RESEARCH ARTICLES
Risk factors associated with nasal injury by use of positive pressure device in newborns
Cândida Caniçali PrimoI; Maiara Soares BaratelaII; Maria Laura Pereira ValladaresIII; Sandra Cristina AlvarengaIV; Eliane de Fátima Almeida LimaV; Franciéle Marabotti Costa LeiteVI
INurse. Master in Collective Health. Professor of the Graduation and Master Degree Course in Nursing of the Federal University of Espírito Santo. Vitória, Espírito Santo, Brazil. E-mail: candidaprimo@gmail.com.
IINurse, graduated in the Federal University of Espírito Santo. Vitória, Espírito Santo, Brazil. E-mail: maiabaratela@hotmail.com.
IIINurse, graduated in the Federal University of Espírito Santo, Vitoria, Espírito Santo, Brazil. E-mail: mlaurinhapv@hotmail.com.
IVNurse. Coordinator of the Neonatal Intensive Therapy Unit of the University Hospital of the Federal University of Espírito Santo, Vitória, Espírito Santo, Brazil. E-mail: alvarengasandra@terra.com.br.
VNurse. Doctor degree in Nursing. Professor of the Graduation and Master Degree Course in Nursing of the Federal University of Espírito Santo. Vitória, Espírito Santo, Brazil. E-mail: elianelima66@gmail.com.
VINurse. Master degree in Collective Health. Professor of the Graduation and Master Degree Course in Nursing of the Federal University of Espírito Santo. Vitória, Espírito Santo, Brazil. E-mail: francielemarabotti@gmail.com.
ABSTRACT: This retrospective and descriptive study aimed at identifying risk factors associated with nasal lesions by the use of nasal CPAP in newborns at an intensive care unit of a university hospital, in Vitória, ES, Brazil. Sex, birth weight, gestational age, Apgar score, resuscitation, and hospital stay were variables related to the frequency of nasal lesions by the use of CPAP. The sample consisted of 122 newborns hospitalized from April, 2009 to April, 2010 and data was collected from medical records. It was observed that 19.7% of newborns had nasal injury related to variables as birth weight, gestational age, and length of hospitalization. Conclusions show that those variables affect injury by use of CPAP and that neonates in that condition require more care by nursing staff.
Keywords: Premature; nursing care; continuous positive airway pressure; newborn.
Currently, one of the main challenges of medicine is to overcome the serious neonatal problems characterized by pulmonary disorders, respiratory discomfort being one of the most frequent pathologies that affect premature, with an incidence of 3 to 7% in live births. Autopsies indicate that respiratory diseases are responsible for 32 to 52% of neonatal deaths1.
Due to pulmonary immaturity, most premature newborns aged less than 34 weeks, have respiratory failure degree that characterizes a pulmonary disorder and therefore require ventilatory assistance2.
The non-invasive ventilatory support created to benefit the premature, have as their main function to improve gas exchange and decrease the respiratory effort. One of these supporters is the nasal continuous positive pressure device (CPAP), which is a unit of ventilatory assistance with a positive pressure in the airways without interruption throughout the respiratory cycle with the purpose that the inspired gas is not completely eliminated providing a residual functional capacity maintenance, intra-alveolar pressure increases and provides stability, leading an improvement in gas exchange and avoiding the collapse of the alveoli. Thus, the CPAP system becomes an alternative much less invasive than mechanical ventilation3.
Given the above, this study aimed to know the risk factors associated with injuries through the use of nasal CPAP in newborns of a neonatal intensive care unit (NICU) of a university hospital.
LITERATURE REVISION
The CPAP was introduced by Gregory and collaborators in 1971 and first used in treatment of hyaline membrane disease. Later, in 1975, Kattwinkel and collaborators have demonstrated evidence that the CPAP was favorable on preventing and reducing the incidence of episodes of idiopathic apnea of prematurity. And in 1976, researchers Speidel and Dunn confirmed this use. Today, the applicability of this device has been expanded for the treatment of most lung diseases of respiratory distress in neonates and in situations such as meconium aspiration syndrome, in the postoperative period of cardiac surgery, in apnea of prematurity and the weaning of mechanical ventilation4.
