( *)International Classification of Diseases and Related Health Problems - CID1018.
RESEARCH ARTICLES
Assessment and characterization of pain in children: the use of quality indicators
Ligyana Korki de CandidoI; Mauren Teresa Grubisich Mendes TaclaII
I
Nurse. Nusing Resident in Chidren´s Health, State University of Londrina. Paraná, Brazil. E-mail: ligyanakorki@gmail.com
II
Nurse. Ph.D. in Nursing. Associate Professor of the Department of Nursing, Children´s Health Area, State University of Londrina. Paraná, Brazil. E-mail: maurentacla@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.10514
ABSTRACT
Pain, if untreated, can cause harm and limitations in children. Therefore, health services must make a priority of identifying and relieving such pain. This study used quality indicators for children's pain management in order to profile a pediatric unit in terms of the prevalence, intensity, treatment and relief of pain, and assessed the children's condition on hospital discharge. It was an retrospective, quantitative evaluation study, conducted by analyzing medical records of 385 children hospitalized at the Pediatric Unit of the University Hospital of Londrina, Paraná, in 2011. The prevalence of pain in these patients was 58.7% (n = 226), of whom 31.7% felt mild pain, 9.2% moderate pain, and 7.7% severe pain. However, in 51.4%, pain intensity was not quantified. The most common treatment was pharmacological (90.1%), and produced pain relief in 62.0% of cases. In conclusion, the identification, assessment and management of pain in children needs to be more efficacious.
Keywords: Pain; prevalence; quality indicators, health care; pediatric nursing.
INTRODUCTION
The pain, feeling from the beginning of life and during its development, is one of the oldest feelings described by the man, as studied by different sciences1. However, it was only in the last three decades that pain in children started to be particularly studied, which allowed a major step in the understanding of its mechanism, access and management2. The proper management of pain in children has been undervalued and little knowledge applied to our health care system and especially in nursing practice3.
Several authors have tried to explain, conceptualize and define the pain. The International Association for the Study of Pain (IASP) defines pain as "An unwanted sensory and emotional experience associated with actual tissue injury or potential, or described in terms of such damage"4:211. And he adds that the inability to verbally communicate the pain does not deny the possibility that a person is experiencing pain and require treatment and relief of it. Each individual attributes the meaning of pain according to the experiences. Pain is therefore subjective4.
Other authors defined pain as a multifactorial phenomenon, since it involves physical stimulation, anatomical changes and sensory physiology, due to various etiological factors. The theory of pain control gate suggests that it must be understood as a stimulus-response pathway, which is complex and mediated by a network of interactive processes5.
While it may be helpful, showing that something is not right, the pain is unwanted. Man avoids pain and seeks in health sciences all means to fight it6. Unfortunately, pediatric pain is a little recognized problem7, even though a common and disturbing experience in children 8.
The same progress achieved for the relief of pain in adults, in recent years, do not apply to children in the same proportions. Pain in children still need to be properly investigated, since the prevention, diagnosis and relief are still surrounded by myths and uncertainties8. It is believed that misconceptions, outdated knowledge and practices contribute to the occurrence of this fact9.
Among the myths permeating the assistance to pain in children, there are the idea of immaturity of the nervous system, which would lead to think that the pain is not felt in the same level by the child than the adult; the child does not have memory for pain; and metabolizes painkillers differently from adults, which would lead to poisoning and respiratory depression1,8,10.
Opposite to what is often thought, the child has memory for pain and can prevent future medical care, if the child have experienced painful situations not treated in hospitals. The pain not treated early in life can affect the psycho-physical and social dimensions for an extended period of time, as well as causing permanent damage to the nervous system of the child, which will affect the development and future painful experiences7,11.
"Pain damages and limitations on child affect everyday activities, changing their behavior and affecting their clinical evolution, when untreated or undertreated".12:198. In this context, pain assessment is the first step to achieving effective treatment, whether pharmacological, non-pharmacological or associated8. Consequently, the development of appropriate assessment instruments of pediatric pain is essential for the assessment not becoming subjective. Using these instruments, it should be considered the age, clinical condition and neurological impairment of the child 9,12.
