FIGURE 1: List of publications in the sample of the study. Santa Maria/RS, 2011.
RESEARCH ARTICLES
Health care in men: reality and perspectives
Rogério PozzattiI; Margrid BeuterII; Lucimara Sonaglio RochaIII; Naiana Oliveira dos SantosIV; Maria de Loudes Denardin BudóV; Nara Marilene Oliveira Girardon-PerliniVI
I
Nurse at Santa Maria University Hospital. Member of Care Research Group, Health and Nursing, Federal University of Santa Maria. Santa Maria, Rio Grande do
Sul, Brazil. E-mail: roger.pozza@yahoo.com.br
II
PhD in Nursing. Associate Professor, Nursing Department and from the Graduate Program in Nursing of Federal University of Santa Maria. Member of Care
Research Group, Health and Nursing. Santa Maria, Rio Grande do Sul, Brazil. E-mail: margridbeuter@gmail.com
III
MS in Nursing. Nurse from the Charity Hospital Dr. César Santos de Passo Fundo, Rio Grande do Sul, Brazil. Member of Care Research Group, Health and
Nursing. E-mail: lucimarazz@hotmail.com
IV
Nurse. MS in Nursing. PhD in Nursing on Federal University of Rio Grande do Sul. CAPES scholarship. Porto Alegre, Rio Grande do Sul, Brasil. Member of Care
Research Group, Health and Nursing. E-mail: naiaoliveira07@gmail.com
V
PhD in Nursing. Nursing Department and from the Graduate Program in Nursing of Federal University of Santa Maria. Member of Care Research Group, Health and
Nursing. Santa Maria, Rio Grande do Sul, Brazil. E-mail: lourdesdenardin@gmail.com
VI
PhD in Nursing. Adjunct Professor from the Department of Nursing and the Graduate Program in Nursing at Federal University of Santa Maria. Member of Care
Research Group, Health and Nursing. Santa Maria, Rio Grande do Sul, Brazil. E-mail: nara.girardon@gmail.com
ABSTRACT
This research aimed to know the scientific production about the health care in men. A review of literature was based in database of Latin-American and Caribbean Center on Health Sciences Information and Scientific Electronic Library Online from 1994 to 2011, using the word health of men. Fifteen papers were selected and analyzed by method of content analysis, emerging these categories: the question of gender and its relationship with care or careless with health in men, the portrait of attendance of health of men; and the strategies needed in this process. It is concluded that the hegemonic ideas and the normative of masculinity potentiate the risk, not only to health of men but also to other people, thus requiring new strategies, that includes issues of gender, to meet the needs of this population.
Keywords: Nursing; nursing care; men's health; masculinity.
INTRODUCTION
Historically men take little care for their health and only seek help when problems worsen, in other words, when the disease is already interfering on their quality of life1. Searches that make comparisons between men and women prove that men are more vulnerable to diseases because of the neglect with their health, and they die earlier2.
Regarding about the male mortality in Brazil, the coefficients show a rate 50% higher on men´s group, when compared to women. Considering the male mortality, for age, the largest number occurs in the age group from 20 to 39 years old, which contains three male deaths for each female death. Concerning about the distribution, according to the causes, stand out the deaths from circulatory diseases followed by those relating to accidents and violence 4.
The major causes of men´s low accession measures to comprehensive health care are the sociocultural barriers, which are structured as an obstacle among men and health services. Those barriers foment the belief and the values of what is being a male and the gender stereotypes that are rooted for centuries in our patriarchal culture. In this context, the illness for most part of the male population is considered a sign of fragility and for which it is judged invulnerable, consequently, unless care is taken favoring the exposure to situations oh health risk5.
The promotion of human health is a theme which has being currently discussed and evaluated by researchers, scientific society, as well as managers from the Public Health System (SUS), even so incipient. The proposal of the Nacional Politics of comprehensive care to Men's Health was approved on August 27 th, 2009. This policy recognizes that the health problems to the male constitute relevant problems of the public health. Therefore, it is necessary to promote actions that contribute significantly for understanding the masculine singular reality in their various sociocultural contexts, political and economic. The implementation of this policy is expected to help reduce the rates of mortality by preventable and avoidable causes of men, increasing, thus, the male life expectancy6.