The CPAP is a pressure of distention in the applied areas with few cmH2O usually through the nose and to lead to continue positive pressure there are five techniques being the two most commonly used: the water seal and the electronic fan. The CPAP in water seal is simple, cheap and easy to be adapted in newborns. The devise has a continuous flow of oxygen, mixed or not with compressed air source passing through a heated humidifier through a respiratory circuit and going to the newborn and then going into a vessel containing sterile distilled water, which is the water seal. The CPAP breathing with variable flow, in which the electronic fan modulates the positive end expiratory pressure valve (PEEP) and the flow of the circuit to maintain pressure5,6.
Among the most common devices using the nasal CPAP is prong consisting on an airway connection, due to the simple way of giving CPAP, since it is less invasive and produces recognizable therapeutic effects, but may present difficulties, as in the fixation on the patient's nostril, the loss of pressure during crying and the trauma of the nasal septum of the neonate6,7.
Nasal CPAP installation is the responsibility of the nurse and during installation he should be attentive to: gas flow monitoring; remove excess water from pipes; use the nasal prong with the appropriate size; aspire nostrils gently; instill saline every 2 hours; prong wash with soap and water daily; maintain adequate prong fixation; protect the septum; monitor parameters of pulse oximetry and provide comfort for the newborn. In this way, the nurse's assistance must be guided in a humanized through the use of technical and scientific knowledge and resources available to the reality of the population and the Institution3,8.
METHODOLOGY
This is a retrospective study, descriptive with quantitative approach, held at the NICU of a university hospital situated in the municipality of Vitória – Espírito Santo.
The population consisted of newborns admitted in this unit and the sample was composed for 122 newborns that made use of CPAP in the airways in the period of April 2009 to April 2010. Data collection took place in the period from October to November 2010, by research in clinical records, in which arose the following variables of newborns: sex, birth weight, gestational age, apgar of 1st and 5th minute of life, CPAP injury, neonatal resuscitation, length of hospitalization, pathological diagnosis and type of pathology.
A descriptive analysis was performed and examined the relationship between CPAP and injury characteristics of the newborns through the Chi-square test or Fisher's exact Test, as the variable. The significance level adopted was 5%, and we used the SPSS statistical package 15 (Social Package Statistical Science).
The study was approved by the Ethics and Research Committee of the Health Sciences Center of the Federal University of Espírito Santo, Prod. 194/10.
RESULTS AND DISCUSSION
In the study period were recorded 1106live births in the maternity of the University hospital, 26.58% with referral to the NICU and of these, 41.49% made use of CPAP and 11.03% of the total number of live births in the period, used CPAP. Of the 122 records examined, five were not located, amounting to a loss of 4% of the sample.
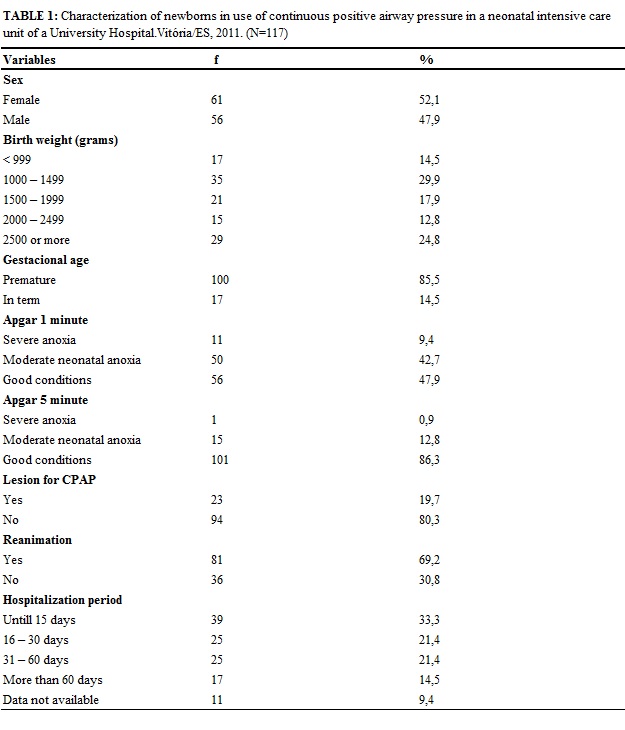
In table 1, there are displayed the variables of characterization of newborns in CPAP use.
