(*) CI: Confidence Interval
ORIGINAL RESEARCH
Hepatitis B in nursing professionals: prevalence and occupational risk factors
Laís Queiroz MoraisI; Ana Rita Coimbra Motta-CastroII; Oleci Pereira FrotaIII; Luciana Contrera IV; Paula Renata Tedesco de CarvalhoV; Fernanda Rodas Pires FernandesVI
I
Nurse. Master. Public Health of Três Lagoas. Mato Grosso do Sul, Brazil.
E-mail: lais_morais@hotmail.com
II
Pharmacist. PhD. Adjunct Professor, Federal University of Mato Grosso do
Sul. Campo Grande, Brazil. E-mail: anacastro@fiocruz.br
III
Nurse. PhD. Adjunct Professor, Federal University of Mato Grosso do Sul.
Campo Grande, Brazil. E-mail: olecifrota@gmail.com
IV
Nurse. PhD. Adjunct Professor, Federal University of Mato Grosso do Sul.
Campo Grande, Brazil. E-mail: l.contrera@ufms.br
V
Nurse. Master. Hospital Universitário Maria Aparecida Pedrossian, Federal
University of Mato Grosso do Sul. Campo Grande, Mato Grosso do Sul, Brazil.
E-mail: tedesco.pr@gmail.com
VI
Pharmacist. Master. Ministry of Agriculture, Livestock and Supply.
Laboratory diagnosis of viral diseases. Minas Gerais, Brazil. E-mail: ferodas@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.11143
ABSTRACT
Objectives: to estimate the prevalence of infection by Hepatitis B Virus (HBV) among nursing staff at a university hospital and to investigate related occupational risk factors. Method: this descriptive, exploratory study was performed at a large public hospital in Campo Grande, Mato Grosso do Sul, Brazil. From 2011 to 2012, 275 nursing professionals, including nurses (n=40), nursing technicians (n=113) and nursing auxiliaries (n=122), were interviewed and underwent blood sampling for detection of serological markers of HBV infection by Enzyme-Linked Immunosorbent Assay (ELISA). Results: overall prevalence of HBV infection was 11.6% (CI 95%: 0.1-0.6). The isolated anti-HBs marker, suggesting vaccine immunity, was detected in 63.7% of participants. Conclusion: it is necessary to implement effective strategies for designing diagnostic, education, prophylactic and healthcare measures for the prevention and control of HBV infection in these professionals.
Keywords: Occupational health; risk factors; Hepatitis B vaccines; biological markers.
INTRODUCTION
Infection with hepatitis B virus (HBV) is one of the most serious problems of contemporary public health worldwide, given the high number of people infected by this etiological agent and the negative consequences for the individual, family, community and public system. The World Health Organization (WHO) reports that there are approximately 240 million chronic carriers of this virus in different regions of the world, and of these, about two million are concentrated in Brazil1.
In health field, depending on the organizational conditions of the working environment, human and material resources, institutional policies, among others, nursing professionals are the most likely workers to be exposed to blood and other biological fluids capable of transmitting infections, such HBV. This high number of exposures due to the fact that these professionals are in greater number in hospitals provide direct care and remain longer with the patient than any other professional category, besides the high frequency of nursing procedures that are performed with the patient in the nosocomial environment2.
The overall prevalence of HBV infection varies from 4.8 to 11.1% in health workers, and may be up to three times greater than the general population. This can be justified by the high risk of occupational exposure, which can reach up to 40% of prevalence in the case of percutaneous exposure, in which the source-patient is positive to the serologic marker HBsAg 3. Occupational risk after an exposure to biological material is variable and depends on the type of accident and other factors such as size of the lesion, presence and involved blood volume, in addition to the source-patient's clinical condition and correct use of post-exposure prophylaxis4.
Immunization against hepatitis B by administration of three sequential doses of Hepatitis B vaccine is the most efficient prevention measure. It is commercially available since 1982 and has been recommended to health care workers since then5. Despite improvements in vaccine coverage in Brazil and the increasing information about the importance of vaccines and their availability in public services, studies3,5,6 have shown that vaccination against hepatitis B and adherence to strategies aimed at seroconversion are below the expected among nursing professionals in different scenarios. Thus, there is need of investment in educational and preventive actions, in addition to monitoring of vaccination status in order to reduce the number of susceptible individuals and thus reduce the risk of transmission from patients to professionals and vice versa. It is also important to conduct studies aimed at situational diagnosis, an essential step for the development of interventions guided by the local reality5.