In view of the problems exposed, the aim of this study was to know the scientific production about the health care of men.
METHODOLOGY
It is a study of literature review. For its preparation the reading of the bibliographic material was held and its selection was as the purpose of the study7. Thus, the work was consolidated from the scientific production related to the theme about the health care of men. The bibliographic survey was performed consulting the Virtual Health Library accessing the Latin American Literature and Caribbean Health Sciences database and the Scientific Eletronic Library Online portal (SCIELO). The literature review is also known as a narrative review, by presenting a descriptive and discursive character. This kind of revision is produced by professionals with recognized competence and experience, constituting an important element in the scientific literature8.
The search for the material was performed on July 17th , 2011, using the word man´s health. The time frame for the material publication was delimited from 1994 to July 2011. From 1994 the Family Health Programs were noted(PSF), today Family Health Strategies (ESF), began to be implanted, focusing on the promotion of population´s health issue, being an important history goal for this investigation focusing on the scientific issue.
The inclusion criteria for the study were: articles in portuguese, english and spanish, original and review published from 1994 to July 2011 with texts available in full addressing the issue about health care of men. Books, book chapters, manuals, event abstracts, experience reports, opinions, repeated work and publications not available in full were excluded.
In the first stage of the research 77 productions were detected, being 57 works in the LILACS database and 20 SCIELO portal. Then, studies that reached the goal and met the criteria for inclusion and exclusion were selected. Being the full text unavailable in the LILACS database and 20 SCIELO portal, the search was conducted on the website of the journal where the article was published (magazine´s homepage) and at the Coordination of Improvement of Higher Education Personnel portal (CAPES) on the journal section. Fifteen full articles, eight in the LILACS database and seven in SCIELO portal were part of the corpus research. The articles were numbered using the coding A1, A2, A3 and even A15. For the organization of the scientific production a token mapping was used constituted of variables: work title; author; periodical; year of publication and type of study.
After this first step, the selected articles were analyzed and interpreted using content analysis9. This analysis may be described as "[...] a set of communication analysis techniques that uses systematic and objective procedures of description of message content"9:40. In this sense, the three phases proposed by the method were proceed.
The pre-analysis consisted of reading and rereading of 15 selected articles, observing the addressed issues. The step in the exploration of the material, the reading of the articles was thorough, occurring delineation of categories focusing on the goal of the study. From the analysis of articles, the data handling, the inference and the interpretation were followed.
RESULTS AND DISCUSSION
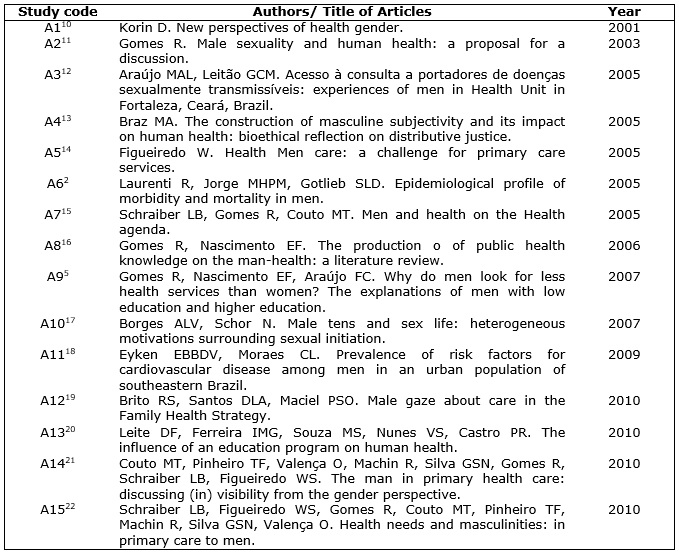
The articles2,5,10-22 which composed the corpus for analysis are presented on figure 1.
