RESEARCH ARTICLES
Insertion site and tip position of peripherally inserted central catheter in neonates
Priscila CostaI; Mirella de Paula Souza VizzottoII; Cintia Luiza OliviaIII; Amélia FumikoKimuraIV
INurse.Master of Science in Health. Specialist in Teaching Laboratory of the Department of Maternal-Child and Psychiatric Nursing, in the School of Nursing of the UniversidadedeSãoPaulo (University of SãoPaulo), São Paulo, SP, Brazil. priscila2.costa@usp.br
IIUndergraduate nursing student.School of Nursing,UniversidadedeSãoPaulo (University of SãoPaulo), São Paulo, SP, Brazil.mirella.vizzotto@yahoo.com.br.
IIINurse.Master's student of the Graduate Program of Health Sciences, School of Nursing of the UniversidadedeSãoPaulo. São Paulo, SP, Brazil. cintiaoliva@usp.br
IVNurse. Professor, Doctorate, Department of Maternal-Child and Psychiatric Nursing, in the School of Nursing of the UniversidadedeSãoPaulo(University of SãoPaulo). São Paulo, SP, Brazil. fumiko@usp.br.
ABSTRACT: This is a cross-sectional study with prospective data collection that aimed to verify the association between the insertion site and the positioning of the epicutaneouscatheter tip in neonates. The study was conducted with neonates with an epicutaneous catheter hospitalized in a neonatal intensive care unit of a private hospital in the city of São Paulo, Brazilduring the period of August 31, 2010 to July 01, 2011. The data were collected from the hospital records, by means of an instrument developed for this study. There were 244 epicutaneous catheter inserts analyzed , of which 212 (86.9%) resulted in a central position of the tip. The majority of the catheters were inserted in right hemisphere body (63.5%), in the upper limb (76.2%) and by axillary vein (31.1%). There was no association between the insertion site and the positioning of the tip. It is concluded that the insertion site does not influence the position of the epicutaneous catheter tip in neonates.
Keywords: Newborn, central venous catheterization, neonatal nursing; delay catheters.
INTRODUCTION
The peripherally inserted central catheter (PICC) or epicutaneous catheter brings benefits for high-risk newborns who need safe venous access for a period of more than six days and for infusion of hyperosmolar solutions and vesicant agents1.
In neonates, the PICC can be inserted via peripheral veins located in various segments, however tangible factors such as extension, location and numbers of valves of each vein should be considered, because they can facilitate or hinder their installation.
The extensive and tortuous course veins, with a large number of venous valves, can conduct the distal end of the catheter (tip) to progress to undesired anatomical positions, even when all the recommendations for patient positioning have been adopted and the procedure is performed by experienced and capable nurses in the handling of the device. Therefore, the segment body hemisphere, as well as the vein accessible for insertion of the PICC may influence the initial position of the catheter tip.
For the clinical practice of nurses in neonatal unit becomes relevant fetch evi scientific trends that subsidize the choice of the best insertion site of the PICC.
Based on these considerations, the objective of this study was to verify the association between the insertion site of the PICC and the initial position of its tip. It sought to compare if the groups with central and non-central tip position of the PICC differ with respect to the body hemisphere accessed or vein segment used for installation of the catheter.
LITERATURE REVIEW
The technological advances in neonatal intravenous therapy intensified markedly from the 1980s. Devices for vascular access were specially developed to give therapeutic support to neonates hospitalized in neonatal intensive care units (NICU).
The PICC is a device with central vascular insertion through peripheral veins. For neonates, there are PICC devices available, single or double lumen, made with polyurethane or silicone, with a variable extension between 8 to 75 cm2,3.
To be considered central, the regulatory authorities of health practices4-6 recommend that the distal end of the PICC should be anatomically positioned in the lower third of the superior vena cava near the junction of the superior vena cava in the right atrium. If inserted in lower extremities should have its tip lodged in the upper third of the vena cava below the level of the diaphragm. If the tip of the PICC is lodged on any other anatomic position will be considered as non-central.