Based on these, this study aimed to estimate the prevalence and to investigate the risk factors associated with HBV infection among nursing professionals at a university hospital in Campo Grande, Mato Grosso do Sul.
LITERATURE REVIEW
Hepatitis is a severe liver inflammation that results in degeneration and necrosis of hepatocytes. Roughly, the etiology may be of two types: infectious or toxic. Infectious hepatitis is caused by different viruses that present different epidemiological, clinical and laboratory characteristics. Toxic hepatitis results from nutritional deficiencies, blood deficiencies, alcoholism or allergic reactions to chemicals present in some drugs7.
Viral hepatitis has been a serious public health problem in Brazil and worldwide. It is caused by various etiological agents (hepatitis A, B, C, D, E viruses) that have the primary tropism by liver tissue as a common feature8. The overwhelming importance of HBV infection is due to its wide geographic distribution, high potential to chronicity, in addition to high morbidity and mortality (cirrhosis and hepatocellular carcinoma) 9. Among the main HBV transmission routes, there is highlight for: unprotected sex; dental and surgical interventions, hemodialysis, tattoos, ear piercings without proper sterilization or use of disposable materials; drug use with sharing syringes, needles or other equipment; contaminated blood and blood products transfusion; vertical transmission (mother/child); breastfeeding and occupational accidents2.
Although vaccination is the most effective prevention measure, it is not a panacea, because there are people who are hypo-responders (5-10% among immunocompetent adults and up to 50% of immunocompromised adults), which makes it necessary to investigate the immune status to make sure about the proper immunization (seroconversion), besides providing to the professional greater certainty as to their susceptibility. To this end, there is the anti-HBs serologic test, which is a serological test that can confirm the development of sufficient antibodies against HBV in the individual. Thus, the anti-HBs is the marker used to control the efficacy of the vaccine program. A suitable vaccine response must have reactive anti-HBs antibodies through ELISA serological technique that quantitatively should be greater than 10 mUI/ml6.
METHODOLOGY
This is a descriptive study of quantitative approach. It was performed at the Maria Aparecida Pedrossian University Hospital, of the Federal University of Mato Grosso do Sul, which is a large public hospital located in Campo Grande, Mato Grosso do Sul, Brazil. Participants were 275 nursing professionals, of whom 40 (14.5%) were nurses, 113 (41.1%) were nursing technicians and 122 (44.4%) were nursing assistants from different sectors, from September 2011 to December 2012. After a brief explanation about the research, all professionals who agreed to participate by signing the Informed Consent Form underwent systematic interview, blood collection and vaccination against hepatitis B, when appropriate.
All collected samples were subjected to detection of markers of hepatitis B virus infection, such as the surface antigen (HBsAg), the total antibody against the core antigen (anti-HBc) and the antibody against the surface antigen (anti- HBs), determined by the Enzyme-Linked Immunosorbent Assay (ELISA), by using commercial kits ( Hepanostika HBsAg Ultra, Biomerieux, Murex anti-HBc total, Abott Murex; Imunoelisa anti-HBsAg Wama diagnostica ). Nursing professionals with initially reactive results were submitted to the new collection and the sera were retested in duplicate.
Data from the questionnaires and the results of serological tests were entered in a personal computer and analyzed by Epiinfo statistical program (Centers for Disease Control and Prevention, 2008). Prevalence and geometric mean of anti-HBs, HBsAg and anti-HBc titles were calculated with 95% confidence interval. Initially, researchers estimated the odds of seropositivity to HBV (HBsAg and/or anti-HBc) associated with the risk factors investigated. Factors that were significantly associated (p <0.05) were submitted to binomial logistic regression analysis by using the Statistical Package for Social Science, version 20.0 (SPSS). The Fisher's exact test was used when appropriate.