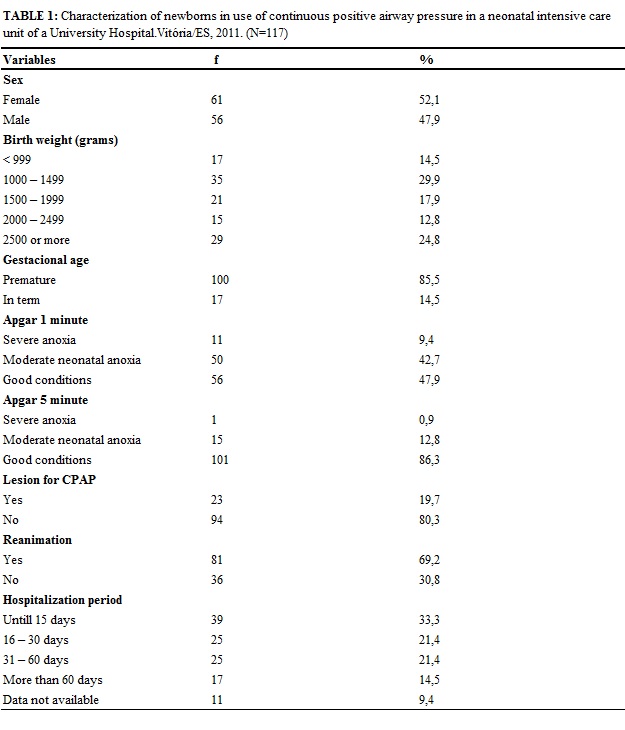
Corroborating the results of this research, cohort study conducted in Pelotas and Jardim América, claims that, in 2004, 4,558 children born in these municipalities, 52% were male and 48% female, resembling the proximity of birth between both sexes9. Another study conducted in Ohio in the United States, demonstrates this same proximity of numbers of live births of female and male genders, where 54% of the sample were male and 46% female10.
Newborns with birth weight between 1000 to 1499 grams (29.9%) prevailed, followed by 24.8% weighing 2500 grams or more. The birth weight is considered to be one of the most important features of the newborn and one of the major predictive factors for neonatal mortality, so it is a very variable used in epidemiological studies11.
The premature births are 85.5% and agreeing with these findings, a study with 180 newborns to three neonatal intensive care units of Atlanta in the United States, showed that the population of newborns more often placed on CPAP were premature, with an average of 32 weeks of gestational age12. A search also in NICU of Sao Paulo noted that newborns studied showed an average of 34 weeks gestational age and average weight greater than 1900g13.
Another study points out that most premature newborns tolerates the use of positive pressure continues in the airways, not requiring invasive ventilation, while newborns extremes, most often requires invasive ventilation14.
The Apgar score is used to assess the vitality in the 1st and 5th minute of birth, most of the births of this study consists of newborns in good condition of vitality, both in the first and in the fifth minute of life. It is worth mentioning that the apgar score at the 1° minute correlates with the ph of the blood from the umbilical cord and a possible intrapartum asphyxia, in the 5° minute apgar score less than seven, reflects an important suffocation and considerable chance of neurologic sequel15.
In this research, it was found that the newborns did not present 80.35% lesion and opposed to these findings, study in order to determine the frequency of nasal lesions in newborns by CPAP with prong in NICU of Maceió, noted that there were injuries in all (100%) of newborns, graduated in: lightweight (79.6%), moderate (19.7%) and severe (0.7%)3.
