENCES
1.Sociedade Brasileira de Pneumologia e Tisiologia. III Diretrizes para tuberculose da Sociedade Brasileira de Pneumologia e Tisiologia. J Bras Pneumol. 2009;35:1018-48.
2. World Health Organization. Global tuberculosis control: WHO report 2011. Geneva (Swi): WHO; 2011.
3. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Manual de recomendações para o controle da tuberculose no Brasil. Brasília (DF): Editora MS; 2011.
4. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Guia de vigilância epidemiológica. 7a ed. Brasília (DF): Editora MS; 2009.
5. Chin J. Manual de controle das doenças transmissíveis. Tradução de Bolner Ane Rose. Porto Alegre (RS): Artmed; 2002.
6. Fiúza Melo FA, Afiune JB, Hijjar MA, Gomes M, Rodrigues DSS, Klautau GB et al. Tuberculose. In: Veronesi R, Focaccia R, editores. Veronesi: tratado de infectologia. 4a ed. São Paulo: Atheneu; 2009. v. 1, p.1263-328.
7. Belo MTCT, Luiz RR, Hanson C, Selig L, Teixeira EG, Chalfoun T et al. Tuberculose e gênero em um município prioritário no estado do Rio de Janeiro. J Bras Pneumol. 2010; 36(5):621-5.
8. Pineda NIS, Pereira SM, Matos ED, Barreto ML. Quimioprofilaxia na prevenção da tuberculose. J Bras Pneumol. 2004; 30: 485-95,
9. Sterling TR, Villarino ME, Borisov AS, Shang N, Gordin F, Bliven-Sizemore E et al. Three months os rifapentine and isoniazid for latent tuberculosis infection. N Engl J Med. 2011; 365(23): 2155-65.
10. Morrison J, Pai M, Hopewell PC. Tuberculosis and latent tuberculosis infection in close contacts of people with pulmonary tuberculosis in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2008; 8(6):359-68.
11. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Boletim epidemiológico do ministério da saúde especial tuberculose. 2012; 43 [Internet]. [citado em 12 jun 2012]. Available at: http://portal.saude.gov.br/portal/arquivos/pdf/bolepi_v43_especial_tb_correto.pdf
12. Santos TMMG, Nogueira LT, Santos LNM, Costa CM. O acesso ao diagnóstico e ao tratamento de tuberculose em uma capital do nordeste brasileiro. Rev enferm UERJ. 2012;20:300-5.
13. Siqueira KZ, Mendonça AS, Penedo CC. Indicação da prova tuberculínica e infecção latente da tuberculose em HIV-positivos, Município de Blumenau, Estado de Santa Catarina, Brasil, 2004-2009. Epidemiol Serv Saúde. 2012; 21: 635-44,
14. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Programa Nacional de DST e AIDS. Recomendações para terapia anti-retroviral em adultos infectados pelo HIV. 7ª ed. Brasília (DF): Editora MS; 2008.
15. Lopes DMA, Pinheiro VGF, Monteiro HSA, Queiroz JAN, Madeira LS, Lopes MMA. Diagnóstico e tratamento da tuberculose latente em pacientes com doenças inflamatórias crônicas e uso de imunobiológicos inibidores do TNF-α. J Bras Pneumol. 2011;37:308-16.
16. Silva DGST, Silva BDS, Junqueira-Kipnis AP, Rabahi MF. Tuberculose em pacientes com artrite reumatoide: a dificuldade no diagnóstico da forma latente. J Bras Pneumol. 2010;36:243-51.
17. Keane J. TNF- blocking agentes and tuberculosis: new drugs iluminate na old topic. Rheumatology (Oxford). 2005; 44(6):714-20.
18. Lima EVA, Lima MA, Duarte A, Marques C, Bernard G, Lorena V et al. Investigação de infecção tuberculosa latente em pacientes com psoríase candidatos ao uso de drogas imunobiológicas. An Bras Dermatol. 2011;86:716-24.
19. Trigueiro DRSG, Nogueira JA, Monroe AA, Sá LD, Anjos UU, Villa TCS. Determinantes individuais e utilização dos serviços de saúde para o diagnóstico da tuberculose. Rev enferm UERJ. 2013;21:371-8.
Recebido em: 02.04.2013
Aprovado em: 27.10.2013