The PICC can be inserted in neonates through various veins, namely: basilica, cephalic, median cubital, axillary, temporal, posterior auricular, internal jugular vein, saphenous, femoral and dorsal arches of hands and feet1.
There are advantages and disadvantages involved in the choice of access vein for insertion of the PICC. The blood vessels of first choice for installation of the PICC in newborns (NB) are located in the upper limbs due to ease of access, lower number of venous valve and risk of infection or other complications2. In addition, it is common for the nurses prefer insert the catheter in right hemisphere body, by reason of the greater proximity to the inferior vena cava.
The vein access most recommended for vascular insertion of this device in neonates is the basilica, being that requires lesser extent for progression of the catheter by presenting greater luminal diameter in cubital region.Its path runs along the inner face of the arm and has between 4 and 8 venous valves. The cephalic vein, also located in the upper limbs, presents less luminal diameter, has between 6 and 8 venous valve and its trajectory follows the external face of the arm by bypassing the shoulder, which gives it a path of greater extension until the inferior vena cava and may also increase the risk of phlebitis and bad positioning of the tip of the PICC2,7.
Prior to installation of the catheter, the nurse estimates the length of catheter that will be inserted by measuring the distance between the site of venous puncture to third right intercostal space1. Once the recommended technique for measuring the extent of PICC to be inserted does not differ between the different veins of the same body segment, the tip of the catheter may become lodged with greater frequency in non-central positions.
Because of differences in anatomical characteristics of various veins in each segment and body hemisphere, it is assumed that the site of insertion may influence the tip position of the device.
METHODOLOGY
A cross-sectional study with prospective data collection on hospital medical charts (documentary analysis). The study was conducted in the NICU of a private large hospital, in the southern area of the city of São Paulo, with newborns undergoing the installation of a PICC device, hospitalized in the period August 31, 2010 to July 01, 2011.
In the study neonates without congenital anomalies were included, born in the hospital's maternity unit and submitted to PICC installation, totaling 244 devices, during the period of data collection in the NICU. The neonates were excluded if there was no record regarding the site of insertion and the tip position of the device, variables of interest in this study.
The data were obtained from the hospital records and a form called institutional control of the PICC, in which the nursing team records information regarding the insertion, maintenance and removal of the device.
The institution maintains a protocol for management of PICC based on standards published by professional societies, responsible for training of Brazilian nurses in procedures of insertion, maintenance and removal of this intravascular device.
Initially the newborn is positioned in the supine position with the arm to be puntctured at an angle of 90 in relation to the trunk, the head turned to the side of the ipsilateral limb to be catheterized and the length of the catheter to be inserted is measured.
If the catheter is inserted into an upper body segment, the length of the portion to be inserted will be measured from the puncture site to junction sternal notch right, toward the thrid right intercostal space. If the venous puncture is made in the left upper limb, the measurement of the length of the catheter will extend to the puncture site to junction sternal notch with the head of the right clavicle and the third intercostal space. When inserted through veins of the lower limbs, the measurement of the length of the catheter will be extended from the puncture site to the umbilical region toward the xiphoid process.
After the venous puncture, a complete progression of the PICC inside the vein punctured is made and then the insertion site is occluded with dressing, then performing a radiography to identify the position of the catheter tip.
The thoracic vertebrae and the venous anatomy of the thorax were used as anatomical references for identification of the distal end of the catheter. When the tip of the PICC was lodged next to the 1st thoracic vertebra it was considered in subclavian vein; next the 2nd thoracic vertebra, in brachiocephalic vein; between the 3rd and 4th thoracic vertebra, superior vena cava; between the 5th and 6th thoracic vertebra and/or two vertebrae below the carina, in cavoatrial junction; and below the 7th thoracic vertebra, in the right atrium. The distal end of the catheter at the level of the diaphragm or near the 9th and 10th thoracic vertebra, was considered in the inferior vena cava1,8,9 .