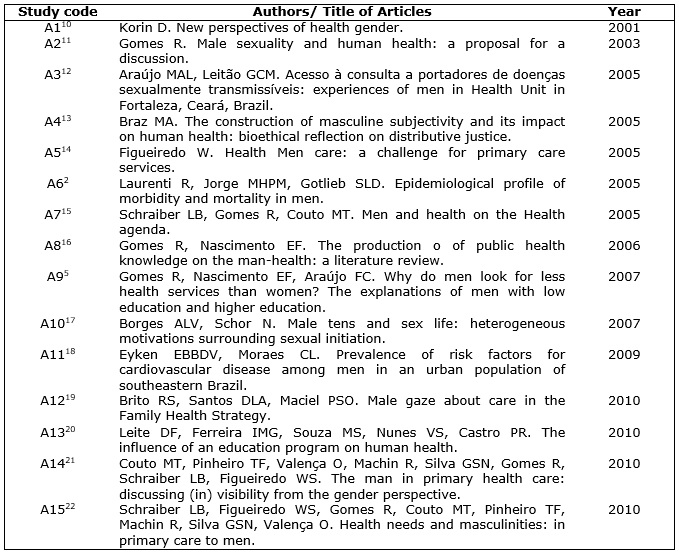
FIGURE 1: List of publications in the sample of the study. Santa Maria/RS, 2011.
The three emerging categories of the studies are analyzed as follows: the issue of gender and its relationship with care (less) of the Men's Health; the portrait of services in men´s health care treatment; and, the strategies needed for the men's health care.
The gender issue and its relationship with care (less) of the Men's Health
The differences between men and women are discussed from different aspects in many knowledge areas. In health area, they are addressed more specifically into issues of sex and gender. Amiss, the terms sex and gender are usually used as synonyms2,10. The term sex reserves to biological predetermined
Characteristics, relatively invariant, from the man and the woman, while the term gender is used to signal the socially constructed characteristics that constitute the definition of male and female, in different cultures2. Gender issues vary spatially (from one culture to another), temporally (n the same culture in different historical times), and longitudinally (throughout the whole life of an individual)10. Being a man means incompatible features with the demonstration of weakness signs, of fear and insecurity. Those who do not reach this goal, or those who do not consider it crucial to their lives, they end up being branded as weak or, even, effeminate5. A more appropriate way to understand men's health is by adopting a gender approach. That means examine health issues in men and women context. 21,23. In this sense, becomes crucial to think of actions that aimed at promoting health, because the social masculinity construction influences the habits and male behaviors, putting men in vulnerable situation, especially on health issues.
The gender issues influence on male life´s behavior and habits, producing not only livelihoods, but also ways of getting sick and dying6,13,16. The results of the study show that men with strong masculinity beliefs have half the probability to receive preventive care than those with moderate masculinity beliefs. Stereotypical notions of masculinity reduce the possibilities of preventive health care, making men die earlier than women 24. Therefore, there is a need to transform certain concepts and roles assigned to men and women related by gender.
The care is still seen and understood as essentially feminine task, because women are early educated to perform and take responsibility for this role 25. Caring is associated with femininity, making that many men do not take care of their health. In counterpoint, the male identity is more associated with the devaluation of the self-care and to health risks exposure14.
In accomplished study, found that women look more regularly for health services than men. Gender differences between men and women are also related to the reasons for the demand of health care services12. The woman is not afraid to look for medical attention, not ashamed either to admit that she cares for her, health because there is no prejudice against this care.
Overall, men live less than women2, besides, they occupy more than half of all hospital beds26. The mortality data from many countries of Latin America indicate that men have a lower life expectancy at birth, in all studied nations2.
Among the main causes of male death are: cardiovascular diseases (ischemic heart disease and cerebrovascular diseases), the malignant neoplasms (stomach cancer, lung cancer and prostate cancer) and violence, highlight on transport accidents.
Many causes of male death are due to risky behaviors, which could be prevented or avoided through changes in behavior and in his lifestyle2,20.