In this way, pain measurement instruments are divided into three categories: self-report, observation of behavior, instruments of pain measurement 9, and may be single or multidimensional12. The difficulty in assessing pain in children is inversely proportional to age, since the older child is able to verbalize his pain, unlike the newborn and infant8. The chosen therapy should also consider the age, clinical condition, the type and intensity of pain. It is preferable to associate pharmacological and non-pharmacological measures. Therefore, it is essential to nursing knowledge to prescribe nonpharmacological measures for pain relief12.
Knowing that a lot of pain can be prevented, treated or at least reduced by using low-cost medications, physical and/or psychological techniques, there is no reason that many children in the world do not receive appropriate treatment7.
Avoid the pain of a child should be an ethical and humanitary8 obligation, and a right duty in law. The National Council for the Rights of Children and Adolescents establishes the rights of those clients in Resolution No. 41, October 1995, and in Article 7 providing the right not to feel pain when there are ways to avoid it13. Therefore, it is necessary that the relief of pain in children becomes a priority for all health professionals7.
With this sub-identification and inadequate treatment of pain in children issues, the objectives of this research were: to use the quality indicators of the management of child pain to evaluate and get the profile of a pediatric unit in the prevalence, intensity, treatment and relief of pain in children; and verify their status as hospital-related painful process.
LITERATURE REVIEW
Every day is more evident the role of nurses in the management of health services and in the quest for improved quality of care. Thus, the use of quality indicators is critical to enable the assessment of care over time and allow the comparison with internal and external references12,14,15.
An initiative aimed at improving children´s health care is the self-monitoring in health services, enabling the evaluation of the health team efforts to improve quality, and change responses to needs arising from this evaluation9. In order to improve the quality of childcare, as well as access and treatment for their pain, it is essential to be realized the management of child pain through quality indicators12.
Other advantages resulting from efforts to improve the quality of pain management are to reduce hospital costs, the short the patient's stay in hospitals and reduced medical error risk16. The same author also demonstrates the importance of identifying strategies measure and indicators of pain management quality and recommends the standardization of outcome measures to be used in the evaluation of quality care17.
It is necessary to understand that decisions based on evidence provide a strong justification for the development of policies that encourage changes in clinical practice and therefore better care9.
Therefore, the use of quality indicators provides not only the improvement of the care process, but also records of nursing practice. It provides information that can support decision making, as well as the development of institutional and public health policies, aimed at improving the quality of care in the management of childhood pain.
METHODOLOGY
Evaluative study, retrospective, quantitative approach, performed in child population records of the pediatric unit of the University Hospital of Londrina (HUL), supplementary service of the State University of Londrina (UEL), of higher education, public nature, located in Londrina, Paraná, Brazil.
The sample consisted of 385 medical records of children aged 0-13 years old hospitalized from January to December 2011. The sample size (n=385) was determined by statistical calculation, considering the deviation values of parameters confidence level standard (z), desired level of accuracy (p), and population standard deviation (s).
Data relating to the characterization of the sample profile (age, gender, caregiver), the profile of hospitalizations (total days, clinic, diagnostic/International Statistical Classification of Diseases and Related Health Problems (ICD10)18 and the characterization, assessment and pain treatment (in the first two days of the experience of pain) were collected by the researcher in printed records provided by the Statistical and Medical Archive Service (SMAS) of HUL. In printed records, first the nursing prescription was analyzed (vital signs and annotation). In cases where they met contradictory or incomplete information, they also used the medical prescription. During the analysis, not quantified pain was considered in cases where the pain was not recorded numerically as a vital sign, but it was described in nursing annotation.
Inclusion criteria were children who were in the age group foreseen and hospitalized to the pediatric unit from January to December 2011. The exclusion criteria were children with medical records missing or incomplete, in which the nursing forms and prescription were not located. There were no losses in the sample during the study. The sample was considered random because of not intentionality of choice of records in SAME, observing only the defined criteria.
The inpatient unit has 34 pediatric beds and adopts rooming-in system. During 2011, 685 children were treated in the unit, for a total of 1702 hospitalizations. In cases where the child has been hospitalized more than once, it was decided to consider the admission of longer days and to submit full medical records.
Infant scales for pain assessment used for routine pediatric unit are: Pain Behavior Scale for Newborns and Children under 2 years old and 364 days - Neonatal Infant Pain Scale (NIPS)19 - and Faces Scale20 for children aged three years old or more.
The NIPS scale consists of five behavioral and physiological indicators, in which the score ranges from 0 to 7, considering pain to values greater than or equal to 419.
