Source: medical records of newborns in the NICU
ORIGINAL RESEARCH
Profile of newborns with extremely low birth weight in a northeastern Brazilian city
Bruna Borges SantosI; Juliana de Oliveira Freitas MirandaII; Deisy Vital dos SantosIII; Climene Laura de CamargoIV; Carlito Lopes Nascimento SobrinhoV; Darci de Oliveira Santa RosaVI
INurse. Graduated by the State University of Feira de Santana - Bahia.
Email: brunasantos23@hotmail.com
IIPhD Student in Nursing. Professor at the State University of Feira de
Santana - Bahia. Email: julidefreitas@hotmail.com
IIIPhD Student in Nursing. Professor at the Federal University of Reconcavo
da Bahia. Email: deisy@ufrb.edu.br
IV
PhD in Public Health. Professor at the School of Nursing of the Federal
University of Bahia. Email: climenecamargo@hotmail.com
VDoctor in Medicine and Health. Professor at the State University of Feira
de Santana - Bahia. Email: mon.ica@terra.com.br
VIPhD in Nursing. Professor at the School of Nursing of the Federal
University of Bahia. Email: darcisantarosa@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.10825
ABSTRACT
Objective: to describe the profile of extremely low-birth-weight newborns in neonatal intensive care units (ICUs) in Feira de Santana, Bahia. Method: this descriptive study used documentary research in 64 medical records of newborns admitted to the city's three neonatal ICUs in 2012. Absolute and relative frequency measures and case fatality rate were calculated. Results: conspicuous were the number of teenage mothers (35.9%), resuscitation applied in the delivery room (67.2%), high incidence of perinatal asphyxia (51.6%) and sepsis (60.9%), and high cumulative case fatality (78.2%). Conclusion: the profile of this population showed that problems such as perinatal asphyxia, sepsis and case fatality were high in the neonatal ICUs of Feira de Santana, even with access to high-complexity care.
Keywords: Newborns; low birth weight; neonatology; intensive care units neonatal.
INTRODUCTION
Premature newborns (NBs) and babies with very low birth weight (VLBW), born with 500 to 1,500 grams, are subject to various morbidities such as perinatal asphyxia, respiratory distress syndrome (RDS), infections and others. The hospitalization time is extended and may result in complications. These conditions make them more vulnerable to death1,2.
There are few published studies on the profile of morbidity and mortality of NBs with extremely low birth weight (NBELBW), that is, less than 1,000 g. Usually, this group is included in studies of NBs with very low birth weight (NBVLBW), defined by the World Health Organization (WHO) as weigh values below 1,500 g. The morbidity of NBVLBW contributes significantly to infant mortality and to the occurrence of consequences and may lead to a poor quality of life of these children3.
Since the year of 2000, policies for newborn health have been the focus of the Ministry of Health. These has been represented by initiatives such as the Program for Humanization of Prenatal and Birth, the Standards for Humanized Care to Newborns with Low Birth Weight and the Stork Network, all with common features aimed at offering better conditions in the monitoring of pregnancy, delivery and birth up to the first years of life of children4,5.
The city of Feira de Santana, the largest city of the countryside of Bahia, inaugurated its first neonatal intensive care unit (NICU) in 2005 when there was an investment from federal and state governments to the implementation of neonatal units in the state. Since then, three public NICUs have been installed, two are state institutions and one is a municipal institution.
In this context and in order to obtain a diagnosis to know the actual health situation of NBELBW in the municipality, the aim of this study was to describe the profile of NBELBW hospitalized in NICUs of Feira de Santana, Bahia.
LITERATURE REVIEW
The extremely low birth weight (LBW) is one of the determinants of infant mortality and of the morbidity of psychomotor development of children. Growing evidence shows that these children have developed neurobehavioral problems, even when cerebral palsy does not occur, and such problems are observed up to adolescence, becoming a major public health problem and theme of several studies6.