In a study about the prevalence of risk factors for cardiovascular disease on men aged 20 to 49 years old, modifiable factors or factors that can be controlled consider, the smoking, the arterial hypertension, combating physical inactivity, the control of mellitus diabetes, the obesity and hyperlipidemia18. The authors found that most part of the studied population had at least one risk factor for cardiovascular diseases.
Between the common male risk behaviors is the alcohol abuse, the performance of dangerous tasks, the disregard on safety standards in relation to personal protective equipment in their work activities and, also, resistance to condom use in sexual relationships15. Some studies show that it´s scarce the attention to the actions of reproductive and sexual health, mainly with teen men17. Also emphasize that is in this age that most of the male population has her sexual initiation in which, if unprepared, they are exposed to a greater risk of contracting sexually transmitted diseases (STDs) as the Acquired Immunodeficiency Syndrome (AIDS).
The male population is affected by situational factors that put them away from the health services and expose them to more risks10. While women use more health services, which can be explained by differences in health needs between gender. This is due to the demands associated with pregnancy and childbirth, and a greater interest in health for women27.
The portrait of health care services in men
The public health services, especially the primary care, were shaped and constructed originally by programs and policies aimed at women's, children´s and elderly´s health. Therefore, in essence, they were not designed to attend the specifics of the male population. Added to the worrying situation of male mortality, study data suggest raise emerging concerns of new service strategies that will meet the needs of men's health within their particularities 13.
Some men consider the basic health units (BHU) a feminized space14. This is because, most clients and professional staff is mostly female, with few actions geared specifically to men's health. This reality can remove men from health units because of the feeling of not belonging to this space.
Among the various reasons that make some men look for health services, as a preventive, is the fact of the exposition to another man or a woman5 . This feeling, characterized by shame, would be associated with machismo and lack of habit of being exposed to professionals. The fear of discovering that something goes wrong with your health and the lack of health care specific to men are barriers that hinder the access of users. An accomplished study with men, regarding their perceptions about prostate cancer, showed that cultural, economic barriers and lack of access to treatment, reflect the low demand for early detection of prostate cancer28.
The near absence of males in the BHU may be associated with the difficulty that man has to verbalize their health problems and the fear of appearing weak in front of others14. The health services need to be transformed to include specific needs of the male population14,29.
There is a large number of young men with AIDS and the lack of an effective approach by health units about sexual and reproductive issues that are surrounding men´s health17. It is necessary a mobilization for the care of men's health, from youth, based on the population´s health needs principles, like sexuality and reproduction.
The demand of the male population for emergency on health services, such as pharmacies and emergency, in detriment of BHUs, can be justified by the fact that, in these spaces, men feel more comfortable to expose their health problems and have their needs promptly met. The pharmacy is seen by men as a semiprofessional instance where they can ask for advice from medical services without wasting time, objectively, on this account, in general, their urgency is to relieve pain or alleviate symptoms5,14. In these places men would be attended faster with no lines and no schedule medical appointments and they would expose their problems more easily14. One of the consequences of the demand for a fast and emergency and, sometimes, inappropriate is the worsening of many chronic diseases that if treated early could be avoided. The mean duration of hospitalization days is higher in males, pointing as a possible hypothesis the fact that, maybe, men would be hospitalized to specialized medical services at more advanced stages of the disease than women. thus prolonging treatment2.
The strategies required to treatment of men's health
Receiving and giving resoluteness specific male population health needs is a challenge for health services. Include male participation in health activities is a need that must be addressed on gender focus, which at first sight might be taken as a countermove against woman11. However, from the gender dimension is possible to better understand the specifics both male and female, thus enabling, the achievement of health gains for both man and woman.
Accordingly, is necessary to enable providers of health services at all levels to fit more progressive man care models. This is because the position of the health institutions professionals may represent a barrier to their health10,22.
The Family Health Strategy may consider some specific men's health issues, developing promotion and health prevention2,19. Thus, strengthen educational activities especially in relation to violence, prostate and lung cancer, and to stimulate the reduction of smoking and alcoholism, promoting the habit of looking for health services as a preventive measure2.