For data collection a form developed for this study was used with the variables of interest in this investigation. The variables of characterization of the population included the clinical diagnosis, postnatal age (days of life), corrected gestational age (weeks) in procedure date, gender and weight.
They comprised the independent variables:
As a dependent variable was considered; if the positioning of the tip of the PICC after insertion of the device - central or non-central:
Taking into account the Resolution no. 196/96 of the National Health Council, the research project has been approved by the Ethics Committee of the hospital (Process no. 238/2010).
The data collected were stored in Microsoft Office Excel spreadsheet l 2007 and analyzed in SAS System software for Windows 9.0.
The quantitative variables were described by means and standard deviation. The study population was divided according to the position of the epicutaneous catheter tip, i.e. a group with the central tip and another with the non-central tip. The comparisons of means between groups were analyzed with the Student t Test. The qualitative dichotomous and polytomous variables were described by absolute and relative frequencies percentage. The association between the insertion site and the initial positioning of the tip of the PICC was analyzed using the Pearson's chi-squared test or Chi-square by Monte Carlo simulation. The adopted level of statistical significance was p < 0.05 with a confidence interval of 95%.
RESULTS AND DISCUSSION
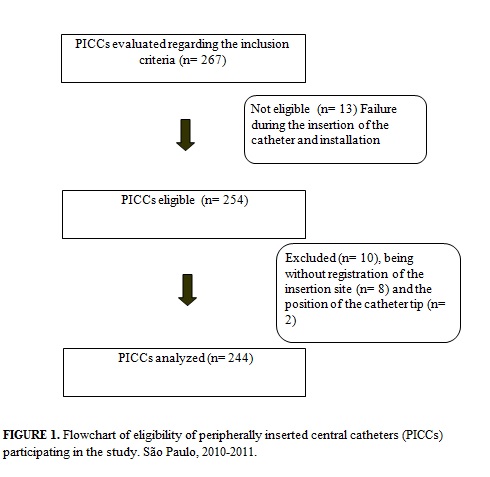
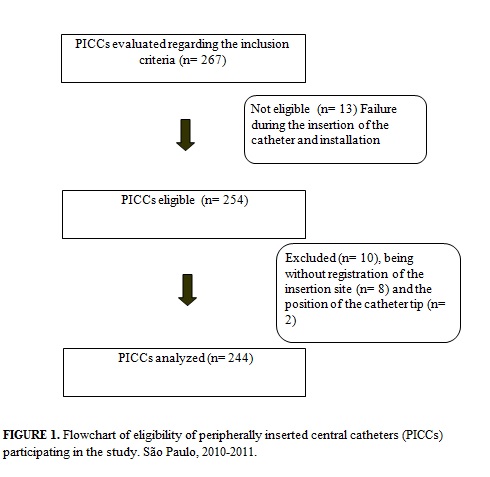
This study evaluated, regarding the eligibility criteria, the set of 267 attempts for PICC insertion in neonates. After exclusion of insertions unregistered in hospital records regarding the insertion site, tip position or unsuccessful, remained 244 PICCs for analysis, as shown in Figure 1.
The 244 PICCswere installed in 201 newborns and the frequency with which each newborn was submitted to installation of the catheter ranged from one to five. The majority of infants, 163 (81.1% ), were subjected to only one procedure.
From the244 epicutaneous catheters inserted, 212 (86.9%) were positioned centrally and 32 (13.1%) non-centrally. Catheter tips located in the superior vena cava were observed in 159 (75%) insertions, followed by the inferior vena cava - 26 (12.3%) insertions, cavoatrial junction - 15 (7%) insertions and right atrium - 12 (5.7%) catheters. Among the non-central catheters, the most common anatomic position was the subclavian vein - 23 (71.9%) catheters, followed by the iliac vein - 6 (18.7%) and axillary - 3 (9.4%) catheters.