It was observed that 69.2% newborns were reanimated immediately after childbirth, 33.3% were hospitalized until 15 days and 21.4% from 16 to 30 days.
In table 2, there are the pathological diagnosis of newborns in use of CPAP.
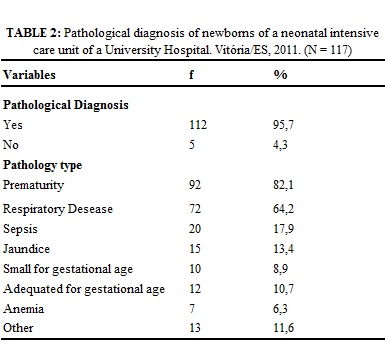
It was found that 95.7% of newborns had the presence of pathological diagnosis, 82.1% premature and 64.2% with some respiratory disease, such as: pneumonia, bronchiolitis, respiratory syndrome or 17.9% had sepsis and 13.4% jaundice. Confirming these findings, research shows that the premature neonates, due to pulmonary immaturity, need CPAP or another type of ventilatory support and newborns of extreme low birth weight are more prone to respiratory distress syndrome, thus needing more time in use of some kind of mechanical ventilation16,17.
Research of neonates in NICU, about inclusion of PICC, recorded that the most frequent clinical diagnoses were 79.1% prematurity, 67.6%, respiratory distress, 23.4% early twin pregnancy, 22.1% sepsis, 17.6%, cardiopathy and 14.8% gastrointestinal tract disorders13.
Variables are described and their association with presence or absence of injury CPAP in newborns, in table 3.
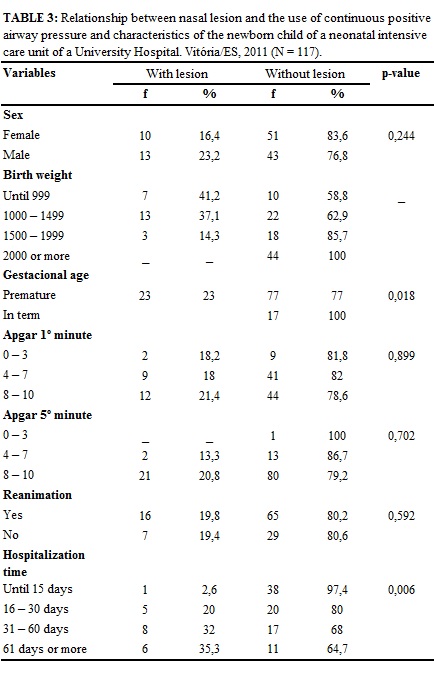
The newborns who have injury CPAP, 23.2% were male, 41.2% newborns with weight up to 999 grams, 37.1% with 1000 to 1499 grams, 23% premature newborn with apgar, of 1 and 5 minutes in good condition, 19.8% needed to be reanimated and 35.3% were hospitalized to 61 days or more, according to Table 3.
Variables: sex, apgar and resuscitation after applying the Chi-square test showed no statistical significance, which demonstrate that there is no association of these variables and the occurrence of injury by the use of CPAP. On the other hand, the results showed there is an association with significant value p <0.05 between occurrence of injury by using the CPAP and the variables: birth weight, gestational age and length of hospitalization.
Corroborating with these findings, a study notes that the weight variable has close relationship with gestational age noting that the lower the gestational age less than the weight of the newborn and bigger the chance of prolonged length of hospitalization since in extreme premature organs are underdeveloped and these need a longer time to care for the maturing of the organism16,17.
In addition, it was found similar data to our research, which sought to evaluate newborns in use of CPAP in NICU in the United States, demonstrating that the highest birth weight neonates, showed reduced period using CPAP12.
Agreeing with these findings, study in Maceió showed that 83.7% of newborns have using CPAP with prong had gestational age less than 37 weeks and 34.7 percent were underweight, proving that injury from use of prongs compromise more often premature and low-weight newborns3.