Technological evolution has been essential to increase the survival rates of these NBs. In the early days of neonatology, care to premature neonates consisted of the warming, careful handling and feeding the NB. A real revolution in the care began in the 1960s when modern incubators, cardiac and respiratory frequency sensors, oxygen saturation monitors, equipment for positive pressure generation and mechanical ventilation (MV), pulmonary surfactant, high frequency ventilation, nitric oxide, and other technologies were developed7. Thus, children born with LBW became a concern for neonatology and for health professional services and such this evolution led to significant increased survival of this population.
NBVLBW now have greater survival due the advancement of technology and new knowledge in perinatal medicine8. All this change has been translated into higher survival rates of increasingly immature NBs and NBVLBW, leading neonatal units to introduce rules, routines and protocols aimed to obtain better results in the clinical evolution of NBs in the long-term9.
The survival of premature NBs and NBVLBW is related to the quality of antenatal care, with care during labor and delivery and with the structure of neonatal care throughout the world. Thus, it is expected that wealthier countries present lower neonatal mortality rates than countries that offer less efficient health care. On the other hand, the frequency of preterm births tends to be higher in poorer countries where pregnant women's health conditions are more precarious10.
METHODOLOGY
Descriptive and retrospective study carried out through documentary research in 64 medical records of newborns weighing <1000 g admitted to the only three public units of neonatal intensive care in Feira de Santana, Bahia, during the period from January to December 2012. It is noteworthy that, during the period of collection, there were no private neonatal intensive care units in the municipality, located in the countryside of Bahia, 108 km from Salvador, with a total land area of 1363 km2 and a population of 556,642 inhabitants11.
The study included all records of NBVLBW hospitalized during 2012 and found in the medical and statistical files of the institutions during the period studied. The data collection instrument, tested by applying a pilot test, was constructed based on the summary of discharge of high-risk newborns of the Scientific Department of Neonatology of the Brazilian Society of Pediatrics (BSP). Variables were related to: data on the mothers and on prenatal conditions, birth conditions, hospital stay and clinical outcome (discharge, death and transference).
The study was approved by the Ethics Committee of the State University of Feira de Santana under opinion nº 278,551.Data were entered and processed in Statistical Package for Social Science (SPSS) version 9.0 for Windows . Absolute and relative frequencies and the cumulative mortality rate were calculated. Analysis was based on descriptive statistics and results were presented in tables.
RESULTS AND DISCUSSION
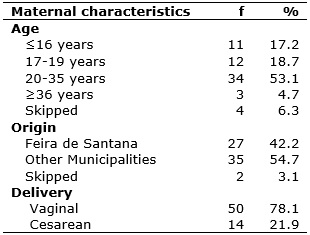
Regarding the profile of the 64 (100%) mothers of NBs surveyed, 34 (53.1%) were 20 to 35 years old. There was a significant incidence of teenagers - 23 (35.9%). Most women, 35 (54.7%) were from other municipalities. As for the type of delivery, 50 (78.1%) were vaginal delivery and 14 (21.9%) were cesarean sections, as shown in Table 1.
TABLE 1:
Distribution of the profile of mothers of newborns with extremely low birth
weight in neonatal intensive care units of Feira de Santana, 2012. (N=64)
Source: medical records of newborns in the NICU
The teenage pregnancy, issue exposed by the results of this study, is associated with premature and VLBW children. Pregnancy during this stage of development causes harm to the mother as well as neonatal complications. However, this factor is not independent and is linked to other characteristics of the mother, and prenatal and perinatal characteristics 12.
The increase in the number of pregnant adolescents is accompanied by great challenges for perinatology, due to adverse neonatal outcomes observed among NBs of mothers in this age group. Because the body is still in ongoing physical and emotional development, adolescents are more likely to have premature delivery than adult women13.
In addition to biological risk factors for the mother and the baby associated with teenage pregnancy, a worrying issue is the need for psychosocial preparation and family support to the woman, to the monitoring and to the care of the NBVLBW during hospitalization and after discharge14.
The data revealed that the majority of women were from other municipalities. This may hamper the outpatient follow-up of high-risk NBs. The main objective is to monitor the growth and development of these children, any possible sequelae, in addition to prevent and detect diseases in early moments, to apply intervention and treatment measures15 .