A prospective cohort study conducted in a NICU at a hospital in Saudi Arabia evaluated 47 PICCs inserted in 41 neonates and found similar results. Catheters in central position were recorded in 87.2% procedures and only 12.8% of PICC inserted had its tip housed in internal jugular vein, subclavian or submental10.
In both studies the frequency of epicutaneous catheters inserted in center position approached the 90% which indicates lower risk of complications and greater likelihood of catheter maintenance until the completion of intravenous therapy.
The studied population was predominant of males, 144 (59%), without statistical difference between the groups with catheter in a central position and non-central (p=0.96).
The most frequent clinical diagnoses were prematurity in 193 (79.1%) insertions, early respiratory distress in 165 (67.6%) insertions, twinning in 57 (23.4%) insertions, sepsis in 54 (22.1%) insertions, heart disease in 43 (17.6%) insertions and disorders of the gastrointestinal tract in 36 (14.8%) catheter inserted. There was no statistically significant difference among neonates with the central epicutaneous catheter tip and those with the non-central catheter tip, except for the diagnosis of heart disease, being proportionately more frequent among infants with non-central catheters (p=0.03).
The results were similar to a descriptive retrospective study that evaluated the insertion of 239 epicutaneous catheters in 191 newborns admitted to a NICU of a public hospital in Rio de Janeiro and found that the early respiratory distress was evident as the primary pathology associated with the use of the catheter11.
Since preterm newborn infants represent the main population admitted in the NICU, clinical diagnoses corroborate the main indications for insertion of PICC which include treating infections requiring intravenous antimicrobial therapy, gastrointestinal disorders, respiratory diseases and cardiac congenitalities1.
It was observed in the studied population had an average gestational age of 34 weeks, chronological age greater than 10 days of life and average weight greater than 1900g, with no statistically significant difference between the groups with the central and non-central PICC tip, as shown in Table 1.

It has been demonstrated that one of the main indications for epicutaneous catheter in newborns is prematurity. This finding corroborates the founds of a prospective cross-sectional study carried out in a NICU at a large public hospital of Sao Paulo that aimed to identify the initial positioning of the PICC tipin 37 newborns. The majority of the neonates evaluated was male (59.4%), with corrected gestational age of 32.2 weeks, average weight of 1.289G and postnatal age of 4.3 days of life12.
For the insertion of the PICC, the administration of analgesics or sedatives was verified in 79 (32.4%) catheter installations and there was no difference with respect to their occurrence among the PICCs with central and non-central location (p= 0.79). The most commonly used sedative was midazolam in 45 (18.4%) insertions, and the most commonly used analgesic was fentanyl citrate in 14 (5.7%)PICC insertions.
Inferior results were found in a descriptive exploratory study with a sample of 43 newborns in a neonatal unit of a hospital in the city of São Paulo, that aimed to investigate the use of pharmacological and non-pharmacological analgesic during PICC insertion in neonates. The results showed a frequency of 86.0% of the PICC insertions without analgesia and in 13.9% there was only sedative employment. The results showed no record of adoption of non-pharmacologic analgesic and stress relief methods during the catheter installation13.
Health professionals, including nurses, tend to underestimate pain in children, and the adoption of pain control measures is sporadic. The rationale for adopting this approach is guided on the argument that the use of analgesics, especially opioids cause physical and psychological dependence and respiratory depression14.