Ethical aspects recommended by Resolution No. 466/12 of the National Health Council regarding research involving human beings were respected. The project that gave rise to this study was approved by the Ethics Committee on Human Research of the Federal University of Mato Grosso do Sul under Protocol No. 2154/2011.
RESULTS AND DISCUSSION
Characteristics of the study population
Researchers interviewed 275 nurses, of whom 205 (74.5%) were female and 70 (25.5%) were male. The age of participants ranged from 25 to 64 years (mean 45.5). Most were white (57.8%), followed by brown (31.6%) and black (8.4%). Regarding marital status, 151 (55%) lived with a partner and 124 (45%) had no partner. As for the level of education, the majority of participants (60.4%) reported having 13 years of study or more.
HBV infection and risk factors associated
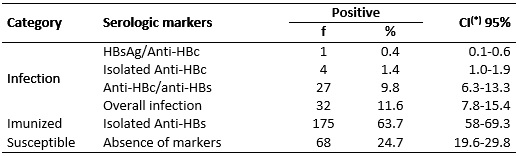
The overall prevalence of HBV infection in the population studied was 11.6% (CI: 95%: 0.1-0.6). The positive result for HBsAg was 0.4% (1/275; CI: 95%: 0.1-0.6). The seropositive sample for HBsAg was negative anti-HBc IgM, negative HBeAg and positive anti-HBeAg. The total anti-HBc marker associated with anti-HBs was detected in 27 (9.8%) of the nursing professionals and the isolated anti-HBc was found in 4 of them (1.4%). The presence of isolated anti-HBs, suggesting immunity to HBV vaccine was detected in 175 (63.7%) participants. Of these, 31 (18%) were nurses, 72 (41%) were nursing technicians and 72 (41%) were nursing assistants. However, 68 (24.7%) of the sample showed no marker of HBV infection, which characterizes susceptibility to the infection. See Table 1.
TABLE 1:
Prevalence of serological markers of HBV infection among nursing staff.
Campo Grande, MS, 2012. (N=275)
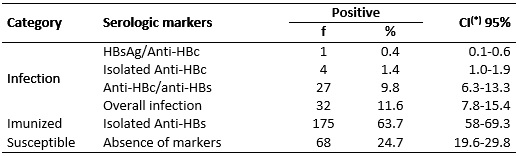
(*) CI: Confidence Interval
In the binomial probability analysis of the risk factors studied, increased age (OR: 1.08; 95% CI: 1.02-1.14), longer time of nursing exercise (OR: 1.73; 95% CI: 1.02 - 2.92), history of blood transfusion (OR: 6.41; 95% CI: 1.53-6.83) and history of work accident (OR: 1.08; 95% CI: 1.02 -1.14) were significantly associated with HBV infection in the population studied, according to Table 2.
TABLE 2:
Binomial analysis of risk factors for hepatitis B virus in exposed nursing
professionals (overall infection+susceptible ones). Campo Grande, MS, 2013.
(N=100)
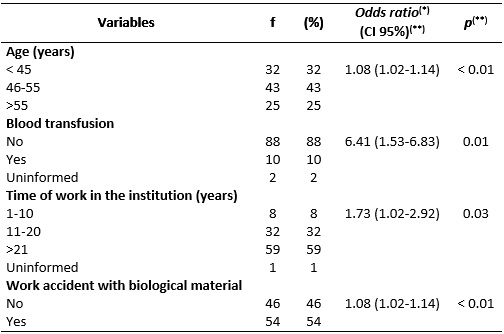
(*)Estimated by binomial logistic regression; (**)CI: Confidence interval;
(***)Fisher's exact test
Nursing professionals are among the population groups at high risk of exposure to HBV infection due to the professional activities they perform. The risk of HBV infection is directly related to several factors: type of procedures performed, frequency of exposure to biological materials, prevalence of infection in the assisted population and last but not least, occupational conditions intrinsic to the institution and profession10.
The nursing profession is performed by different categories of workers, recognized by professional legislation. Each of the professional categories (nursing assistant, nursing technician and nurse) has its own training process, which establishes a distinct set of activities11. However, there is a predominance of nursing assistants and technicians in hospitals12,13, as confirmed in this study.