The follow-up must be more than an outpatient follow-up, it must assess the child in all its aspects: physical, motor, cognitive, emotional, psychological and social. It is noteworthy that this monitoring should be initiated in the prenatal care, and should be continued still in the NICU and later in clinics with a multidisciplinary team14.
Despite the reduction in mortality in the neonatal period, the incidence of chronic morbidities involving failure to grow and delayed neurodevelopment has not decreased significantly among survivors. The presence of various complications makes the appropriate follow-up after hospital discharge an extension of the care provided in the NICU. There is a need to monitor these patients in a standardized manner in order to know the profile of NBs who survive NICUs in Brazil and improve their assistance, establishing an early intervention planning15.
In this research there was a predominance of births through vaginal delivery. Study on survival of NBVLBW showed a significantly higher mortality in cases of vaginal delivery (71.1%), which may suggest natural childbirth as a contributing factor for mortality in these children16.
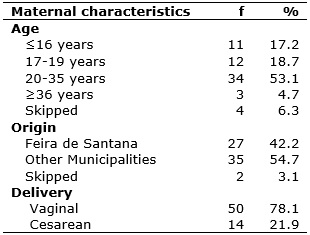
Among the 64 (100%) NBs, 43 (67.2%) had irregular breathing, gasping or apnea and required some resuscitation maneuvering. As for heart rate, 14 (21.9%) had less than 100 beats per minute. Among the main grievances during hospitalization, 33 (51.6%) NBs had record of perinatal asphyxia, 39 (60.9%) had sepsis and 58 (90.6%) had hyaline membrane disease (HMD) or SDR. According to therapeutic procedures, central vascular access was installed in 62 (96.9%) NBs, 54 (85.7%) used invasive mechanical ventilation, and 58 (90.6%) received antibiotics. See Table 2.
TABLE 2:
Distribution of birth conditions and clinical conditions of newborns with
extremely low birth weight in Neonatal Intensive Care Units in Feira de
Santana, 2012. (N=64)
Source: medical records of newborns in the NICU
Resuscitation depends on the joint assessment of respiration and heart rate (HR), which are the main indicators to determine the moment to perform the resuscitation, according to BSP17. Children born with irregular breathing, gasping, apnea and/or HR less than 100 bpm indicate the need for positive pressure ventilation. In this study, 67.2% of newborns needed resuscitation at birth because they had abnormalities in respiration and HR, which may suggest a high risk of the need to apply resuscitation in NBVLBW17.
Adequate care provided to the newborn in the delivery room is crucial to prevent the onset of asphyxia, which leads to death and, in survivors, to the presence of neurological sequelae that cause damage to the child's quality of life and the family18.
Importantly, in order to ensure adequate assistance to labor and birth, not only for premature and low weight NBs, but for all NBs, a safe environment in terms of physical infrastructure and human resources needs to be available. All institutions that assist the mother and the child during the birth process should be equipped and should have trained staff for the care of this population.
The RNEBP is susceptible to many diseases. In this research, there was a considerable number of problems that are common to this population: perinatal asphyxia, sepsis and HMD.
Perinatal asphyxia is a serious problem for neonatologists and for public health because, despite the obstetric and neonatal care, perinatal asphyxia occupies a prominent place for its potential influence in the future psychomotor performance of the NB19. Cohort study noted that the Apgar score between 0 and 6 in the 5th minute was strongly associated with early neonatal death20.
The handling of the infection is a great challenge in NBVLBW because the immaturity of the immune system associated with low clinical specificity and diversity of infections hinder a more accurate diagnosis21.
An investigation to characterize neonatal infections related to health care in a NICU of a university maternity hospital in the city of Natal, Rio Grande do Norte, showed that in a sample of 100 cases of infection, 44 (62.9%) NBs had low birth weight. Among these, 23 (32.9%) were born weighing 1,500 g 1,001g and 21 (30%) weighing less than 1.001g22 .