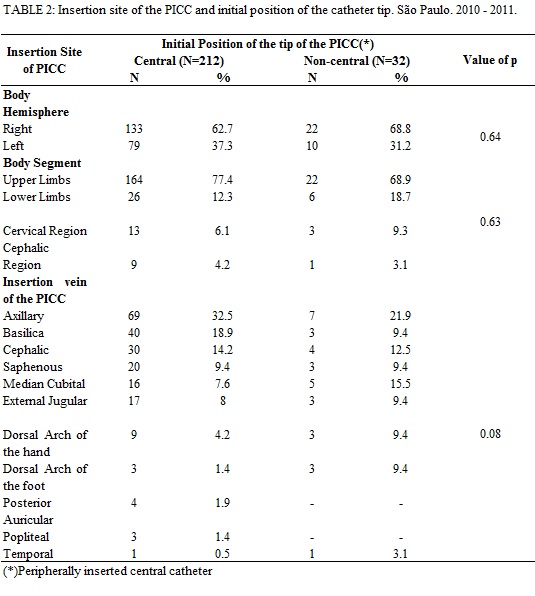
Regardingthe epicutaneous catheter insertion site, it was found that the body hemisphere most commonly used for installing the catheter was the right - 155 (63.5%), most often on the upper limb - 186 (76.2%) and axillary vein in 76 (31.1%) procedures, in accordance with Table 2. There was no statistically significant difference found between the insertion site (hemisphere, body segment and vein accessed) and the initial position of the tip of the PICC.
Different results were found in a retrospective study conducted in a NICU at a hospital in Turkey that evaluated 40 inserted PICCs. Themost frequently vein was the great saphenous vein (85%) and most frequent body hemisphere for catheter installation was the left (53%)15.
In this study, the axillary vein was the one that presented the highest frequency of access for inserting the PICC. This result differs from the findings in the literature and their choice may have elapsed in reason of the amplitude of the diameter of the vein that makes it technically easier to perform the venipuncture and progress the catheter until the superior vena cava.The axillary vein can allow the use PICC with a larger-diameter and a greater number of lumens. This vein has the disadvantage of difficulty of its visualization in older children because of its greater depth and presence of adjacent subcutaneous tissue. Another disadvantage of its use is its proximity to the axillary artery, which increases the risk of arterial puncture1.
However, 31.5% of the device insertions were performed by the basilica and cephalic veins, which have fewer valves, larger caliber, favorable anatomy and ease in dressing changes.
A descriptive study, retrospective and documentary with 125 newborns, which aimed to describe the use of PICC in a NICU of a private hospital in Santa Catarina, showed that the veins of access for inserting the PICC were the basilica (23.8%), the cephalic (19.4%), posterior auricular (18.2%), external jugular (13.6%), axillary (12.5%), median cubital (6.8%) and great saphenous vein (5.7%). The tip of the catheter was centrally lodged in 98.9% of the procedures3.
In the present study, the 43 catheters inserted through the basilic vein, 3 (7%) had their tips lodged in a non-central position. Of the 34 catheters inserted into the cephalic vein, 4 (11.8%) was non centrally allocated. The most common anatomic position of the PICC tipnon-centrally located, from cephalic vein and the basilic vein, was the subclavian vein, 75%.
Discordant findings in the literature indicate that catheters inserted in the basilic vein may have their tip poorly positioned in internal jugular vein and those entered through the cephalic vein may have its tip in axillary and basilica veins1.
In catheters inserted through the lower limbs, the saphenous vein was the most accessed, then the veins of the dorsal foot arches and the popliteal. For the inserts in the cervical region, the external jugular vein was used on all the inserts. Among the 20 insertions performed in jugular veins, 3 (15 %) resulted in non-central catheter tip, settling in the subclavian vein.
In this research, the only variable that showed to have influence in the initial position of the catheter tip was the presence of difficulty for progression of the catheter (p= 0.001). The results reveal its occurrence in 63 (25.8%) PICC insertions. There was record of difficulty for progression of the catheter in 16 (50.0%) of intravenous devices inserted that had the initial position of its tip hosted non-centrally and only 47 (22.2%) in central tip catheters.