The Faces Scale uses the figure of a character known by Brazilian children (Cebolinha by the cartoonist Maurício de Souza), which makes it more attractive and facilitates the identification of the child with the scale. The instrument consists of five images with the expression without pain to unbearable pain and accompany an alphanumeric scale, where 0 = no pain, 2 = moderate pain, 3 = severe pain, and 4 = unbearable pain20.
Data analysis was performed using the Microsoft Excel® program and using the formulas of quality indicators for assessing the prevalence of pain in children; occurrence rate of mild, moderate and severe pain; pharmacological treatment rate, non-pharmacological rate and associated in children with pain; and rate of children with pain at discharge12.
The study was conducted in accordance with the requirements of Resolution 196/96 of the National Health Council, with approval of the project by the Ethics Committee for Research Involving Human Beings of the State University of Londrina (CEP/UEL), Opinion 310/2011, CAAE 0292.0.268.00011. The researcher signed the term of confidentiality and secrecy of data, ensuring ethical behavior in the research.
RESULTS AND DISCUSSION
Subjects' profile
The data collected from medical records (n=385) showed that 246 (64%) children hospitalized in the period were male and 139 (36%) were female. Regarding to age, 158 (41%) children were from 0 to -2 years old; 127 (33%) from 3 to 7 years old; and 100 (26%) between 8-13 years old.
The average length of stay in the Pediatric Unit was 4.5 days, the mother being the most frequent company in 335 (87%) hospitalizations; then the father in 27 (7%) and other caregivers (grandparents, uncles and brothers) in 19 (5%); 4 (1%) children were institutionalized and were unaccompanied. It should be remembered that this hospital adopts the rooming-in system for many years and recognized the importance of the presence of parents in the child´s recovery, as it influences the way in which the child plays, express and respond to the experience of pain21.
As the clinic responsible for the hospitalization, 206 (53.5%) children were treated by the Pediatric Emergency Room; 73 (18.9%) by the Children´s Surgery and Emergency Surgical; 47 (12.3%) for Orthopedics and Orthopedic Emergency Room, and 59 (15.3%) remaining for other clinics.
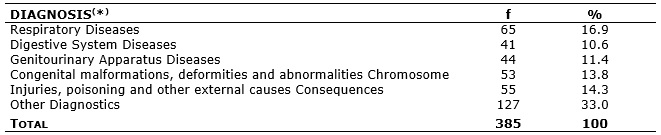
It was also found that the most common diagnoses were diseases of the respiratory tract in 65 (16.9%) patients; Injuries, Poisoning and other external Causes of Consequences in 55 (14.3%) patients; and Congenital Malformations, Deformities and Abnormalities Chromosome in 53 of them (13.8%), according to Table 1.
Table 1:
Distribution of patients by hospitalization diagnosis, in the pediatric unit of the University Hospital of Londrina. Londrina, Paraná 2015.
(
*)International Classification of Diseases and Related Health Problems - CID1018.
Chidren´s pain issue
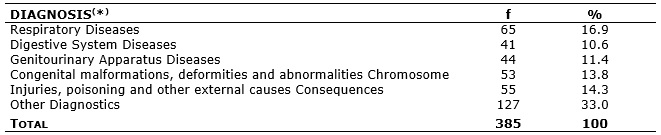
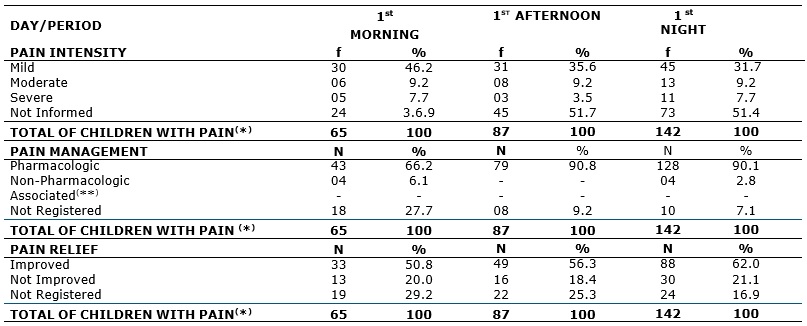
The prevalence of pain during the sample period of hospitalization investigated was 226 (58.7%). Evaluating the first two days when the child experienced the pain phenomenon during the three periods of the day, it was found that there was a higher prevalence of pain during the night, 142 (62.8%) and 70 (31%) respectively in the first and second days, as shown in Tables 2 and 3. Similar results were found in a study also conducted in Brazilian university hospital, which examined the prevalence of pain in children considering the child´s own reports, their family and health professionals. The prevalence of pain found in this study was 59%, according to reports of the child; 49% as family members; 50% according to nurses; and 38%, according to medical staff 22.