Study review of immunological peculiarities of extreme preterm NBs as a challenge for the prevention of nosocomial sepsis concluded that due to the immaturity of various components of immunity, extremely premature infants are highly susceptible to nosocomial infections. The very limited possibilities for intervention in this system make the control of extrinsic factors essential for prevention of nosocomial sepsis in these infants23.
Testimonials of nurses in a study on social representations of neonatal infection addressed handwashing as a simple and effective measure for the prevention of infections in NBs. In addition, the professionals scored that to prevent infections related to health care, it is necessary the use of personal protective equipment and carrying out aseptically procedures as protective measures to block the spread of pathogens in these patients24.
In this context, for the control of neonatal infections, there is the need to emphasize preventive actions by the multidisciplinary team, such as proper hand washing, care in the handling catheters, administration of medicines, in making dressings in routine cleaning, in visits, among other practices related to newborn care.
Among respiratory problems that affect premature NBs, HMD constitutes one of the most serious and frequent problems, a significant cause of morbidity and mortality25.
Longitudinal study with 360 NBs weighing between 500 and 1,500g analyzed the in-hospital mortality of these neonates, considering their clinical progression and factors associated with mortality. The results showed that the SDR was the most common disease occurring in 178 (51.4%) NBs, and 79 (44.4%) of these NBs died. SDR, pneumothorax and intracranial hemorrhage were significantly associated with death2.
Faced with the many clinical disorders to which the NBVLBW are exposed, the health team must be attentive to the need for early diagnosis and interventions in complications in order to avoid possible consequent sequelae, and thus improve the survival of children, minimizing the risk of mortality.
Generally, the NBELBW in NICU requires a number of invasive procedures for survival, such as the use of central venous catheters and invasive mechanical ventilation (MV), which were used by the majority of NBs in this investigation.
Central intravascular devices are indispensable in neonatology, since they are used for infusion of fluids, electrolytes, parenteral nutrition, blood products, exsanguination transfusion, drug administration and monitoring of critically ill patients. The use is very often prolonged due to the characteristics of patients who are unable to receive nutrition and medications through the oral via, or have limited availability of peripheral vessels and due to the very seriousness of the case in itself. Although it is a critical access, the NB is exposed to the risk of infectious and mechanical complications26.
Medical and nursing teams are responsible for proper maintenance, handling and prevention of complications associated with the use of vascular devices. It is up to these teams to establish safe measures to prevent or reduce the risks associated with the use of catheters, both central and peripheral.
The use of the MV in the neonatal period is important for the improvement of mortality rates. On the other hand, its association with lung injury can be high, especially in premature NBs21. Furthermore, in order to administrate lung surfactant therapy, which usually happens with NBELBW, the NB must be intubated, and this requires the use of MV.
Several studies have shown that the use of surfactant decreases mortality and severity of RDS, as well as reduces the incidence of barotrauma27. In Latin America, the use of surfactant was observed to reduce by around 50% the mortality in the first week of life; after this period, it reached a significant reduction of 18% in overall mortality, until hospital discharge28.
Regarding the use of antimicrobials, NBs often need these drugs in neonatal units because they are susceptible to infections and are continuously subjected to invasive procedures during hospitalization29.
All health professionals should be concerned with neonatal antimicrobial resistance, as the appearance of multi-resistant microorganisms in services is a problem of large proportions. The continuous and excessive use of these drugs promotes the induction, selection and spread of multi-resistant microorganisms responsible for serious infections, increasing the length of stay, hospital costs and especially, neonatal mortality29.
The Health Surveillance Agency (ANVISA) has made available for public consultation, since 2008, a protocol on infections related to health care (IRHC) in neonatology mapping the diagnosis of primary bloodstream infection through the use of serial measurements of protein C- reactive (PCR) of hematological and clinical criteria and partial results of the collected blood cultures30.
A study using the protocol suggested by ANVISA at the University Hospital Antonio Pedro, Fluminense Federal University, concluded that there was a reduction in the number of early diagnosis of sepsis and consequent likely reduction or antimicrobials in low-weight NBs31.