The time in use of non-invasive ventilation, such as CPAP, was significant regarding the evolution of the stages of nasal injuries, confirming the theory that the prolonged duration of CPAP with prong is a risk factor for the development of nasal trauma and injury6.
Although we have not found in the scientific literature, many works linking nasal lesions in newborns by use of CPAP in the airways with the variables described in this study, we identified that the scientific references emphasize that nasal complications are present mainly in newborns and premature and low birth weight, due to pulmonary immaturity, thus necessitating early CPAP and correlated to other factors such as: the size of the attachment type of the prong, prong wear, the size of the cap or beanie, among others3,6.
In addition, it is necessary to discuss the issues about the care provided to newborns in CPAP use, as they may be associated with increased frequency of injury. Such propositions are discussed in study on nursing care for the use of nasal CPAP and concluded that to be used without appropriate remarks, the CPAP can be a complicating the process of restoring health and quality nursing care offered to newborn19.
Research evaluating the knowledge of nursing staff about the use of CPAP, the complications and interventions carried out noted that the most frequently cited complications were: necrosis of nasal septum, irritation and discomfort and, among the interventions carried out, it became clear: aspiration of airway and proper positioning of the newborn. Thus, it was concluded that knowledge of nursing staff about the complications of CPAP usage was limited to the effects more prevalent in healthcare practice, although the technicians have pointed to greater diversity of complications20.
CONCLUSION
This study found that 19.7% of newborns in using CPAP nasal injury and had identified the variables: birth weight, gestational age and length of hospitalization as risk factors associated with injuries through the use of nasal CPAP in newborns of NICU.
The CPAP is a good alternative for non-invasive ventilatory therapy for premature newborns, however, its potential complications will be found more often, so it is imperative that the nursing staff is attentive in the installation and maintenance of nasal CPAP, in order to avoid further complications to these newborns.
This research contributes to the development of nursing, because to know the variables that were associated with the development of injury by use of CPAP in newborns can assist in the targeting of assistance provided by the nursing staff in the care of newborns, but also assist the nurse in the elaboration of protocols and training of nursing staff, given that these newborns are more fragile by requiring a larger and more frequent attention.
In order to reduce the incidence of injury by use of CPAP, it is suggested the holding of training courses in neonatology to subsidize the theoretical-practical contribution and to assist in improvement of performance in professional service.
REFERENCES
1. Malik RK, Grupta RK. A two year experience in continuous positive pressure ventilation using nasal prongs and pulse oximetry. Mjafi. 2003; 59 (1):36-9.
2. Ferreira S, Nogueira C, Conde S, Taveira N. Ventilação não invasiva. Rev Port Pneumol. 2009; 15: 655-67.
3. Nascimento RM, Ferreira ALC, Coutinho ACFP, Veríssimo RCSS. Frequência de lesão nasal em neonatos por uso de pressão positiva contínua nas vias aéreas com pronga. Rev Latino-Am Enfermagem. 2009; 17: 489-94.
4. Carvalho WB, Horigoshi NK. Conceitos básicos e contra indicações da VNIPP. In: ventilação não invasiva em neonatologia e pediatria. São Paulo: Editora Atheneu; 2007.
5. Morley C. Which neonatal nasal CPAP device should we use in babies with transient tachypnea of the newborn? J. Pediatr. [Scielo-Scientific Electronic Library Online]. 2011[cited 2014 Jan 10]; 87: 466-8. Available at: http://www.scielo.br/pdf/jped/v87n6/v87n06a02.pdf
6. Alves MA, Santos ERS, Souza TG. Prevenção de lesões nasais secundárias ao uso de pressão positiva contínua nas vias aéreas (CPAP) em recém- nascidos prematuros de extremo baixo peso. Revista da Universidade Vale do Rio Verde. [Internet] 2013 [citado em 2014 10 jan]; 11(2): 209-17. Available at: http://revistas.unincor.br/index.php/revistaunincor/article/view/1109/pdf_56
7. Rocha E, Carneiro EM. Benefícios e complicações da ventilação mecânica não-invasiva na exacerbação aguda da doença obstrutiva crônica. Rev bras ter intensiva. 2008; 20(2): 184-9.