The overall prevalence of HBV infection in 11.6% of this research sample was two times higher than the prevalence found in a population-based study, also conducted in the Midwest Region, whose global prevalence of HBV infection was 5.3 %14. Studies conducted in the Mato Grosso do Sul State with various other professional categories at risk of HBV infection found lower results15,16. This suggests that the exercise of nursing in hospitals is an associated factor to the risk of occupational HBV infection, probably due to the higher number of invasive risk procedures performed in routine and emergency situation, the longer time spent with the patient and the high frequency of exposure to body fluids potentially contaminated with HBV.
In Brazil, few studies have been conducted specifically about nursing professionals, since most of the works reports the prevalence of HBV infection in health care workers in general. In relation to the studies conducted in Brazil, a research conducted in Natal, Brazil (23.6%) among nursing professionals had higher results than those found in this study17. Similar results were found in the cities of Sao Jose do Rio Preto (9.4%)18 and Salvador (8.8%)19, with health professionals in general, and specifically with dental surgeons (10.8%)20 and primary health care professionals (11.1%) in Mato Grosso do Sul State21.
Regarding research conducted with health professionals in other countries, the result of the present study was also higher than, for example, the study in tertiary hospitals in Pakistan, which showed 2.18% of prevalence for HBV22. On the other hand, it was lower than that found in studies that showed 18.7% and 16.4% prevalence of HBV infection among nursing professionals in Turkey23 and in Poland24, respectively.
Low positive results for HBsAg (0.4%) was similar to a population-based study conducted in the Midwest Region14, confirming the low endemicity for HBV in this region. Higher results for this marker (HBsAg) were found in other studies conducted with nursing professionals23,25,26.
Approximately 25% of the studied subjects showed no marker of infection for Hepatitis B. It is known that the most effective measure against hepatitis B, in the hospital environment, is the active immunization of health professionals, but even so, the adherence of participants to the full vaccination schedule against hepatitis B was not satisfactory, proving the need to implement health promotion strategies to improve immunization coverage among these professionals27-29.
Older age, time of work in nursing at the institution≥21 years, history of blood transfusion and history of accident with biological material were significantly associated with HBV infection. The first two are supported in the literature30,31 and they are possibly related to overconfidence and safety in work routine, which leads to underestimating the risks32. The other findings are not recorded in the surveys consulted by the authors of this study as factors associated with HBV infection in nursing professionals.
The rates of HBV infection secondary to blood transfusions have reduced more than 1,000 times compared to 50 years ago. This is due to the development of antigen tests increasingly sensitive to Hepatitis B (HBsAg), the adoption of the screening of HBV core antigen (anti-HBc), the improvement in donor selection procedures, HBV vaccination programs, among others33. Currently, the risk of acquiring HBV associated with blood transfusion is about 1: 500,000 to 1: 1,000,00034. For this reason, this risk factor is not found in similar studies.
The risk factor history of accident with biological material presupposes that such professionals have behaviors, beliefs and/or attitudes that increase the risk of exposure to pathogens. Thus, this group of professionals deserves greater attention and investment by the institution, occupational health - especially the occupational nurse - and hospital infection control service: continuing education, ongoing monitoring, supervision and guidance, as well as quantitative and qualitative adequacy of human and material resources according to evidence-based practices.
Although this study had been conducted in a single reference hospital, not representing, therefore, all hospitals in the region, the information obtained in this study are important for the development and intensification of effective strategies for the design of administrative, preventive, diagnostic, educational and care actions for the prevention and control of HBV infection among these professionals.
CONCLUSION
The results of this study indicate a high prevalence of HBV infection, suggesting that the nursing practice in the hospital environment is a risk factor for occupational infection. Nursing professionals with more time of work and older age, with history of accident with biological material and history of blood transfusion are more susceptible to HBV infection. There was insufficient seroconversion rate (isolated anti-HBs). Some risk factors are related to overconfidence, underestimation of risks, behaviors or beliefs.
REFERENCES
1.Simão SAF, Soares CRG, Souza V, Borges RAA, Cortez EA. Acidentes de trabalho com material perfurocortante envolvendo profissionais de enfermagem de unidade de emergência hospitalar. Rev enferm UERJ. 2010; 18(3):400-4.