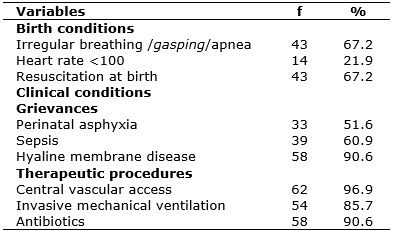
Among the total NBELBW in this study, 50 (78.2%) died (cumulative mortality rate), 9 (14.0%) were discharged and 2 (3.1%) were transferred. Three (4.7%) records did not have date on outcome, because they were incomplete, and these were considered missing data. Most deaths, 34 (68%), occurred in the first week of hospitalization, as shown in Table 3.
TABLE 3:
Distribution of outcomes according to the length of hospitalization of
newborns with extremely low birth weight in neonatal intensive care units
of Feira de Santana in the year 2012.

Source: medical records of newborns in the NICU
This research draws attention to the high rate of mortality. Deaths that occur during the neonatal period have extreme relationship with the health care of mothers and NBs, associated mainly to failures in health care during prenatal, labor and delivery32.
A multi-centered prospective cohort study on perinatal factors associated with early deaths of preterm infants born in centers of the Brazilian Network of Neonatal Research followed 579 live births with gestational age of 23-33 weeks and weight between 400 and 1,500 g without malformations in eight university tertiary public hospitals between June 2004 and May 2005. The authors compared 92 infants who died before 168 hours and 487 survivors, and among the cases of death there was higher frequency of multiple pregnancy, 23-27 weeks of gestational age, birth weight <1,000 g, need for MV and advanced resuscitation in the delivery room, Apgar <7 at 5 minutes, SNAPPE-II (clinical severity score)> 39, presence of SDR and use of surfactant20.
An analysis on the avoidable causes of neonatal mortality carried out in the year 2010 in Cuiabá, Mato Grosso, Brazil, found a coefficient of 7.9 neonatal deaths per thousand live births, and 6.0 deaths per thousand live births in the early neonatal period. Among the NBs who evolved to death (N = 74), 55 (74.3%) were preterm with <37 weeks and 52 (70.4%) had birth weight <2,500 g33.
The contribution of neonatal deaths in the infant mortality rate in Brazil has been growing in recent decades compared to post-neonatal deaths (deaths from the 28th day of life up to less than one year old). Today, neonatal deaths represent the largest portion of deaths of children under one year of age. The concentration of infant deaths in the first day and the first week of life seen in Brazil in the period from 2003 to 2005 represents 64-69% out of all infant deaths, with increased values in the Northeast, 33.6% to 63.6%34.
The high mortality rates of Brazilian studies are in contrast with the indices of wealthier countries where the quality of care, supported by massive investments in technology in NICUs, have drastically reduced the mortality of NBs, especially of NBELBW35.
A review study in Australia that analyzed the experience of a neonatal referral center regarding the survival of NBVLBW in the last 50 years showed that the survival of infants weighing 501-1,000 g has improved from 10% in 1959 to over 60% in 2009. Similarly, the survival of infants weighing 1,001-1,500 g improved about 50% for most. During the period of this study, death caused by extreme prematurity or SDR dropped from 90% in 1964 to 45% in 200836.
Specifically, the first challenge in the context of extreme premature mortality in Brazil is the inadequacy or even absence of reliable and detailed information on deaths among this gestational age group, as well as on associated factors, especially in the North and Northeast or in places far from large urban centers. Low reliability of death certificate data in the country and high underreporting of neonatal deaths (particularly in extremely premature NBs or NBELBW) in some regions of the country are well known difficulties in studies of perinatal mortality in Brazil37.
CONCLUSION
The investigation of the profile of NBELBW hospitalized in NICUs of Santana-Bahia helped to trace a diagnosis of birth conditions, clinical conditions and the outcome of this population. Certain results were cause of concern as the high incidence of asphyxia, need for resuscitation at birth and sepsis, as these can substantially lead to sequelae in these children. The high cumulative mortality revealed difficulties still present in neonatal units for assuring the survival of these NBs, even with access to high-complexity care in neonatal intensive care.