8. Antunes JCP, Nascimento MAL, Gomes AVO. Instalação do cpap nasal: identificando a dor do recém-nato como um cuidado de enfermagem. Rev Enferm UFPE [Internet]. 2010; [citado em 20 mai 2012]. 4: 142-8. Available at: http://www.ufpe.br/revistaenfermagem/index.php/revista/article/viewFile/592/pdf_304
9. Barros AJD, Santos IS, Victora CG, Albernaz EP, Domingues MR, Timm IK et al. Coorte de nascimentos de Pelotas, 2004: metodologia e descrição. Rev Saude Publica [Scielo-Scientific Electronic Library Online]. 2006; [citado em 20 mai 2012] 40: 402-13. Available at: http://www.scielo.br/pdf/rsp/v40n3/07.pdf
10. Jatana KR, Oplatek A, Stein M, Phillips G, Kang DR, Elmaraghy CA. Effects of nasal continuous positive airway pressure and cannula use in the neonatal intensive care unit setting. Arch Otolaryngol Head Neck Surg. 2010; 136(3):287-91.
11. Magalhães MC, Carvalho MS. Atenção hospitalar perinatal e mortalidade neonatal no município de Juiz de Fora, Minas Gerais. Rev Bras Saude Mater Infant. 2003; 3(3): 329-37.
12. Stoeri AL. Correlational study for predictor variables affecting duration on bubble CPAP [tese]. Georgia (USA): Georgia State University; 2009.
13. Costa P, Vizzotto MPS, Olivia CL, Kimura AF. Sítio de inserção e posicionamento da ponta do cateter epicutâneo em neonatos. Rev enferm UERJ . 2013; 21: 452-7.
14. Yong SC, Chen SJ, Boo NY. Incidence of nasal trauma associate with nasal prong versus nasal mask during continuous positive airway pressure treatment in very low birthweight instants: a randomized control study. Arch Dis Child Fetal Neonat. 2005; 90:480-3.
15. Aly H, Massaro AN, Patel K, El-Mohandes AA. Is it safer to intubate premature infants in the delivery room? Pediatrics. 2005; 115:1660-5.
16. Ribeiro AM, Guimarães MJ, Lima MC, Sarinho SW, Coutinho SB. Fatores de risco para mortalidade neonatal em crianças com baixo peso ao nascer. Rev Saude Publica [Scielo-Scientific Electronic Library Online] 2009 [citado em 10 mai 2012]; 43: 246-55. Available at: http://www.scielo.br/pdf/rsp/v43n2/6833.pdf
17. Nascimento RM do, Leite AJM, Almeida NMG, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad. Saude Publica [Scielo-Scientific Electronic Library Online]. 2012 [citado em 14 fev 2014]; 28: 559-72. Available at: http://www.scielo.br/pdf/csp/v28n3/16.pdf
18. Araújo BF, Zatti H, Madi JM, Coelho MB, Olmi FB, Canabarro CT. Análise da morbiletalidade neonatal em recém-nascidos pré-termo tardios. J Pediatr. [Scielo-Scientific Electronic Library Online]. 2012 [citado em 13 fev 2014]; 88: 259-66. Available at: http://www.scielo.br/pdf/jped/v88n3/v88n03a13.pdf
19. Antunes JCP, Nascimento MAL, Gomes AVO, Araujo MC, Christoffel MM. Tecnologia coadjuvante no tratamento do recém-nato prematuro: cuidados de enfermagem no uso do Cpap nasal. Enfermeria Global. 2010; 20: 1-11.
20. Silva1 DM, Chaves EMC, Farias LM, Lélis ALPA. Uso de pressão positiva contínua das vias aéreas em recém-nascidos: conhecimento da equipe de enfermagem. Rev RENE. 2010; 11:195-203