The proposed of SUS health services reorganization lies in the structuring phase, despite all the advances made. Advances that are the result of major political ideological struggles, seeking to ensure health access for all people, without any prejudice12.
New perspectives are being created regarding the participation of the male population in events involving the health of their families. An example is the inclusion of man with his wife on attention in pregnancy and childbirth15.
Concerning the National Policy on Integrated Human Healthcare, Papai Institute, that develop educational activities for poor men and gender studies in Recife, produced guidelines document to a policy of comprehensive care to men in health. In this publication, the institute suggests that health policy for men does not compete with the women's health policy resources, but act jointly. The goal is to consider psychosocial and cultural aspects, investing in the improvement of human health information systems, respecting diversity within the genre itself30.
CONCLUSION
The factors that lead to high male mortality are due from habits and unhealthy lifestyle. Such factors are due to male stereotype, being perceived by society as strong and invulnerable being.
The analysis of scientific production demonstrated that men recur less than women to health services. This happens due to the feeling of not belonging to the group of beneficiaries, posing as barriers the non compliance performance schedules and the lack of skilled professionals to work on the population´s health issues.
Men are supporters of emergency health care services, which are most sought when some symptom that hamper their daily activities or professional arises. The late diagnosis and treatment contribute to the chronicity of the disease, increase the number and length of hospital stay, raising the death rate of men compared to women.
The strategies required for the men health care include the training of professional health services with gender focus, the knowledge of the specifics of this population, and the development of educational actions on main issues that affect men's health.
REFERENCES
1.Costa-Junior FM, Maia ACB. Concepções de homens hospitalizados sobre a relação entre gênero e saúde. Psicologia: Teoria e Pesquisa. 2009; 25:55-63.
2.Laurenti R, Jorge MHPM, Gotlieb SLD. Perfil epidemiológico da morbi-mortalidade masculina. Ciênc saúde coletiva. 2005; 10:35-46.
3.Waldman, EA. A transição epidemiológica: tendências e diferenciais dos padrões de morbimortalidade em diferentes regiões do mundo. O Mundo da Saúde. 2000; 24:10-8.
4.Sociedade Brasileira de Urologia. SBU promove campanha de Saúde do Homem até final de setembro. 2008. [citado em 20 mar 2013]. 8:336. Disponível em: http://www.sbu.org.br/indexGeral.php?do=imprensa&sub=6&pagina=2&dado_id=5 .
5.Gomes R, Nascimento EF, Araújo FC. Por que os homens buscam menos os serviços de saúde que as mulheres? As explicações de homens com baixa escolaridade e homens com ensino superior. Cad Saúde Pública. 2007; 23:565-74.
6.Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Política Nacional de Atenção Integral à Saúde do Homem. Brasília (DF); 2008. [citado em 20 abr 2013]. 9:335. Disponível em: http://dtr2001.saude.gov.br/sas/portarias/port2008/pt-09-cons.pdf.
7.Gil AC. Como elaborar um projeto de pesquisa. 4ª. ed. São Paulo: Atlas; 2002.
8.Munoz SIS, Takayanagui AMM, Santo CB, Sanchez-Sweatman O. Revisão sistemática da literatura e metanálise: noções básicas sobre seu desenho, interpretação e aplicação na área de saúde. In: Anais do 8º Simpósio Brasileiro de Comunicação em Enfermagem; 2002; Ribeirão Preto (SP), Brasil. [citado em 25 abr 2013]. 17:368. Disponível em: URL: http://www.proceedings.scielo.br/pdf/sibracen/n8v2/v2a074.pdf.
9.Bardin L. Análise de conteúdo. Tradução de Luís Antero Reto e Augusto Pinheiro. Lisboa (Por): Edições 70; 2010.
10.Korin D. Novas perspectivas de gênero em saúde. Adolesc Latinoam. 2001; 2:67-79.
11.Gomes R. Sexualidade masculina e saúde do homem: proposta para uma discussão. Ciênc saúde coletiva. 2003; 8:825-29.