2.Lima BFL, Waffae MC, Figueiredo EN, Filipinni R, Luz MCB, Azzalis LA, et al. Occupational infection by the hepatitis b virus: risk and prevention measures. Journal of Human Growth and Development. 2013; 23(2):184-89.
3.Costa FM, Martins AMEBL, Santos Neto PE, Veloso DNP, Ferreira RC. Is vaccination against hepatitis B a reality among Primary Health Care workers? Rev Latino-Am Enfermagem. 2013; 21(1):316-24.
4.Ministério da Saúde (Br). Coordenação Geral de Saúde do Trabalhador. Exposição a materiais biológicos. Brasília (DF): Ministério da Saúde; 2011.
5.Oliveira VC, Guimarães EAA, Souza DAS, Ricardo RA. Situação vacinal e sorológica para Hepatite B em profissionais da estratégia saúde da família. Rev Rene. 2011; 12(4):960-65.
6.Pinheiro J, Zeitoune RCG. O profissional de enfermagem e a realização do teste sorológico para Hepatite B. Rev enferm UERJ. 2009; 17(1):30-4.
7.Rossi GC, Afonso PMD, Oliveira SLG, Furlan MLS. Hepatites B e C: o conhecimento dos estudantes universitários da área da saúde. Rev enferm UERJ. 2010; 18(1):38-41.
8.Araújo TME, Sá LC, Santos AS, Faustino SKM, Tapety FI, Mesquita GV. Prevalência da Hepatite B em usuários do laboratório central do Piauí. Rev enferm UERJ. 2012; 20(2):229-34.
9. Pessôa IN, Vasconcellos MP. Aproximações do cotidiano de pessoas com Hepatite B. Rev enferm UERJ. 2013; 21(3):343-8.
10. Piratheepkumar V, Kulendran S, Nadarajah S, Murugananthan K. Hepatitis B vaccine immunogenicity among nurses of a hospital. Ceylon Med J. 2014; 59(2):59-60.
11.Nicola AL, Anselmi ML. Dimensionamento de pessoal de enfermagem em um hospital universitário. Rev Bras Enferm. 2005; 48(2):186-90.
12.Frota OP, Ferreira AM, Loureiro MDR, Cheade MFM, Reis MG. O uso de equipamento de proteção individual por profissionais de enfermagem na aspiração endotraqueal. Rev enferm UERJ. 2012; 20(esp. 1):625-30.
13.Padilha MICS, Vagheti HH, Brodersen G. Gênero e enfermagem: uma análise reflexiva. Rev enferm UERJ. 2006; 14(2):292-300.
14.Pereira LMMB, Martelli CMT, Merchán-Hamann E, Montarroyos UR, Braga MC, De Lima MLC, Et al. Population-based multicentric survey of hepatitis B infection and risk factor differences among three regions in Brazil. Am J Trop Med Hyg. 2009; 81(2):240-7.
15.Contrera-Moreno L, Andrade SMO, Pontes ERJC, Stief ACF, Pompilio MA, Motta-Castro, ARC. Hepatitis B vírus infecction in a population exposed to occupational hazards: firefighters of a metropolitan region in central Brasil. Rev Soc Bras Med Trop. 2012; 45(4): 463-7.
16.Mousquer, GJ. Infecção pelo vírus da hepatite b em mulheres profissionais do sexo em Campo Grande, Mato Grosso do Sul [master degree]. Campo Grande (MS): Universidade Federal de Mato Grosso do Sul; 2011.
17.Fernandes JV, Braz RFS, Neto FVA, Costa NF, Ferreira AM. Prevalência de marcadores sorológicos do vírus da hepatite B em trabalhadores do serviço Hospitalar. Rev Saude Publica. 1999; 33(2):122-8.
18.Ciorclia LAS, Zanetta DMT. Hepatitis B in healthcare workers: prevalence, vaccination and relation to occupational factors. Braz J Infect Dis. 2006; 9(5):274-89.
19.Carvalho P, Schinoni MI, Andrade J, Rego, MAV, Marques P, Meyer R et al. Hepatitis B virus prevalence and vaccination response in health care workers and students at the Federal University of Bahia, Brazil. Ann Hepatol. 2012; 11(3):330-7.