The results of this research did not allow establishing a causal relationship, since this is a descriptive study that aimed to know a local reality. The secondary data source was also a limitation, since there were losses of data, which can compromise the quality of the records.
Thus, it is necessary to review investments and redirect the neonatal care practices in the pursuit of increased survival and better conditions of survival of these NBELBW. Furthermore, prospective and analytical further studies are needed to measure factors associated with diseases and high cumulative mortality found in this investigation.
REFERENCES
1. Lemons JA, Bauer CR, Oh W, Korones SB, Papile LA, Stoll BJ et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network. Pediatrics [Internet]. 2001 [cited 2016 Jan 21]. 107(1):2-8. Available from: http://pediatrics.aappublications.org/content/107/1/e1.full
2. Carvalho ABR, Brito ASJ, Matsuo T. Health care and mortality of very low weight newborns. Rev Saúde Pública [Internet]. 2007 [cited 2015 Sep 05].41(6):1003-12. Available from: http://www.scielo.br/pdf/rsp/v41n6/5438.pdf
3. Castro ECM, Leite AJM. Hospital mortality rates of infants with birth weight less than or equal to 1,500 g in Fortaleza. J Pediatr. [Internet]. 2007 [cited 2015 Nov 15]. 83(1):27-32. Available from: http://www.scielo.br/pdf/jped/v83n1/v83n1a06.pdf
4. Ministry of Health (Br). Department of Health Care. Children's Health area. Humanized care to the newborn with low weight: Kangaroo Care. Brasília (DF) Ministry of Health; 2009.
5. Ministry of Health (Br). Ordinance No. 1,459 of June 24, 2011. [cited 2015 Nov 10]. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt1459_24_06_2011.html
6. Holanda ACOS, Silva MGC. The newborn at risk: a literature review. Rev Pediatr Ceará. 2004;5(2):11-7.
7. Zaconeta CM, Siqueira APR, Siqueira FR, Ramos EC, Margotto PR. Neonatology, the third wave. [Internet]. 2001 [cited 2015 Jun 20]. Available from: http://www.paulomargotto.com.br/documentos/neo_04022004.doc
8. Méio MDBB, Lopes CS, Morscha DS. Prognostic factors for cognitive development of very low birth weight infants. Rev Saúde Pública [Internet]. 2003 [cited 2015 Jan 21].37(3):311-8. Available from: http://www.scielo.br/pdf/rsp/v37n3/15858.pdf
9. Leone CR. Epidemiology, Challenges and Perspectives. In: Costa HT, Marba ST, organizers. The very low birth weight newborn. São Paulo (SP): Atheneu; 2004. p.10-5.
10. Joseph KS, Liston RM, Dodds L, Dahlgren L, Allen AC. Socioeconomic status and perinatal outcomes in a setting with universal access to essential health care services. CMAJ [Internet]. 2007 [cited 2015 Nov 19]. 177:583-90. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1963370/pdf/20070911s00018p583.pdf
11. Brazilian Institute of Geography and Statistics (IBGE) [website]. 2010 Demographic Census [cited 2015 Nov 10]. Available from: www.ibge.gov.br
12. Ramos HAC, Cuman RKN. Risk factors for prematurity: document search. Rev Bras Enferm. [Internet]. 2009 [cited 2015 May 25]. 13(2):297-304. Available from: www.scielo.br/pdf/ean/v13n2/v13n2a09.pdf
13. Goldenberg P, Figueiredo MCT, Silva RS. Teenage pregnancy, prenatal care and perinatal outcomes in Montes Claros, Minas Gerais, Brazil. Cad. Saúde Pública [Internet]. 2005 [cited 2015 Jun 20]. 21(4):1077-86. Available from: www.scielo.br/pdf/csp/v21n4/10.pdf .