12.Araújo MAL, Leitão GCM. Acesso à consulta a portadores de doenças sexualmente transmissíveis: experiências de homens em uma unidade de saúde de Fortaleza, Ceará, Brasil. Cad Saúde Pública. 2005; 21:396-403.
13.Braz MA. A construção da subjetividade masculina e seu impacto sobre a saúde do homem: reflexão bioética sobre justiça distributiva. Ciênc saúde coletiva. 2005; 10:97-104.
14.Figueiredo W. Assistência à saúde dos homens: um desafio para os serviços de atenção primária. Ciênc saúde coletiva. 2005; 10:105-09.
15.Schraiber LB, Gomes R, Couto MT. Homens e saúde na pauta da saúde coletiva. Ciênc saúde coletiva. 2005; 10:7-17.
16.Gomes R, Nascimento EF. A produção do conhecimento da saúde pública sobre a relação homem-saúde:uma revisão bibliográfica. Cad Saúde Pública. 2006; 22:901-11.
17.Borges ALV, Schor N. Homens adolescentes e vida sexual: heterogeneidades nas motivações que cercam a iniciação sexual. Cad Saúde Pública. 2007; 23:225-34.
18.Eyken EBBDV, Moraes CL. Prevalência de fatores de risco para doenças cardiovasculares entre homens de uma população urbana do Sudeste do Brasil. Cad Saúde Pública. 2009; 25:111-23.
19.Brito RS, Santos DLA, Maciel PSO. Olhar masculino acerca do atendimento na Estratégia Saúde da Família. Rev RENE. 2010; 11:135-42.
20.Leite DF, Ferreira IMG, Souza MS, Nunes VS, Castro PR. A influência de um programa de educação na saúde do homem. O Mundo da Saúde. 2010; 34:50-6.
21.Couto MT, Pinheiro TF, Valença O, Machin R, Silva GSN, Gomes R, et al. O homem na atenção primária à saúde: discutindo (in)visibilidade a partir da perspectiva de gênero. Interface – Comunic, Saude, Educ. 2010; 14:257-70.
22.Schraiber LB, Figueiredo WS, Gomes R, Couto MT, Pinheiro TF, Machin R, et al. Necessidades de saúde e masculinidades: atenção primária no cuidado aos homens. Cad Saúde Pública. 2010; 26:961-70.
23.Tannenbaum C, Frank B. Masculinity and health in late life men. Am J Mens Health. 2011; 5:243-54.
24.Springer KW, Mouzon DM. Macho men and preventive health care: implications for older men in different social classes. J Saúde Soc Behav. 2011; 52:212-27.
25.Medrado B, Lyra J, Leão LS, Lima DCL, Santos, B. Homens jovens no contexto do cuidado: leituras a partir da paternidade na adolescência. In: Adorno RCF, Alvarenga AT, Vasconcellos MPC. Jovens, trajetórias, masculinidades e direitos. São Paulo: Edusp; 2005. p. 241-64.
26.Winnett R, Furman R, Enterline M. Men at risk: considering masculinity during hospital-based social work intervention. Soc Work Health Care. 2012; 51:312-26.
27.Pinheiro RS, Viacava F, Travassos C, Brito AS. Gênero, morbidade, acesso e utilização de serviços de saúde no Brasil. Ciênc saúde coletiva. 2002; 7:687-07.
28.Astudillo MNM, Pinzón LAS, Ospina JJ, Grisales A, García JDR. Percepciones sobre el cáncer de próstata en población masculina mayor de 45 años: Santa Rosa de Cabal, 2010. Hacia promoc salud. 2011; 16:147-61.
29.Silva PA, Furtado MS, Guilhon AB, Souza NVDO, David HMSL. A saúde do homem na visão dos enfermeiros de uma unidade básica de saúde. Esc Anna Nery. 2012; 16:561-8.
30.Dominguez B. Saúde do homem: hora de quebrar paradigmas. RADIS comunicação em saúde. 2008; 74:8-9.