The venous valves because they represent obstacles to the advancement of the catheter, as well as the presence of excessive bleeding and aberrant venous anatomy, can contribute to make the catheter follow other ramifications, leading it to non-central positions. In this situation it may be necessary that the nurse perform repositioning maneuvers of the neonate's limbs, catheter traction and new attempt for progression, besides instillation of saline solution to stimulate the opening of venous valve and progression of the tip of the device during the installation of the catheter1.
CONCLUSION
The methodology used was appropriate for the proposed objective. Its reproduction allows conducting research of the same type in other neonatal units. The results of this study have brought elements for reflection and discussion of the practices of nurses regarding the choice of the site of PICC insertion in neonates.
In the population studied, the choice of the site of thePICC insertion did not influence the initial position of the catheter tip. However, there was a higher proportion of non-central catheters among individuals with heart disease or any condition that presented difficulties for intravenous progression. It is recommended to investigate other factors that may affect the positioning of the distal extremity of this device.
However,it is noteworthy that the findings of this study should be analyzed within the constraints, especially because the sample size of non-central catheters was small when compared tocentral catheters, and also owning to the decision making of the nursing team regarding the sites of PICC insertion.
REFERENCES
1. Pettit J, Wyckoff MM. Peripherally inserted central catheters: guideline for practice. 2nd ed. Glenview: National Association of Neonatal Nurses; [diretrizna internet]. 2007 [cited 2011 Jan 15]. Available at: http://www.nann.org/pdf/PICCGuidelines.pdf.
2.Freitas EM, Nunes AB.The nurse in the practice of peripherally inserted central catheter in neonatal care. Rev Min Enferm.2009;13:215-224.
3. Baggio MA, Bazzi FCS, Bilibio CAC. Peripherally inserted central catheter: description of its use in neonatal and pediatric ICU.Rev Gaúha Enferm.2010; 31:70-6.
4. Infusion Nurses Society. Infusion nursing standards of practice. J IntravenNurs. 2011;34(1 Supl 1S):S1-S110.
5. Food and Drug Administration Task Force. Precautions necessary with central venous catheters. FDA Drug Bull.1989:15-16.
6. National Association of Vascular Access Networks (NAVAN). Tip location of peripherally inserted central catheters. J Vasc Access Devices. 1998;3:8-10.
7. Paulson PR, Miller KM. Neonatal peripherally inserted central catheters: recomendations for prevention of insertion and postinsertion complications. J Neonatal Nurs. 2008;27:244-57
8. Mahlon MA, Yoon HC. CT Angiography of the superior vena cava: normative values and implications for central venous catheter position. J VascIntervRadiol. 2007;18:1106-10.
9. Yoon SZ, Shin JH, Hahn S, Oh AY, Kim HS, Kim SD et al. Usefulness of the carina as a radiographic landmark for central venous catheter placement in paediatric patients. Br J Anaesth. 2005;95:514-7.
10. Tawil KA, Eldemerdash A, Hathlol KA, Laimoun BA. Peripherally inserted central venous catheters in newborn infants: malpositioning and spontaneous correction of catheter tips. Am J Perinatol. 2006;23:37-41.
11. Reis AT, Santos SB, Barreto JM, Silva GRG.Peripherally inserted central catheter use in neonatal clients at a public state hospital: retrospective study. Rev enferm UERJ. 2011;19:592-7.
12. Camargo PP, Kimura AF, Toma E, Tsunechiro MA. Initial peripherally inserted central catheter tip position in neonates. Revescenferm USP. 2008;42:723-8.
13. Oliveira MBP, Oliveira DP, Leventhal LC.Pharmacological and non-pharmacological interventions used by nurses to pass peripherally inserted central catheter in a neonatal unit. Rev dor.2009;10:241-5.
14. Rossato LM, Magaldi FM. Multidimensional tools: application of pain quality cards in children. Rev Latino-Am Enfermagem. 2006;14:702-7.
15. Uygun I, Okur MH, Otcu S, Ozturk H. Peripherally inserted central catheters in the neonatal period. Acta Cir Bras. 2011; 26:404-11.