20.Batista SMF, Andreasi, MAS, Borges, AMT, Lindenberg, ASC, Silva AL, Fernandes TD et al. Seropositivity for hepatitis B virus, vaccination coverage, and vaccine response in dentists from Campo Grande, Mato Grosso do Sul, Brazil. Mem Inst Oswaldo Cruz. 2006; 101(3):263-7.
21.Sanches GBS, Honer MR, Pontes ERJC, Aguiar JI, Ivo ML. Caracterização soroepidemiológica da infecção pelo vírus da hepatite B em profissionais de saúde da atenção básica no Estado de Mato Grosso do Sul, Brasil. Rev Panam Infectol. 2008; 10(2):17-22.
21.Attaullah S, Khan S, Naseemulla; Ayaz S, Khan SN, Ali et al. Prevalence of HBV and HBV vaccination coverage in health care workers of tertiary hospitals of Peshawar, Pakistan. J Clin Virol. 2011; 8: 275.
23. Kosgeroglu N, Ayranci U, Vardareli E, Dincer S. Occupational exposure to hepatitis infection among Turkish nurses: frequency of needle exposure, sharps injuries and vaccination. Epidemiol Infect. 2003; 132(1):27-33.
24.Ganczak M, Ostrowski M, Szych Z, Korzen M. A complete HBV vaccination coverage among Polish surgical nurses in the light of anti-HBc prevalence: a cross-sectional sero-prevalence study. Vaccine. 2010; 28(23):3972-6.
25.Shin BM, Yoo HM, Lee AS. Park SK. Seroprevalence of Hepatitis B Virus among Health Care Workers in Korea. J Korean Med Sci. 2006; 21(1):58-62.
26.Djeriri K, Laurichesse JL, Merle JL, Charof R, Abouyoub, A, Fontana L. et al. Hepatitis B in Moroccan health care works. Occup Med. 2008; 58(6):419-24.
27.Silva PA, Fiaccadori FS, Borges AMT, Silva AS, Daher RRR, Martins RMB. Seroprevalence of hepatitis B virus infection andseroconvertion to anti-HBsAg in laboratory staff in Goiânia, Goiás. Rev Soc Bras Med Trop. 2005; 38(2):153-6.
28.Gir E, Caffer Netto J, Malaguti SE, Canini SRMS, Hayashida M, Machado AA. Accidents with biological material and immunization against hepatitis b among students from the health area. Rev Lat-Am Enfermagem. 2008; 16(3):401-6.
29.Hatipoglu CA, Yetkin MA, Ergin F, Ipekkan K, Erdinc FS, Bulut C et al. Vaccination of healthcare workers against hepatitis B virus in a teaching hospital. J Hosp Infect. 2007; 67(2):200-2.
30. Motta-Castro ARC, Martins RMB, Yoshida CFT, Teles AS, Paniago AM, Lima KMB et al. Hepatitis B virus infection in isolated Afro-Brazilian communities. J Med Virol. 2005; 77(2):188-93.
31. Tatsilong HOP, Noubiap JJN, Nansseu JRN, Aminde LN, Bigna JJ, Ndze VN, et al. Hepatitis B infection awareness, vaccine perceptions and uptake, and serological profile of a group of health care workers in Yaoundé, Cameroon. BMC Public Health. 2016; 16:706.
32. Frota OP, Loureiro MDR, Ferreira AM. Open system endotracheal suctioning: practices of intensive care nursing professionals. Esc Anna Nery. 2014; 18(2):296-302.
33. Franco E, Bagnato B, Marino MG, Meleleo C, Serino L, Zaratti L. Hepatitis B: epidemiology and prevention in developing countries. World J Hepatol. 2012; 4(3):74-80.
34. Lindenberg Ade S, Motta-Castro AR, Puga MA, Ortiz Tanaka TS, Torres MS, Fernandes-Fitts SM, et al. Decrease in hepatitis B prevalence among blood donors in Central-West Brazil. J Venom Anim Toxins Incl Trop Dis. 2013; 19(1):7.