As for intensity, management and pain relief in these periods of time of increased prevalence, it was observed that most children have experienced mild pain, followed by moderate and severe pain, according to Tables 2 and 3. Compared with other research, already quoted above, which described the pain as mild and intense, given the reporting of children and their families, it was observed a higher prevalence of severe pain. The children reported intense pain in 22% of cases and mild in 17%; their families already mentioned the pain of the child as severe in 24% of cases and mild in only 3%22.
Table 2:
Quality indicators related to children´s pain by period, in the first day of pain experience of the hospitalized child in the Pediatric Unit of the
University Hospital in Londrina, Londrina, Paraná, 2015.
 (
*)The same child may have experienced pain over a period in the day.
(
*)The same child may have experienced pain over a period in the day.
(
**)Association between pharmacological and non-pharmacological methods.
Table 3:
Quality indicators related to children´s pain by period, in the second day of pain experience of the hospitalized child in the Pediatric Unit of the
University Hospital in Londrina, Londrina, Paraná, 2015.
(
*)The same child may have experienced pain over a period in the day.
(
**)Association between pharmacological and non-pharmacological methods.
The lower prevalence of moderate and severe pain in this study may be explained by the treatment and relief of pain as mild pain, or considering the fact that many children felt pain but did not have the intensity of their pain quantified by the nursing team. Other studies also demonstrate the lack of proper record considering the assessment and management of pain in pediatric records3,22,23. From these findings, it is concluded that the pain is still under-reported, which may result in inappropriate treatment.
It is very important to quantify the pain, to better understand it24. Thus, it is possible to guide the best analgesic method, assess whether there was an improvement or worsening of pain and also if the methods used were effective. However, the pain should be treated regardless of its intensity, that is, whenever there is pain, it is a child´s legal right13. When mild pain not prevented or treated, the painful process can be amplified, hindering its control25. The child should never be encouraged to tolerate the pain or expect it to decrease it alone3, their reports and expressions need to be always considered.
As for the management of pain in this study, it was conducted by pharmacological behavior in 128 (90.1%) cases on the first night; and in a nonpharmacological way in 4 (2.8%) cases; and 10 (7.1%) of non-registered conduits. In the second night, pain management drug was used in 63 (90.0%) cases; nonpharmacological methods in 2 cases (2.9%) and associated in 1 (1.4%); during this period, 4 (5.7%) methods were not recorded, according to Tables 2 and 3. In another study conducted in 2004 in the same university hospital and two private hospitals in the city of Londrina, referring to the post-pain operative in the children, it was also found that most of the methods used for pain relief drug was being reduced prescribing non-pharmacological methods. Most nursing prescriptions were not accurate to pain control as well as the signal recording and complaints of pain in the charts3.
Considering that the definition of pain is multidimensional, so it treatment should be multidimensional, associating pharmacological and non-pharmacological therapies whenever possible12,23. The most widely used pharmacological measures are the nonsteroidal anti-inflammatory drugs, opioids and adjuvant analgesics23. Among the non-pharmacological measures, there are distraction, relaxation and comfort methods; hot water bag; non-nutritive sucking; affection; lullaby; recreational activities and explanatory talk about the pain23,26,27. The association of pharmacological and non-pharmacological measures, as well as potentially effective, is not costly for the institution, since the non-pharmacological measures are easily available, inexpensive and do not cause inconveniences in most clinical situations28.
Regarding to pain relief after their management, there was an improvement of registration in 88 (62.0%) cases; there was no improvement in 30 (21.1%); and there was no record in 24 (16.9%) on the first night. As the second night, where there was an improvement in 40 (57.2%), there was no improvement in 15 (21.4%) and 15 were not recorded (21.4%) about the methods performed for the relief of pain in children, according to Tables 2 and 3.