14. Costa, AAZ. Follow-up: a review for the clinical pediatrician. Pediatr mod. [Internet]. 1999; [cited 2016 Jun 20] 35(9):743-6. Available from: www.moreirajr.com.br/revistas.asp?fase=r003&id_materia=718
15. Procianoy RS, Silveira RC. Importance of outpatient follow-up of preterm newborns. In: Silveira RC, organizer. Outpatient follow-up for premature newborns at risk. Brazilian Society of Pediatrics. Scientific department of neonatology. 2012 [cited 2015 Nov 15]. Available from: http://www.sbp.com.br/pdfs/Seguimento_prematuro_ok.pdf
16. Miotto R, Picoloto ASB, Porto PG, Silva EGS, Moraes LC, Sanfelice FS et al. Survival of extreme low weight newborns and its relationship with obstetric variables in a public hospital in Southern Brazil. In: Paper presented at the XVI South Brazilian Congress of Gynecology and Obstetrics and I South Brazilian Conference of Mastology, Florianopolis Santa Catarina, 2012; 41(1): 182.
17. Almeida MFB, Guinsburg R. Neonatal resuscitation in the delivery room: scientific document of the neonatal resuscitation program of the Brazilian Society of Pediatrics. Brazilian Society of Pediatrics [Internet]. 2013 [cited 2015 Jul 06]. Available from: http://www.sbp.com.br/pdfs/PRN-SBP-Reanima%C3%A7%C3%A3oNeonatal-atualiza%C3%A7%C3%A3o-1abr2013.pdf
18. Almeida MFB, Guinsburg R. Resuscitation of extremely preterm infants in the delivery room: controversies. J Pediatr. [Internet]. 2005 [cited 2015 Jun 20]. 81(1 Suppl):3-15. Available from: www.scielo.br/pdf/jped/v81n1s1/v81n1s1a02.pdf
19. Rosa IRM, Marba STM. Risk factors for neonatal asphyxia in newborns weighing over 1000g. J Pediatr. [Internet]. 1999 [cited 2015 Jun 20] 75(1):50-4. Available from: http://www.jped.com.br/conteudo/99-75-01-50/port.pdf
20. Almeida MFB, Guinsburg R, Martinez FE, Procianoy RS, Leone CR, Marba TM et al. Perinatal factors associated with early deaths of preterm infants born in centers of the Brazilian Neonatal Research Network. Arch Pediatr Urug [Internet]. 2008 [cited 2015 Nov 20].81(2):112-20. http://www.sup.org.uy/revistas/adp81-2/pdf/adp81-2_10.pdf
21. Moreira MEL, Lopes JMA. Mechanical ventilation in the newborn. In: MELO Moreira, Lopes JMA, Carvalho M, organizers. The newborn of high risk: theory and practice of taking care. Rio de Janeiro (RJ): Fiocruz; 2004.p.163-86.
22. Oliveira COP, Souza NL, Silva EMM, Silva JB, Saraiva EM, Rangel CL. Characterization of infections related to health care in a neonatal intensive care unit. Rev Nurse UERJ. [Internet]. 2013 [cited 2016 Mar 19]. 21(1):90-4. Available from: http://www.e-publicacoes.uerj.br/index.php/enfermagemuerj/article/view/6370/5899
23. Mussi-Pinhata MM, Rego MAC. Immunological peculiarities of extremely preterm infants: a challenge for the prevention of nosocomial sepsis. J Pediatr [Internet]. 2005 [cited 2016 Jun 20]. 81 (1 Suppl):59-68. Available from: http://www.scielo.br/pdf/jped/v81n1s1/v81n1s1a08.pdf
24. Cunha KJB, Moura MEB, Nery IS, Rocha SS. Social representations of neonatal infection produced by nurses. Rev Nurse UERJ. [Internet]. 2013 Oct/Dec [cited 2016 Jul 02]. 21(4):527-32. Available from: http://www.facenf.uerj.br/v21n4/v21n4a18.pdf