A study conducted in 2007 with parents accompanying children hospitalized in the same university hospital of this study, there was improvement of pain in most cases after the pharmacological and non-pharmacological method. However, non-pharmacological treatment was not prescribed by nurses but done by parents who applied knowledge/common sense measures27. It is essential that nurses have knowledge and prescribe non-pharmacological care for pain relief12. Often these measures are performed in routine pediatric units, but are not properly prescribed and recorded in medical records.
Finally, during the time of hospital discharge, while 192 (50%) children did not present pain, it was observed that 14 (3.5%) still felt pain and 179 (46.5%) did not have their information about pain or general condition recorded in medical records.
It is estimated that children experienced the suffering of pain on average 2.7 days during their hospitalization. However, the number ranged from 1 to 17 days and is also related to the case history of the child and total days of hospitalization. It is known that situational factors may affect children more than adults. Thus, greater attention in evaluating the painful process in children hospitalized is required22,24.
According to the author about the quality indicators used in this study12, after 3 years of managing the indicators on pain in children, it was possible to identify the profile of the children with pain, the characteristics of their pain and the treatments used to relieve it, in addition to understanding the nursing contribution in the use of non-pharmacological therapies. The author also states that the discussion of the results found with the nursing staff favors the engagement of staff in an attempt to improve care for children with pain, and also record it properly12, since the failure to register may result in consequences, not only assistance but also administrative and financial29.
CONCLUSION
The prevalence of pain in children was 226 (58.7%). Evaluating the first two days when the child experienced the pain phenomenon in relation to the three periods of the day, it was found that there was a higher prevalence of pain during the night, in the first and second days.
In the intensity of the pain phenomenon more prevalent period, it ranged from mild, moderate and severe; however, most had not quantified the intensity of their pain. For the management of pain, pharmacological procedure was performed in most of cases, resulting in pain relief. During the time of hospital discharge, it is noteworthy that half of the sample did not show pain, although small part still felt; and significant part did not contain such information on files.
It is concluded that the pain identification in children needs to be more effective, as well as its evaluation and management. It is noteworthy that the study was limited by the lack of appropriate notes in medical records, which shows the importance of the nurse´s commitment to the legal registration of care practice. In this way, appropriate training for health professionals on the evaluation, the management and registration of pain are necessary, in addition to new studies to better understand the painful process in children.
REFERENCES
1.Pulter ME, Madureira VSF. Dor no recém-nascido: percepções da equipe de enfermagem. Revista Ciência, Cuidado e Saúde. 2003; 2:139-46.
2.Walco GA, Goldschneider KR, organizadores. Pain in children: a practical guide for primary care. Springer, ed. Ilustrada; 2008.
3.Tacla MTGM, Hayashida M, Lima RAG. Registros sobre dor pós-operatória em crianças: uma análise retrospectiva de hospitais de Londrina, PR, Brasil. Rev Bras Enferm. 2008; 61: 289-95.
4.Merskey H, Bogduk DN. Part III: pain terms, a current list with definitions and notes on usage. In: Classification of Chronic Pain . Seattle (USA): IASP Press; 2012. p. 209-14. [citado em 22 ago 2014]. Disponível em: http://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698&navItemNumber=576 .
5.Melzack R, Wall PD. Textbook of pain. Edinburg (UK): Churchill Livingstone; 1999.
6.Horta WA. Dor: seu significado psicológico para estudantes e docentes de enfermagem e psicologia. Rev Enferm: Novas Dimensões; 1976; 2: 1-4.
7.International Association for Study of Pain. Children's pain matters! Priority on pain in infants, children, and adolescents. Special interest group on pain in childhood; 2005. [cited in 2014 Oct 25]. Available from: http://childpain.org/sig-child-position-stmt.pdf.
8.Pimentel MH. Mitos e ideias incorretas acerca da dor na criança. Nursing (Lisboa). 2001; 13:27-31.
9.Finley GA. Supporting evidence for childkind principles. 2010; [cited in 2014 Mai 10] 1-17. Available from: http://aneswebout.tch.harvard.edu/sites/childkindinternational/files/2013/05/EvidenceChildKindPrinciplesPort.pdf .
10.Ashwill JW. The child in pain. In: Ashwill, JW, Drosk, SC. Nursing care of children: principles and pratice. Philadelphia (USA): WB Saunders Company;1997. p. 514-31.