25. Diniz EMA, Vaz FAC. Hyaline membrane disease. Modern Pediatrics [Internet]. 2000 Jun [cited 2016 Jun 20]. Special edition. Available from: http://www.moreirajr.com.br/revistas.asp?fase=r003&id_materia=216
26. Margotto PR, Vieira MG, Resende JG, Brito CP, Menezes KR, Andrade LMCA et al. Vascular access in newborn. [Internet]. 2011 [cited 2016 Mar 23]. Available from: www.paulomargotto.com.br/index_sub.php?tipo=1
27. Rebello CM. Use of surfactant in the newborns. I Brazilian Consensus on Mechanical Ventilation in Pediatrics and Neonatology. AMIB [Internet]. [cited 2016 Mar 24]. Available from: www.sbp.com.br/pdfs/USO_SURFACTANTE_RECEM-NASCIDO.pdf
28. Castro ECM, Leite AJM. Hospital mortality rates of infants with birth weight less than or equal to 1,500 g in Fortaleza. J Pediatr [Internet].2007 [cited 2016 Mar 06] 83(1):27-32. Available from: www.scielo.br/pdf/jped/v83n1/v83n1a06.pdf
29. Chaves EMC, Lima NM, Dias KCF, Aragão MMS, Almeida, PC, Vasconcelos SMM. Antimicrobial use in a Neonatal Intensive Care Unit in Fortaleza. Modern Pediatrics [Internet]. 2011 abr [cited 2015 Oct 17]. 48(4):121-5. Available from: www.moreirajr.com.br/revistas.asp?fase=r003&id_materia=4976
30. National Health Surveillance Agency (Br). Public Consultation No. 13, of 2008 April 1. D.O.U de 02/04/2008. [cited 2015 Nov 03]. Available from: www.anvisa.gov.br/divulga/consulta/index.htm
31. Pinto MCFG, Bueno AC, Vieira AA. Application of protocol proposed by the National Health Surveillance Agency for the use of antibiotics in very low weight infants. J Pediatr [Internet]. 2013 [cited 2015 Nov 04]. 89(5):450-5. Available from: www.scielo.br/pdf/jped/v89n5/v89n5a06.pdf
32. Carvalho PI, Pererira PMH, Frias PG, Vidal AS, Figueiroa JN. Risk factors for neonatal mortality in hospital cohort of live births. Epidemiol Serv Saúde [Internet]. 2007 [cited 2015 Nov 04]. 16(3):185-94. Available from: http://scielo.iec.pa.gov.br/pdf/ess/v16n3/v16n3a05.pdf
33. Gaíva MAM, Fujimoi E, Sato APS. Neonatal mortality: analysis of preventable causes.
Rev enferm UERJ. [Internet]. 2015 Mar/Apr [cited 2015 Jul 02]. 23(2):247-53. Available from: http://www.facenf.uerj.br/v23n2/v23n2a17.pdf
34. França E, Lansky S. Neonatal infant mortality in Brazil: situation, trends and perspectives. RIPSA. Department of Preventive and Social Medicine / Faculty of Medicine //UFMG. Belo Horizonte. [Internet]. 2008 [cited 2015 Oct 19]. Available from: www.abep.nepo.unicamp.br/encontro2008/docsPDF/ABEP2008_1956.pdf
35. Araujo BF, Bozzetti MC, Tanaka ACA. Early neonatal mortality in Caxias do Sul municipality: a cohort study. J Pediatr [Internet]. 2000 [cited 2015 Nov 04]. 76(3):200-6. Available from: www.jped.com.br/conteudo/00-76-03-200/port.pdf
36. Battin MR, Cavaleiro DB, Kuschel CA, Howie RN. Improvement in mortality of very low birthweight infants and the changing pattern of neonatal mortality: The 50-year experience of one perinatal centre. Journal of Paediatrics and Child Health [Internet]. 2012 [cited 2015 Nov 30]. 48:596–9. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1440-1754.2012.02425.x/pdf
37. Lansky S, França E, Leal MC. Preventable perinatal deaths in Belo Horizonte, Minas Gerais, Brazil, 1999. Cad Saúde Pública [Internet].2002 [cited 2015 Nov 04]. 18(5):1389:400. Available from: www.scielo.br/pdf/csp/v18n5/11012.pdf