11.Schechter N, Berde C, Yaster Y, organizadores. Pain in infants, children and adolescents. Lippincott Williams & Wilkins. Seattle; 2003. p. 3-16.
12.Leão ER, Silva CPR, Alvarenga DC, Mendonça SHF e organizadores. Qualidade em saúde e indicadores como ferramenta de gestão. São Caetano do Sul: Yendis Editora; 2008. p.197-208.
13.Ministério da Justiça (Br). Conselho Nacional dos Direitos da Criança e do Adolescente Hospitalizados: Resolução no 41/95. Brasília (DF): CNDCA; 1995.
14.Caldana G, Gabriel CS, Bernardes A, Évora YDM. Indicadores de desempenho em serviço de enfermagem hospitalar: revisão integrativa. Rev Rene. 2011; 12:189-97.
15.Vituri DW, Matsuda LM. Validação de conteúdo de indicadores de qualidade para avaliação do cuidado de enfermagem. Rev esc enferm USP. 2009; 43:429-37.
16.Gordon DB, Dahl JL, Miaskowski C, McCarberq B, Todd KH, Paice JÁ, et al. American Pain Society recommendations for improving the quality of acute and cancer pain management. American Pain Society quality of care task force. Arch Intern Med. 2005; 165:1574-80. [cited in 2011 Oct 10]. Disponível em: http://archinte.ama-assn.org/cgi/reprint/165/14/1574.pdf..
17.Gordon DB, Pellino TA, Miaskowski C, McNeill JÁ, Paice JÁ, Laferriere D, et al. A 10-year rewiew of quality improvement monitoring in pain management: Recommendations for standardized outcome measures. Pain Management Nursing. 2002; 3:116-30.
18.Ministério da Saúde (Br). DATASUS tecnologia da informação à serviço do SUS [site de Internet]. Morbidade Hospitalar do SUS: CID-10 Capítulos. [citado em 10 out 2011]. Disponível em: http://tabnet.datasus.gov.br/cgi/sih/mxcid10.htm.
19.Lawrence J, Alcock D, McGrath P, Kay J, MacMurray SB, Dulberg C. The development of a tool to assess neonatal pain. Neonatal Netw. 1993; 12:59-66.
20.Claro MT. Escala de faces para avaliação da dor em crianças: etapa preliminar [dissertação de mestrado]. Ribeirão Preto (SP): Universidade de São Paulo; 1993.
21.Pimenta CAM. Dor crônica, terapia cognitiva comportamental e o enfermeiro. Rev Psiq Clin. 2001; 28:288-94.
22.Linhares MBM, Doca FN, Martinez FE, Carlotti AP, Cassiano RG, Pfeifer LI, et al. Pediatric pain: prevalence, assessment, and management in a teaching hospital. Braz J Med Biol Res. 2012; 45: 1287-94. [cited in 2014 Sep 10]. Available in: http://www.scielo.br/pdf/bjmbr/v45n12/2302.pdf.
23.Macgrath PA. Children - not simply little adults. In: Merskey H, Loeser JD, Dubner R (organizadores). The paths of pain. Seattle (USA): Iasp Press, 2005. p.433-46.
24.Melo LR, Pettengill MAM. Dor na infância: atualização quanto à avaliação e tratamento. Rev Soc Bras Enferm Ped. 2010; 10: 97-102.
25.Andrade MP. Dor pós-operatória: conceitos básicos de fisiopatologia e tratamento. Rev Soc Bras Estudos Dor. 2000; 2:7-14.
26.Lemos S, Miguel EA. Caracterização do manejo da dor realizado pela equipe de enfermagem na unidade de terapia intensiva pediátrica. Cienc Cuid Saude. 2008; 7: 82-7.
27.Silva LDG, Tacla MTGM, Rossetto EG. Manejo da dor pós-operatória na visão dos pais da criança hospitalizada. Esc Anna Nery. 2010; 14:519-26.
28.Curtis S, Wingert A, Ali S. The Cochrane Library and procedural pain in children: an overview of reviews. Evid.-Based Child Health. 2012; 7:1363-99.
29.Claudino HG, Gouveia EML, Santos SR, Lopes MEL. Auditoria em registros de enfermagem: revisão integrativa da literatura. Rev enferm UERJ. 2013; 21:397-402.